
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Research ArticleOpen Access 
The Effect of Remote Consultations on Quality of Care for Patients During the COVID-19 Pandemic: An Update and a Review of Current Literature Volume 5 - Issue 1
Omar Rawi* and Miaaz Zidan
- Primary Health Care Corporation (PHCC), Qatar
Received: December 01, 2022 Published: December 14, 2022
Corresponding author: Dr. Omar Rawi, Consultant Family Physician (MBChB, MRCGP), Primary Health Care Corporation (PHCC), Qatar
Abstract
Background: Many countries around the world used remote consultations in primary care during the COVID-19 pandemic to protect patients and staff from infection.
Aim: The goal of this review was to summarize the academic papers on patients’ experiences with remote consultations in primary care during the COVID-19 pandemic in order to inform future delivery.
Methods: From inception to November 1st, 2022, a systematic literature search was carried out on PubMed, ScienceDirect, Medline, and Scopus. Before reading the full article, the titles and abstracts of the studies were reviewed to determine their eligibility. Then, from those who were eligible, qualitative and quantitative data were collected.
Results: During the COVID-19 pandemic, remote consultation greatly increased worldwide, especially during the COVID-19 lockdowns. Patients reported overall high satisfaction with telehealth in general practice. Telehealth was convenient because it allowed patients to safely access health care without needing to weigh the risk of COVID-19 infection against the need to see a doctor. Telehealth proved beneficial for routine and familiar health issues, as well as when patients and clinicians established professional relationships. This was easier with an already established clinical relationship, but not impossible without one. Telehealth has been less appropriate when a physical examination was required, when the diagnosis was unknown, or when patients strongly preferred to be seen in person.
Conclusions: Even during the disruptive COVID-19 period, which resulted in an unexpected and rapid implementation of telehealth services in general practice, the majority of patients had positive telehealth experiences. Patients will want to be able to choose the type of consultation that best suits their needs, circumstances, and preferences in the future. Technological issues and funding barriers may need to be clarified, and proper communication about key aspects of telehealth would be required for both patients and clinicians (e.g., cost, appropriateness, privacy). Preserving telehealth as an option during an outbreak has the potential to improve many patients’ timely and safe access to primary health care.
Keywords: Primary care; SARS-CoV-2; virtual consultation; telemedicine; telephone consultation
Research Article
Telemedicine (remote consulting) is defined as the communication of medical information and delivery of medical care via electronic, digital, and internet-based communication, as well as telephone communication. Prior to the Coronavirus disease 2019 (COVID-19) pandemic, the primary advantage of remote consulting was the provision of subspecialty healthcare to rural or underserved populations, where avoiding patient travel for hospital visits was seen as a method to enhance equity of care delivery [1] and obtain greater access for patients who had impaired mobility or other disabilities (e.g., cognitive) from chronic neurological diseases [2-4].
For more than a decade [5], remote consulting has been a wellestablished care model in neurology, primarily for stroke treatment. Cardiovascular telemedicine has enhanced patient outcomes such as independent ambulation and disability days by enabling access to acute stroke care and the timely administration of thrombolysis [6]. It has recently emerged as a model for chronic neurological conditions such as Parkinson’s disease, multiple sclerosis, and epilepsy [7]. Qiang and Marras [8] found that implementing remote consulting for Parkinson’s disease patients resulted in high patient satisfaction due to greater convenience, accessibility, and reduced caregiver burden. Furthermore, remote consultation improved medication adherence in patients with multiple sclerosis [9]. Despite the advantages of remote consulting, there are some disadvantages. It is a less personable medium, which makes it difficult to establish rapport in the clinician-patient relationship [10]. Because performing clinical examinations via remote consulting can be difficult or impossible, it is best suited to historydriven conditions. The implications of missing critical information or clinical signs from remote consulting must still be investigated in terms of patient safety and quality of care. Furthermore, there are risks associated with the digital split among patients [11], as well as technical, logistical, and regulatory challenges [11].
