
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Research Article(ISSN: 2690-5760) 
The Specifics of the Deficit of Social Cognition in Old Age and Ways of Rehabilitation Volume 4 - Issue 4
AI Melehin*
- Associate Professor, Clinical Psychologist, PA Stolypin Humanitarian Institute, Russia
Received:June 10, 2022; Published: June 28, 2022
Corresponding author: AI Melehin PhD, Associate professor, clinical psychologist of the highest qualification category. P.A. Stolypin Humanitarian Institute, Moscow, Russia
DOI: 10.32474/JCCM.2022.04.000194
Abstract
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
The article, based on foreign and own research over the past 5 years, has shown the specificity and prognostic significance of changes in social cognition during normal aging. A model of the influence of changes in social cognition on the functional status of an elderly and senile person is presented M.F. Green, W. P. Horan. The specifics of socio-cognitive deficits in late-life neurocognitive disorders, as well as mental disorders according to DSM-V. are detailed. The concepts of «social cognition», «mentalization», «theory of mind» is differentiated. The trajectory of changes in the «emotional» and «cognitive» components of the mental model in normal aging is shown. Rehabilitation drug and psychological ways (multimodal cognitive behavioral therapy, mentalization therapy, metacognitive therapy) to minimize the deficit in social cognition in old age are described. In routine gerontological (geronto psychiatric) practice to this day, more attention is paid to the state of neurocognitive functioning («neuro-cognitive abilities»), while «age-specific» features of socio-cognitive functions («socio-cognitive skills»/abilities) or social cognition, which provide the process of perception, interpretation of «mental» states and intentions of other people, are not sufficiently considered. They are crucial for effective interpersonal functioning, therapeutic alliance, and resocialization [1], minimizing conflicts and providing social support [2].
Introduction
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
Aging is associated with a decrease in both the «cognitive» and «affective» components of the «theory of mind» (metallization, reading «mental» state [3]). This discovery highlights the importance of evaluating the functioning of the «mental» model in contextual social situations representative of life, where decoding and reasoning processes act together with other cognitive functions, such as episodic memory, social knowledge, and related processes, in accordance with several models of the functioning of social cognition [4]. The concept of socio-cognitive aging has appeared in foreign psychology («social-cognitive aging»). To determine sociocognitive changes (Figure 1), an assessment of the ability to build a theory of mind, empathy, social perception and behavior is carried out [5].
Changes in the ability to understand «mental» states are a key factor, a cognitive-behavioral phenotype not only of several mental and neurological disorders [6-13], but can also occur with «normal» development («healthy aging») [1,14-23] «Productive» (successful) aging is largely connected to the existence of social capital (more precisely, «mental resources»): social circle, a person to confide in, emotional support, social interactions, significant social activities. Social capital as a component of mental resources acts as an everyday stress «buffer», helps decrease uncertainty in the elderly. Having emotional support in elderly years plays an important role in maintaining somatic and mental health. If a person with Alzheimer, Parkinson has somebody to confide in, the risks of dysfunctions decline as well as a drop in suicidal tendencies can be seen [10,24]. Absence of emotional support in elderly is closely related to high risks of heart failure complications, after suffering a stroke or undergoing surgical operations [15].
Aging brings about changes in social interactions and the intrinsic emotional circumstances around them. An elderly starts showing selective motivation towards different forms of social activities. They arbitrarily structure their social network focusing on trustworthy relationships and shielding themselves from «negative» and traumatic experiences [22]. Our foreign colleague Laura Carstensen has proposed the Socio-emotional Selectivity Theory [25]. She assumed that it is not the chronological changes that lie at the base of the alterations in selecting and structuring social contacts but rather awareness of time. Elderly perceived future time, which in turn brings a massive shift in goals - from «cognitive» to «emotional». Despite the narrow socio-emotional selectiveness, the elderly interacts with other people and confronts situations which require understanding of intentions, truthfulness, beliefs, and emotions of other people - in other words, where it is necessary to «read» hidden and indirectly implied «mental» states of other people. The ability to perceive and subconsciously understand psychological states (for example, thoughts, feelings, beliefs, intentions, desires, emotions) of «Self» of the «Other», to explain or predict the behavior and build effective communication is called the theory of mind (To M):
a) Metacognitive ability that provides understanding of mental states: emotions of intentions, false beliefs, feelings, thoughts of one’s own and other people.
b) This ability allows you to build a cognitive model of mental state, relationships and predict possible behavior.
c) Underlies the understanding of non-literal statements: humor, sarcasm, irony of deception.
d) Changes in social cognition/ theory of mind) in elderly patients.
e) Trajectories of wakefulness (life satisfaction, loneliness).
f) Social competence; social support (lack of interpersonal relations) and social relations (social capital).
g) Social quality of life.
h) Cooperative behavior.
i) Emotional regulation: the level of mutual rejection, aggressive behavior.
j) High empathic distress.
k) Vulnerability to social exploitation and fraud.