The COVID-19 pandemic has compelled a significant shift toward remote consultations [12]. Remote alternative treatments, which eliminate the need for physical contact between patients and healthcare providers, have been adopted by physicians and healthcare systems worldwide, reducing the risk of viral transmission, especially in the COVID-19 scenario. Many of these changes and models of care will almost certainly continue after the pandemic. Sustainable adaptations and improvements to remote delivery systems are thus critical for optimizing healthcare provision and reducing inconsistencies in care. COVID-19 enters the body through the eyes, nose, or mouth and is transmitted through droplets emitted when sneezing, coughing, or speaking [13-17]. Several social distancing and prevention and treatment measures have been implemented by governments around the world to protect the population and the health services that treat them, with the goal of eliminating this once immunity is achieved through vaccination and improvements in treatment are made [18- 28].
Face-to-face consultations for primary care appointments were discouraged in most countries as part of the measures put in place. This has resulted in a radical shift in primary care delivery, with visits increasingly being conducted via remote consultation [29]. In the United States, for example, 46% of patients used telephone consultations in 2020, which was significantly higher than 11% in 2019 [30]. Similar trends have been seen in the United Kingdom, where 80% of appointments will be in person in 2019, but only 50% will be in person in 2020 [31], with telehealth taking the place of the majority of the consultations [32], even though providers are encouraged to do more video consultations. While remote consultations were useful in protecting patients and physicians from COVID-19 during the pandemic, there is uncertainty about their future use, as well as how satisfied patients and primary health care physicians are with them. Thus, the goal of this review was to summarize the findings of previous research on patients’ experiences with remote consultations in primary care settings in order to guide forthcoming research and policy in this area.
Methodology
The current work is a literature review of patients’ experiences with remote consultations in primary care during the COVID-19 pandemic. For this purpose, a search was carried out in the PubMed, Medline, and Google Scholar databases using keywords such as “primary care,” “SARS-CoV-2,” “virtual consultation,” as well as “telemedicine” and “telephone consultation. As a result, we found some initial studies from 2019–2022 and selected those that fit into the proposed theme.
Results
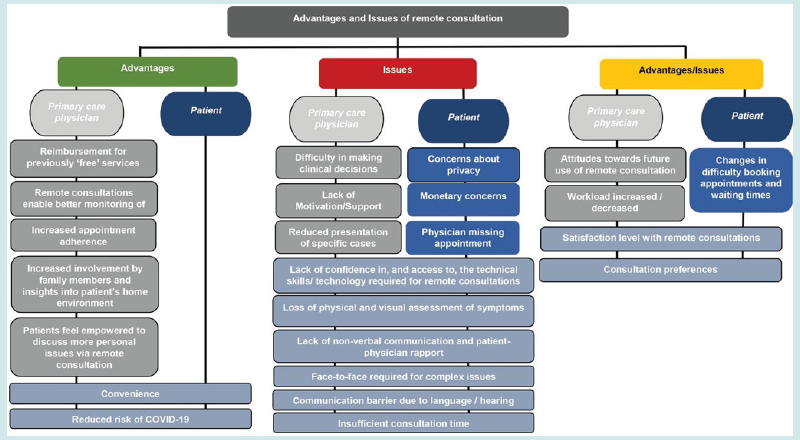
During the COVID-19 pandemic, telehealth could provide numerous benefits to both public and individual health. The number of telehealth patient encounters and the percentage change in telehealth encounters and emergency department visits (Figure 1), as well as the number of telehealth patient encounters for people with COVID-19-like symptoms, coronavirus-related International Classification of Diseases, Tenth Revision (ICD- 10 codes), or coronavirus-related text string entries, have risen exponentially in the United States (Figure 2). It has also been reported that in the latter weeks of March 2020, remote screening and management of people in need of clinical care for COVID-19 as well as other conditions may have increased the availability of treatment at a time when many outpatient offices were shut down or had restricted operating hours (Figures 1 & 2). Widespread availability of telehealth services may have also diminished disease exposure for staff and patients, preserved scarce supplies of personal protective equipment, and reduced patient overload on facilities [33,34]. Also, during the early part of the pandemic, most telehealth patients were treated at home, which may have cut down on the number of people who went to health care facilities. Additionally, this review identified a range of advantages and issues with using remote consultations in primary care during the COVID-19 pandemic. Some of the key advantages described by patients were that remote consultations are more convenient than face-to-face appointments and reduce the risk of patients and staff getting COVID-19. Some of the key issues included a lack of confidence in and access to adequate technology and the loss of non-verbal communication between patients and their primary health care physician (Figure 3).