Changes in the theory of mind of a geriatric patient are risks [23]:
a) Become a victim of social exploitation and fraud.
b) Commit a crime or an illegal act yourself.
c) High family stress.
d) Empathic distress. Difficulties in establishing friendships.
e) Difficulties of the therapeutic alliance of patient and doctor.
These difficulties may relate to the growth of vulnerabilities in the ToM, which influence socioemotional functioning (Figure 2) [13].
Figure 2: A model of the influence of social cognition on the neurocognitive and functional status of a geriatric patient (M.F. Green, W. P. Horan).
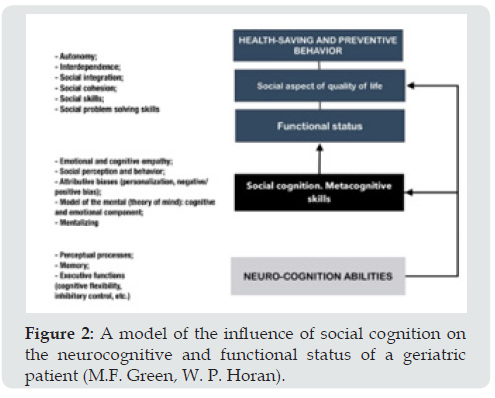
The level of life of the elderly hugely depends on socioemotional functioning – expressing personal feelings and thoughts to the «Other», being able to interpret thoughts and feeling of the Other, showing empathy, effectively managing proper emotions, building the right communication strategies adequate for given social circumstances. Ability to understand mental states in elderly makes a considerable contribution to social life. There are differences in the behavioral models of elderly and senile people. According to various sources, changes in the ToM are starting to show from 55-60(65) years [3]. An elderly can start having difficulties understanding other people «mental» states, motivations, and needs. Elderly people often misinterpret psychological states of unknown people, they find it harder to appreciate untrustworthy people, they tend to trust strangers and, therefore, they fall victims to swindlers more often. The disconnection between one’s own ideas and other people ideas may affect self-help in decision making, lead to «misunderstanding», conflict escalation and violation of social interactions, which furthers the growth of «psycho-sociological problems» and leads to social isolation [26]. Those difficulties may lead to a decrease in social activity, estrangement from significant people which results in feelings of increased loneliness, and being shunned, increases the risk of developing a range of somatic and psychological disorders with further deterioration of health possibly leading to disability [16]. Therefore, the estimation of the presence and deficit of theory of mind in elderly is a «fundamental» diagnostic criterion with the aim to effectively treat and rehabilitate.
For instance, the American psychiatric association (APA) included deficit of theory om mind as one of the criteria for diagnosing neurocognitive disorders in DSM-V [2]. Now, these changes are a transdiagnostic problem, because they represent a recognized area of disorders with functional and clinical significance [8]. Previously, the assessment of socio-cognitive functioning was usually mentioned only in the diagnosis of personality disorders in DSM-IV [27], (Figure 3). The concept of socio-cognitive screening has appeared in the DSM-V, which makes it possible to improve the early diagnosis of the following neurodegenerative disorders: behavioral variant of frontotemporal dementia, Alzheimer disease, amyotrophic lateral sclerosis. In this classification, one of the 6 diagnostic components for determining the severity of neurocognitive disorders, as well as the differentiation of their subtypes, is the assessment of the following components of social cognition: recognition and differentiation of emotions by face; a model of mental, ability to «emotional» and «cognitive» empathy. The integrative model of the onset of depression (stress–reward– mentalizing model of depression), considering the RDoc approach (BehaviorPhysiological MechanismGenetic Features) [5].
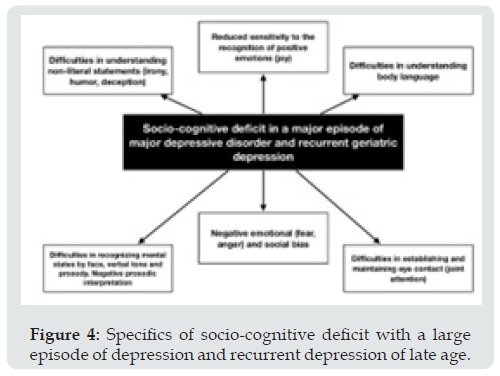
Late-life depression is the result of interacting disorders in the system of response to stressful events, which leads to problems in the system of internal reinforcement (reward), especially on the part of attachment/autonomy, as well as problems understanding mental states. In the elderly and senile age, the presence of everyday stress often leads to the inability to overestimate and regulate negative affect, which leads to reward deficit syndrome, refusal of controlled use of the mental model with a predominance of «hypo»- or «hyper» mentalization. This automatic, emotionally biased construction of models of mental states of other people, based on unreflexively assumptions about oneself and others, leads to a state of subclinical depression, which prevents successful aging. Disorders in the «mental model» in (sub)depressions and more «severe» forms of depression are observed from the perception of facial emotions, facial memory, understanding of deception, irony. The severity and duration of depressive episodes increases the deficit of the mental model, as well as vice versa [12]. Sociocognitive deficit is observed with a «large» episode and recurrent depression (Figure 4).
Figure 4: Specifics of socio-cognitive deficit with a large episode of depression and recurrent depression of late age.
Changes in social cognition are associated with functional status (daily, personal, and instrumental activity). Compared with an isolated focus on improving cognitive functions, enhanced social cognition is an effective predictor of recovery after a «severe» traumatic brain injury. The desire to perceive and use socioemotional information reduces age-related memory deficit [28]. Recommended to evaluate socio-cognitive functions in a geriatric patient when
a) Mood disorders (unipolar major depression, bipolar disorder)
b) Anxiety spectrum disorders
c) Late-life psychoses
d) Personality disorders
e) Somatoform disorder (with pain syndrome)
f) PTSD
g) MCI
h) Neurodegenerative disorders
i) TBI.
Differences Between «Theory of Mind» and «Social Cognition»
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
Theory of mind is a system of conceptualization of knowledge about the «mental» state of self and others which allows analyzing the person «inner» life. Understanding proper «mental» state as well as that of «the Other» is the basis of social cognition, social interaction. Table 1 outlines the key differences between ToM and social cognition [22,24]. Theory of mind permits to disclose «cognitive» mechanisms of understanding in interpersonal interactions because the process of socializing is based on constant monitoring and comparison of «mental» states and events. A person needs to interpret and foresee «mental» states of the other person. In this case, while examining the theory of mind and the « mental mechanism» of social cognition it is necessary to point out that it is aimed at studying the «inner» psychological states of the other person. The attention is focused on the individual conceptual world of a person. ToM is comprised of the following components (Table 1) [13]:
a. «Cognitive» component tom: the ability to recognize beliefs, false opinions, thoughts, deception or irony, cognitive component of empathy. It provides the skills needed for manipulating and deceiving the interlocutor or irony regarding a person or situation.
b. «Emotional» component tom: the ability to recognize and understand emotions and feeling of another person. It plays a role in prosocial behavior, ability to console the «other» and help solve a problem, the emotional component of empathy.
c. «Conative» tom belongs to the forms of social communication when one person is trying to influence the mental and emotional state of the other person.
Theory of Mind in Elderly
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
Studies of the ToM in elderly indicate deficit of this ability. However, it is not enough to speak of the «deficit of the ToM» in elderly, it is necessary to take into consideration some compensatory mechanisms: «crystallized» intelligence, emotional intelligence, and the skills of interpersonal understanding [18-22,24]. On the other hand, the changes in the theory of mind happen heterogeneously: there are different trajectories and dynamics of transformations of the «affective» and «cognitive» components in the elderly [11]. The problems of the ToM are not total/absolute; they are selective [23]. For example, elderly with Alzheimer can recognize other people emotions; however, they have difficulties in recognizing false beliefs [22]. Regular everyday socializing at elderly age is connected to the cognitive component of the theory of mind [2]. At elderly age the «cognitive» component ToM is mostly affected by changes [30]. This can be explained from different perspectives. For instance, at elderly avoid dangerous, negative social interactions due to the fear of being deceived [4]. The «affective» component at elderly age stays intact longer thanks to the preservation of various life interests and hobbies [116]. Our colleagues L. Bottirolia and E.A. Cavallini showed that there is a divergent trajectory in decline of the «affective» and «cognitive» components of the ToM, with aging «affecting» the «cognitive» component more than the affective one [1]. This research is interesting because it gives the possibility to compare the dynamics of changes in the ability to rationalize and the ability to recognize, understand emotions. Nonetheless, most of the studies of the ToM in elderly focus on either the «cognitive» or the «affective» component which often leads to contradictions [31].