Figure 1: The number of telehealth patient encounters reported by four telehealth providers who provide services in all states, as well as the percentage change in telehealth encounters and emergency department (ED) visits in the United States from January 1 to March 30, 2019 (comparison period) and January 1 to March 28, 2020 (early pandemic period) [35].
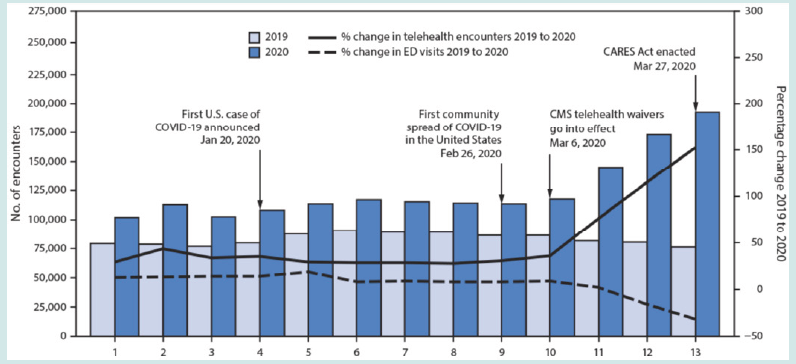
Figure 2: Number of telehealth patient encounters for persons with COVID-19-like symptoms, coronavirus-related ICD-10 codes, or coronavirus-related text string entries reported by four telehealth providers that offer services in all states (United States, January 1–March 28, 2020) [35].
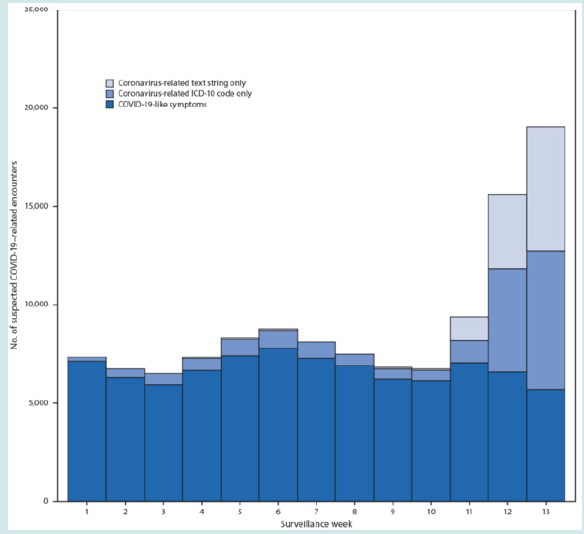
Figure 3: Perceived advantages and issues with remote consultations during the COVID-19 pandemic, according to Verma et al. (2022) [36].
Discussion
Using remote consultations in primary care during the COVID-19 pandemic had a number of benefits and drawbacks, according to this overview. Remote consultations are much more convenient than face-to-face appointments, and they reduce the risk of patients and staff contracting COVID-19. Some of the key issues were a lack of trust in and access to adequate technology, as well as a loss of nonverbal communication between patients and their primary health care physician. There were several differences in the perceived benefits and issues with using remote consultations in primary care between patients and primary health care physicians. Patients, for example, frequently complained that remote consultations were too brief and that they did not always have time to discuss everything they wanted to [35]. One of the key benefits of remote consultations mentioned in certain articles was increased appointment adherence. Indeed, patients have been reported to have higher appointment adherence when compared to face-to-face consultations, with patients missing fewer telephone and video appointments [36,37]. Furthermore, remote consultation increased family members’ involvement and gave them insights into patients’ home environments because it allowed them to see their patients’ home environments, giving them insights into their living conditions [38]. Another advantage of remote consultation is that patients are more confident discussing personal issues. According to one study, telephone consultations helped patients articulate their symptoms more explicitly, whereas face-to-face consultations could be intimidating at times, especially when patients were sharing sensitive information [39].
Several research [38,40-44] found that patients preferred remote consultations to face-to-face appointments. In one study, for example, 47% of patients indicated that remote consultations saved them more than 30 minutes compared to face-to-face consultations [41]. Remote consultations were found to have a lower risk of infection for primary care physicians and patients in three studies [44-46]. In one investigation for example, it was reported that patients prioritised reducing infection risk, particularly those with chronic conditions [46]. Some quantitative and mixed-methods study protocols [40,43] discovered that patients expressed concerns about the security and privacy of their conversations with physicians. Patients expressed concerns in the qualitative literature, primarily because many telemedicine visits took place at home, where family members could overhear [47]. Several studies found that patients were unsure whether shorter telemedicine consultations should be charged the same as face-toface visits [40,44,47]. Furthermore, two studies found that patients complained that telemedicine visits that required follow-up faceto- face visits were charged twice, raising the total cost [44,47].
According to one qualitative study, caregivers of patients discussed issues over the phone and stated that “doctors did not always keep appointments and either called at different times than agreed or did not call at all” [37]. This was reported to be a significant inconvenience for caregivers who do not live with the patients [37]. The single most frequently coded issue identified in the existing literature was a lack of confidence in, and access to, the technical skills or technology required for remote consultations [38,39,43,44,46,47]. In the quantitative literature, one study found that in the United States, more than 90% of patients reported having the necessary technology for remote consultation, with 20% reporting difficulty connecting to it [41]. In a separate study, 26% of patients thought teleconsultation was too complicated [48], and 30% said they had technical problems before or during the visit [40]. These technical challenges were mostly observed in older adults in qualitative literature. Patients and primary care physicians both agreed that using a computer was more difficult for older adults [37,38,39,47,48].
Aside from technological knowledge, numerous studies discovered that a lack of access to technology, particularly for patients living in rural areas, was a problem, including poor connection, poor reception, poor audio quality, and video calls dropping out [38,42,46-48]. A quantitative study conducted in the United States confirmed this finding, reporting that 12% had sound issues, 35% had video issues, and 40% were unable to connect [40]. According to two quantitative studies [41,48], 25–50% of patients have difficulty using their device and/or video telehealth platform. Moreover, many research [38,42,43,47] reported that the loss of physical and visual assessment of symptoms was a problem. According to a quantitative study, 38% of primary care physicians reported an inability to conduct a thorough physical examination, and 16% reported difficulty assessing physical health status (4% could not hear them properly during a video consultation visit) [42]. A qualitative research of primary care physicians found that skin rashes were extremely difficult to treat due to patients’ inability to explain them [38]. Based on the qualitative research, these problems seem to be caused by new or worsening physical problems that are harder to explain over the phone.
According to recent research [13,42-44], the loss of nonverbal communication was an issue, with some patients finding it extremely difficult to express themselves during a remote consultation. Even if they knew the doctor, patients perceived telemedicine to be impersonal [47]. In this way, three investigations [42,45,49] discovered that, because of the loss of physical touch during the remote consultation, primary health care physicians and patients felt disconnected. They considered it an important part of the patient-physician relationship and developing this bond with a new patient was even more difficult [45]. Face-to-face meetings were typically required for complex issues, which was cited as a challenge in several articles examining physician and patient perspectives [38,42,43]. The quantitative literature aided in quantifying the scope of the problem. According to one study, only 50% of primary care physicians thought remote consultations were appropriate for the overall visit they had conducted [50], while another study found that 90% of patients in the United States did not recover from their illnesses by consulting remotely and instead had to visit an urgent care centre or were sent to medical centres for evaluation [40]. Patients and caregivers reported similar results, stating that they prefer face-to-face consultations over phone consultations because it gives them more confidence to express their symptoms clearly [42].
Communication was identified as a problem by both primary care physicians and patients in several studies [38,46,47]. Primary care physicians reported that some patients were unable to communicate because they did not speak the same language [38,46]. The impact of language barriers varied depending on the social vulnerability of the area served by primary health care physicians. According to one quantitative study, providers in highsocial vulnerability index areas were twice as likely to report language barriers as a problem [51]. Aside from language barriers, one study discovered that patients with hearing impairments struggled with remote consultations [47]. One investigation in the quantitative literature discovered that a small percentage of patients (7%) felt that the amount of time allocated to remote consultation was insufficient [40]. Primary care physicians made similar observations in the qualitative literature. In one study, a physician explained that shorter consultations were due to the patient talking less [43], whereas another found that patients wanted to spend less time on the phone [38].