«Cognitive» Component Theory of Mind in Elderly
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
Elderly demonstrates an evident priority in perception of social and emotional information [25]. Research has shown traces of decrease of the «cognitive» component in elderly years while solving tasks on identification, double bluff, irony, deception, «complex» false beliefs [4,12]. Other studies show absence of age-specific differences in the cognitive component of the ToM with the tasks related to understanding false beliefs of the first category where only one perspective of a character should be understood. Our colleagues S. Bottorilia and E.А. Cavallini carried out an estimate of the «cognitive» component of the ToM using a test detecting tactlessness on elderly [Bottirolia1]. Our studies have made it evident that elderly (55-60) detect deception and irony in narrative stories better than the senile (60-74 and 75-90). An elderly person uses their understanding of false beliefs and deception about the mental state through their personal experience to construct an appropriate paradigmatic interpretation of the situation. Our research has shown that in senile (76-90 years) compared with the elderly (55-60 and 61-74 years old), there are changes in the ability to make pragmatic interpretations, there are no difficulties in understanding the social situation and the ability to draw conclusions about the false opinions of only one person. In the elderly (60-76 years old) and senile (74-89/90 years old), there are difficulties in understanding what one person thinks about the intentions, beliefs of another person («second-order» representations). The phenomenon of emotional-egocentric shift is traced [20,22,24].
«Emotional» Component Theory of Mind in Elderly
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
According to some studies the emotional component in elderly remains [1,10]. Our colleagues S. Battirolia and E. Cavallini demonstrated that while doing tasks on emotion recognition elderly people make less mistakes than the young ones [1]. However, some scholars [Henry, Phillips, Ruffman, 2013] reckon that there are difficulties in emotional recognition and differentiation [Slessor, Phillips, 2007], especially for «complex» emotions [Ruffman, Henry, 2008]. Our studies have proved that by senile (75-90 years) the ability to recognize emotions from people faces decreases. Recognition of negative emotions (fear, anger) suffers more than that of neutral and positive (happiness). Presence and the level of cognitive deficit, depression in elderly effect interpretations of emotions by their expression [19,21]. Thus, our research has shown that more errors in recognizing emotions by face are observed in senile (75-90 years old), as opposed to elderly (55-60/61-74 years old). Drastic changes in this component begin at the age of 60.
There is a phenomenon of «positive cognitive bias». The greatest difficulties are observed when assessing negative emotions (anger, fear, and sadness). The emotion of joy is better differentiated by intensity than sadness. Changes in the differentiation of negative and even positive emotions begin at the age of 65, increasing at 76- 90 years [21,22,24] Figure 5.
Factors Influencing the Theory of Mind in Elderly
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
a) Neuroanatomical factors. Aging relates to nonlinear decline in gray matter, changes in gray matter. Decline in gray matter influences the performance of the cognitive functions [14]. In «normal» aging decreases the volume of premotor cortex, gyrus frontalis inferior, insula and gyrus temporalis superior. A reduction in connections between lobus frontalis telencephali and ltemporalis occurs. Aging brings about natural changes in dorsolateral prefrontal cortex which plays a significant role in securing understanding of the mental state of the other person («cognitive» component) and at the same time ventromedial prefrontal cortex takes part in understanding feeling/emotions of other people («affective» component) [30]. Patients with ventromedial prefrontal cortex injuries show changes in the «affective» component, whereas dorsolateral prefrontal cortex injuries lead to changes in the «cognitive» component. Changes in dorsolateral area occur more often than in the ventromedial. Nonetheless, there are compensatory neuronal mechanisms which reduce «age-specific» cerebral changes. Activation of some of the neural areas may help maintaining understanding «mental» states. For example, bilateral language areas [11,17,32].
b) Somatic factors (Comorbid physical conditions). Our foreign colleagues have shown cardio-vascular diseases with comorbidly burdeness make a significant impact on cognitive functions. Pronounced degrees of heart failure cause difficulties in understanding emotions and recognizing «mental» states of other people [3,15,18].