The difficulty of booking appointments and waiting times has changed dramatically as a result of remote consultation. Indeed, according to a quantitative study, 42% of patients expressed concern about the unavailability of physician appointments during a time of need [48]. These findings were partially supported by qualitative research [44]. One study found that patients reported ease in obtaining a remote consultation [47]. Although telehealth is widely accepted by patients and clinicians, it is not without difficulties. Some patients may face challenges due to limited access to the Internet or devices such as smartphones, tablets, or computers, as well as a lack of familiarity with technology. Furthermore, virtual visits may not be appropriate for some people due to their level of acuity or the need for an in-person physical examination or diagnostic testing. Although several reports have expressed concern about the decline in emergency department use during the early pandemic period, this analysis found that only a small proportion of telehealth patients were referred to emergency care. COVID-induced increases in telehealth use may have longterm benefits for improving appropriate emergency department utilisation.
Conclusions
We demonstrated that it is possible to assess the quality of clinical consultations and that the shift from face-to-face to telephone clinics during the COVID-19 pandemic had an effect on this quality. Furthermore, high-quality consultations are associated with higher patient satisfaction, higher clinician satisfaction, and more definitive decisions about the consultation outcome. To improve consultation quality even further, clinicians should take steps to better understand their patients as people, such as learning about their occupations and interests and offering to involve a patient’s family or friends in their healthcare on a more consistent basis. Improved methods should be put in place to ensure that all relevant information is available during the consultation. Given the difficulties of maintaining quality when consulting remotely, consideration should be given to the patient group most suitable for telephone consultations. These areas for improvement must be considered as we move toward a healthcare model that includes increasing levels of remote consultations and deals with the COVID-19 pandemic’s backlog.
Acknowledgments
Not applicable.
Funding
This paper was not funded.
Declaration of Interest
The authors have no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer Disclosures:
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author Contributions
a) Conception and design: Omar Rawi and Miaaz Zidan
b) Analysis and interpretation of the data: Omar Rawi
c) Drafting of the paper: Omar Rawi
d) Revising it critically for intellectual content: Miaaz Zidane
e) Omar Rawi and Miaaz Zidan gave their final approval to the version that will be published.
f) All authors agree to be accountable for all aspects of the work.
References
- Davis LE, Coleman J, Harnar J, King MK (2014) Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemedicine and e-Health 20(5): 473-477.
- Hatcher Martin JM, Adams JL, Anderson ER, Bove R, et al. (2020) Telemedicine in neurology: telemedicine work group of the American Academy of Neurology update. Neurology 94(1): 30-38.
- Patel UK, Malik P, DeMasi M, Lunagariya A, Jani VB (2019) Multidisciplinary approach and outcomes of tele-neurology: a review. Cureus 11(4): e4410-e4415.
- Wechsler LR, Tsao JW, Levine SR, Swain Eng RJ, Adams RJ, et al. (2013) Teleneurology applications: report of the Telemedicine Work Group of the American Academy of Neurology. Neurology 80(7): 670-676.
- Guzik AK, Switzer JA (2020) Teleneurology is neurology. Neurology 94(1): 16-17.
- Bladin CF, Cadilhac DA (2014) Effect of telestroke on emergent stroke care and stroke outcomes. Stroke 45(6): 1876-1880.
- Campos C, Caudevilla E, Alesanco A, Lasierra N, Martinez O, et al. (2012) Setting up a telemedicine service for remote real-time video-EEG consultation in La Rioja (Spain). International journal of medical informatics 81(6): 404-414.
- Qiang JK, Marras C (2015) Telemedicine in Parkinson's disease: a patient perspective at a tertiary care centre. Parkinsonism & related disorders 21(5): 525-528.
- Turner AP, Sloan AP, Kivlahan DR, Haselkorn JK (2014) Telephone counseling and home telehealth monitoring to improve medication adherence: results of a pilot trial among individuals with multiple sclerosis. Rehabilitation psychology 59(2): 136-146.
- Dorsey ER, Venkataraman V, Grana MJ, Bull MT, George BP, et al. (2013) Randomized controlled clinical trial of “virtual house calls” for Parkinson disease. JAMA neurology 70(5): 565-570.