c) Cognitive factors (neurocognitive factors). Various trajectories of changes of development of cognitive processes can be observed while aging. For example, self-regulation, emotional functioning stays intact and may even improve in elderly, which proves the socio-emotional selectivity theory [1]. Understanding «mental» states requires participation of the cognitive processes (working memory, episodic memory, cognition, speech) [11]. Executive functions are the predictor of the theory of mind [33], consist of inhibitory control, working memory, changes of the attention target and verbal fluency. The processes of «braking» control and renovation/restoration of the working memory are more vulnerable in elderly, and they have an impact on securing the «cognitive» component theory of mind [4].
d) Psychosociological factors. The efficiency of understanding of mental states of self and the other in elderly is influenced by perception of the future (features of the time perspective), feeling of loneliness, social avoidance, and presence of support [28]. Decline in the number of interactions, detachment may be a factor that influences the decrease in the «cognitive» and not the «affective» component in understanding «mental» state of the others [24]. Even if an elderly is socially active, they are involved in social exchange with a close circle of people [21]. If an elderly has regular social interactions with new people, they develop their communication skills and this in turn has a positive influence on the «cognitive» component ToM. Elderly suffering from depression, anxiety, grief experience difficulties in understanding «mental» states of self and the others. Study showed that depression in elderly affects the ability to understand reason-and-cause social connections («causal connection»), verbally express emotional states («psychological lexicon»). Elderly with a major depressive episode experience serious difficulties in understanding mental state, recognizing deception and irony [1].
Ways of Improving the Theory of Mind in Elderly
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
There are studies on the effectiveness of various correctional approaches to improve social cognition at a later age, systematized by us in Table 2. It should be noted that now the evaluation of the effectiveness of the drug interventions and brain stimulation methods listed in the table is at the stage of clinical studies. The gold rehabilitation standard for the deficiency of the ToM at a late age is a systematic cognitive-behavioral approach, which includes neuropsychological and metacognitive trainings; formation and strengthening of existing socio-cognitive skills and regulation of emotional state based on internal and external resources; psychoeducation for an elderly person and his relatives. The therapeutic tactics of minimizing the deficit of the ToM (C.J. Harmer) are presented in Figure 6 [10].
Figure 6: Combined tactics to minimize the deficit of the social cognition (according to C.J. Harmer, 2018).
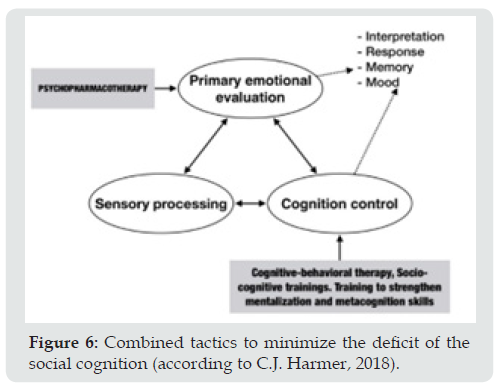
a) Multimodal cognitive behavioral psychotherapy (cognitive behavioral intervention with theory of mind; cognitive enhancement therapy). Cognitive bias modification protocol (CBM). The form of psychotherapy is aimed at minimizing the symptoms of geriatric depression, chronic insomnia, and improving the cognitive and emotional components of the mental model. Psychotherapeutic interaction is based on a therapeutic union between a patient and a clinical psychologist based on empathic understanding. Alexithymia in geriatric depression and many other late-life psychopathologies can have a negative impact on therapeutic relationships and likely therapeutic outcomes. Regardless of alexithymia, geriatric patients with depression tend to show difficulties in empathic judgments when suppression of related emotional states is required. This seems especially important because in everyday social interactions, the emotional states of the «I» and the «Other» rarely coincide. Thus, these difficulties can be associated with a depressive state, and corrected with the help of psychotherapy.
b) Metacognitive psychotherapy. Changes in metacognitive functions in the form of socio-emotional selectivity in perception, interpretation and response to emotional information should be considered when constructing individual protocols of metacognitive psychotherapy for late-life depression, anxiety spectrum disorders and chronic insomnia of a geriatric patient. This form of psychotherapy shifts the focus from result-oriented (actions to reduce stress) to process-oriented (I drew(a) attention, I stressed (a), I can use) the approach. The traditional cognitive behavioral model of mental disorders looks like A-B-C, and in the metacognitive approach it is replaced by A-B-M-C, in which A is a trigger mechanism (trigger) leading to maladaptive emotions and patterns of behavior (C), B is negative automatic thoughts/beliefs, and M- metacognitive processes (the ability to notice changes and compensate for them). The obtained data are recommended to be used in metacognitive training aimed at using effective behavioral techniques to minimize the risks of victimization, i.e., become a victim of scammers.