- Schneider RB, Biglan KM (2017) The promise of telemedicine for chronic neurological disorders: the example of Parkinson's disease. The Lancet Neurology 16(7): 541-551.
- Ohannessian R, Duong TA, Odone A (2020). Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR public health and surveillance 6(2): e18810-e18815.
- Dergaa I, Abubaker M, Souissi A, Mohammed AR, Varma A, et al. (2022) Age and clinical signs as predictors of COVID-19 symptoms and cycle threshold value. Libyan Journal of Medicine 17(1): 2010337-2010341.
- Dergaa I, Abdelrahman H, Varma A, Yousfi N, Souissi A, et al. (2021) COVID-19 vaccination, herd immunity and the transition toward normalcy: challenges with the upcoming sports events. Annals of Applied Sport Science 9(3): 0-0.
- Musa S, Dergaa I, Abdulmalik MA, Ammar A, Chamari K, et al. (2021) BNT162b2 COVID-19 vaccine hesitancy among parents of 4023 young adolescents (12-15 years) in Qatar. Vaccines 9(9): 981-985.
- Varma A, Dergaa I, Mohammed AR, Abubaker M, Al Naama A, et al. (2021) Covid-19 and diabetes in primary care-How do hematological parameters present in this cohort? Expert review of endocrinology & metabolism 16(3): 147-153.
- Romdhani M, Vedasalam S, Souissi A, Fessi MS, Varma A, et al. (2022) Is there a diurnal variation of COVID-19 patients warranting presentation to the health centre? A chronobiological observational cross-sectional study. Annals of Medicine 54(1): 3060-3068.
- Akbari HA, Pourabbas M, Yoosefi M, Briki W, Attaran S, et al. (2021) How physical activity behavior affected well-being, anxiety and sleep quality during COVID-19 restrictions in Iran. Eur Rev Med Pharmacol Sci 25(24): 7847-7857.
- Romdhani M, Fullagar HH, Vitale JA, Nedelec M, Rae DE, et al. (2022) Lockdown duration and training intensity affect sleep behavior in an international sample of 1454 elite athletes. Frontiers in Physiology 13(1): 904778-904785.
- Romdhani M, Ammar A, Trabelsi K, Chtourou H, Dergaa I, et al. (2022) Ramadan observance exacerbated the negative effects of COVID-19 lockdown on sleep and training behaviors: an international survey on 1681 Muslim athletes. Frontiers in Nutrition 9(1): 925092-925095.
- Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, et al. (2021) Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biology of Sport 38(4): 495-506.
- Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, et al. (2021) Sleep quality and physical activity as predictors of mental wellbeing variance in older adults during COVID-19 lockdown: ECLB COVID-19 international online survey. International journal of environmental research and public health 18(8): 4329-4334.
- Musa S, Elyamani R, Dergaa I (2022) COVID-19 and screen-based sedentary behaviour: Systematic review of digital screen time and metabolic syndrome in adolescents. PloS one 17(3): e0265560-e0265565.
- Musa S, Dergaa I, Tayebi SM (2022) Emergence of SARS-CoV-2 B. 1.1. 7 and the Future of Mega Sport Events: Is This the Tipping Point from Pandemic to Endemic? Annals of Applied Sport Science 10(1): 0-0.
- Dergaa I, Varma A, Tabben M, Malik RA, Sheik S, et al. (2021) Organising football matches with spectators during the COVID-19 pandemic: What can we learn from the Amir Cup Football Final of Qatar 2020? A call for action. Biology of Sport 38(4): 677-681.
- Dergaa I, Musa S, Romdhani M, Souissi A, Abdulmalik M, et al. (2022) FIFA World Cup 2022: What can we learn from the inspiring Tokyo 2020 Olympic Games held in COVID-19 times? Biology of Sport 39(4): 1073-1080.
- Dergaa I, Saad HB, Souissi A, Musa S, Abdulmalik MA, et al. (2022) Olympic Games in COVID-19 times: lessons learned with special focus on the upcoming FIFA World Cup Qatar 2022. British Journal of Sports Medicine 56(12): 654-656.
- Dergaa I, Ammar A, Souissi A, Fessi MS, Trabelsi K, et al. (2022) COVID-19 lockdown: Impairments of objective measurements of selected physical activity, cardiorespiratory and sleep parameters in trained fitness coaches. EXCLI Journal 21(1): 1084-1098.