c) Socio-cognitive training to improve the understanding of mental states and deception S. Bottiroli et al. -it is aimed at overcoming the emotional-egocentric shift, recognizing warning signs and flexible avoidance of undesirable behavior. Considering the mental characteristics of another person in complex, dynamic social situations (double bluff, «misunderstanding», blackmail).
Resume
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
a. The state of social cognition in a geriatric patient is an indicator of the course of aging, mental well-being, and satisfaction with the quality of life. An indicator of the available potential for social adaptation, regardless of vulnerabilities and psychopathological diathesis. Effective rehabilitation after stroke, severe traumatic brain injury depends on the restoration of sociocognitive abilities.
b. Lack of social cognition is not a manifestation of normal aging. The common components that determine the deficit of the pragmatic function of speech at a late age include changes in emotional self-efficacy, social communication during discourse, in the control of behavior in the process of communication, in the selfregulation of mental state.
c. At a late age, the following symptoms of changes in the processing of emotional information were observed: changes in response time; an increase in the frequency of errors in emotion recognition (anger, sadness, and fear); false attribution, negative perceptual bias or the effect of mood congruence (sadness, fear); difficulties in recognizing emotions at low intensity, the effect of a high threshold of emotion intensity. There is a spectrum of compensatory strategies.
d. At a later age, secondary, diffuse, deficiency of social cognition is more often observed due to the prevalence of affective spectrum disorders; cardiovascular disorders; traumatic brain injuries due to falls; moderate cognitive impairment and neurodegenerative diseases. These disorders have a progressive course.
e. Changes in social cognition, is the main cognitive phenotype of many neurological and mental disorders of late age, in this regard, when examining a geriatric patient, attention should be paid not only to cognitive, emotional status, but also to the state of social cognition, to identify the index of socio-cognitive functioning.
References
- Abstract
- Introduction
- Differences Between «Theory of Mind» and «Social Cognition»
- Theory of Mind in Elderly
- «Cognitive» Component Theory of Mind in Elderly
- «Emotional» Component Theory of Mind in Elderly
- Factors Influencing the Theory of Mind in Elderly
- Ways of Improving the Theory of Mind in Elderly
- Resume
- References
- Bottirolia S, Cavallini E, Irene Ceccato, Tomaso Vecchi, Serena Lecce (2016) Theory of Mind in aging: Comparing cognitive and affective components in the faux pa’s test. Archives of Gerontology and Geriatrics 62(1): 152-162.
- Dernt B, Habel U (2011) Deficits in social cognition: a marker for psychiatric disorders? Eur Arch Psychiatry Clin Neurosci 261(2): 145-149.
- Henry JD, Phillips LH, Ruffman T, Phoebe E Bailey (2013) A meta-analytic review of age differences in theory of mind. Psychology and Aging 28(3): 1-16.
- Phillips LH, Bull R, Roy Allen, Pauline Insch, Kirsty Burr, et al. (2011) Lifespan aging and belief reasoning: influences of executive function and social cue decoding. Cognition 120(2): 236-247.
- Rosi A, Cavallinia E, Sara Bottiroli, Federica Bianco, Serena Lecce (2016) Promoting theory of mind in older adults: does age play a role?. Aging Ment Health 20(1): 22-28.
- Cаnnuscio C, Block J,Ichiro Kawachi (2003) Social capital and successful aging: the role of senior housing. Ann Intern Med 139(5 Pt 2): 395-399.
- Dernt B, Habel U (2011) Deficits in social cognition: a marker for psychiatric disorders? Eur Arch Psychiatry Clin Neurosci 261(2): S145-149.
- Henry JD, von Hippel W, Pascal Molenberghs, Teresa Lee, Perminder S Sachdev (2016) Clinical assessment of social cognitive function in neurological disorders. Nat Rev Neurol 12(1): 28-39.
- Monetta L, Grindrod CM, Marc D Pell (2009) Irony comprehension and theory of mind deficits in patients with Parkinson’s disease. Cortex 45(8): 972-981.
- Poletti M, Enrici I, M Adenzato (2012) Cognitive and affective Theory of Mind in neurodegenerative diseases: neuropsychological, neuroanatomical and neurochemical levels. Neuroscience & Biobehavioral Reviews 36(9): 2147-2164.
- Rakoczy H, Harder Kasten A, Lioba Sturm (2012) The decline of theory of mind in old age is mediated by developmental changes in domain-general abilities. British Journal of Psychology 103(1): 58-72.
- Ruffman T, Henry JD, Vicki Livingstone, Louise H Phillips (2008) A meta-analytic review of emotion recognition and aging: Implications for neuropsychological models of aging. Neuroscience & Biobehavioral Reviews 32(4): 863-881.
- Shamay Tsoory SG, Shur S, Liat Barcai Goodman, S Medlovich, Hagay Harari, et al. (2007) Dissociation of cognitive from affective components of theory of mind in schizophrenia. Psychiatry Research 149(1-3): 11-23.
- Castelli I, Baglio F, Valeria Blasi, Margherita Alberoni, Andrea Falini, et al. (2010) Effects of aging on mindreading ability through the eyes: an fMRI study. Neuropsychologia 48(1): 2586-2594.
- Drewelies J, Gerstorf D (2020) Cognition and well-being across adulthood and old age. In AK Thomas, A Gutchess (Eds), The Cambridge handbook of cognitive aging: A life course perspective. Cambridge University Press, United Kingdom pp. 532-551.
- Duval C, Piolino P, Alexandre Bejanin, Francis Eustache, Béatrice Desgranges (2011) Age effects on different components of theory of mind. Consciousness and Cognition 20(3): 627-642.
- Fischer H, Nyberg L, Lars Bäckman (2010) Age-related differences in brain regions supporting successful encoding of emotional faces. Cortex 46(4): 490-497.
- Melehin AI (2018) Assessment of emotional competence as a biopsychosocial marker of the course of aging. Collection of humanitarian studies. Electronic scientific journal 15(6): 1-5.
- Melehin AI (2019) Projective identification when recognizing emotions by face in old age. Personality in a changing world: health, adaptation, development 7(1): 31-48.
- Melehin AI (2019) Understanding deception in old age: specificity and predictors. Neurodynamics. Journal of Clinical Psychology and Psychiatry 3(1): 20-41.
- Melehin AI, Sergienko EA (2019) Cognitive biases in facial emotion recognition in old age. Clinical and special psychology 8(2): 53-79.
- Melehin AI (2016) Model of the mental: the trajectory of changes in the elderly and senile age. Consultative psychology and psychotherapy 24(1): 24-43.
- Ruitenberg MFL, Santens P, Notebaert W (2020) Cognitive and affective theory of mind in healthy aging. Experimental Aging Research 46(5): 382-395.
- Melehin AI (2015) Theory of mind for normal aging. Social psychology and society 1(1): 139-150.
- Carstеnsеn LL, Fung HH, Charles ST (2003) Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motivation and Emotion 27(2): 7-19.
- Yeh ZT (2013) Role of Theory of Mind and executive function in explain social intelligence: a structural equation modeling approach. Aging Ment Health 17(5): 527-534.
- Simpson JR (2014) DSM-5 and neurocognitive disorders. J Am Acad Psychiatry Law 42(2): 159-164.
- Sullivan S, Ruffman T (2004) Social understanding: how does it fare with advancing years? British Journal of Psychology 95(Pt 1): 1-18.
- Melehin AI (2019) The program of development of the model of the psychic (theory of mind) in later ages. Clinical and special psychology 1(1): 110-123.
- Frank Van Overwalle (2009) Social cognition and the brain: a meta-analysis. Human Brain Mapping 30(3): 829-858.
- Pinsker DM, McFarland K, Nancy A Pachana (2009) Exploitations in older adults: social vulnerability and personal competence factors. Journal of Applied Gerontology 29(6): 248-267.
- Cаbinio M, Rossetto F, Valeria Blasi, Federica Savazzi, Ilaria Castelli, et al. (2015) Mind-Reading Ability and Structural Connectivity Changes in Aging. Frontiers in Psychology 6(1): 19-33.
- Pezzuti L, Longobardi E, Serena Rossetti, Elena Bartolini, Giulia Natale, et al. (2015) The Relation between the Theory of Mind and Socio-Emotional Functioning in a Sample of Older Adults. J Neurol Psychol 3(2): 3-21.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...