- Smith A C, Thomas E, Snoswell C L, Haydon H, Mehrotra A, et al. (2020) Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). Journal of telemedicine and telecare 26(5): 309-313.
- Bestsennyy O, Gilbert G, Harris A, Rost J (2021) Telehealth: a quarter-trillion-dollar post-COVID-19 reality. McKinsey & Company.
- Spencer J, Oung C (2020) How has lockdown affected general practice and where do we go from here. Nuffield Trust, UK.
- Ohannessian R, Duong TA, Odone A (2020) Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR public health and surveillance, 6(2): e18810-e18818.
- Larry A, Green Center. Quick COVID-19 primary care survey, series 3, fielded March 27-30, 2020. Richmond, VA: Larry A. Green Center; 2020.
- Koonin LM, Hoots B, Tsang CA, Leroy Z, Farris K, et al. (2020) Trends in the use of telehealth during the emergence of the COVID-19 pandemic-United States, January–March 2020. Morbidity and Mortality Weekly Report 69(43): 1595-1599.
- (2022) Centre of Disease Control and prevention (CDC). Morbidity and Mortality Weekly Report (MMWR).
- Verma P, Kerrison R (2022) Patients’ and physicians’ experiences with remote consultations in primary care during the COVID-19 pandemic: a multi-method rapid review of the literature. BJGP open 6(2): BJGPO.2021.0192.
- Tuijt R, Rait G, Frost R, Wilcock J, Manthorpe J, et al. (2021) Remote primary care consultations for people living with dementia during the COVID-19 pandemic: experiences of people living with dementia and their carers. British Journal of General Practice 71(709): e574-e582.
- Gomez T, Anaya YB, Shih KJ, Tarn DM (2021) A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. The Journal of the American Board of Family Medicine 34(Supplement): S61-S70.
- Knights F, Carter J, Deal A, Crawshaw AF, Hayward SE, et al. (2021) Impact of COVID-19 on migrants’ access to primary care and implications for vaccine roll-out: a national qualitative study. British Journal of General Practice 71(709): e583-e595.
- Orrange S, Patel A, Mack WJ, Cassetta J (2021) Patient satisfaction and trust in telemedicine during the COVID-19 pandemic: retrospective observational study. JMIR human factors 8(2): e28589-e28595.
- Vosburg RW, Robinson KA (2022) Telemedicine in primary care during the COVID-19 pandemic: provider and patient satisfaction examined. Telemedicine and e-Health 28(2): 167-175.
- T Connolly SL, Gifford AL, Miller CJ, Bauer MS, Lehmann LS, et al. (2021) Provider perceptions of virtual care during the coronavirus disease 2019 pandemic: a multispecialty survey study. Medical care 59(7): 646-652.
- Gold K, Laurie A, Kinney D, Harmes K, Serlin D (2021) Video visits: family physician experiences with uptake during the COVID-19 pandemic. Family Medicine 53(3): 207-210.
- Javanparast S, Roeger L, Kwok Y, Reed RL (2021) The experience of Australian general practice patients at high risk of poor health outcomes with telehealth during the COVID-19 pandemic: a qualitative study. BMC family practice 22(1): 1-6.
- Verhoeven V, Tsakitzidis G, Philips H, Van Royen P (2020) Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ open 10(6): e039674-e039679.
- Hasani SA, Ghafri TA, Al Lawati H, Mohammed J, Al Mukhainai A, et al. (2020) The use of telephone consultation in primary health care during COVID-19 pandemic, Oman: perceptions from physicians. Journal of Primary Care & Community Health 11(1): 2150132720976480-2150132720976485.
- Imlach F, McKinlay E, Middleton L, Kennedy J, Pledger M, et al. (2020) Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC family practice 21(1): 269-283.
- Isautier JM, Copp T, Ayre J, Cvejic E, Meyerowitz Katz G, et al. (2020) People’s experiences and satisfaction with telehealth during the COVID-19 pandemic in Australia: cross-sectional survey study. Journal of medical Internet research 22(12): e24531-e24536.
- Florea M, Lazea C, Gaga R, Sur G, Lotrean L, et al. (2021) Lights and shadows of the perception of the use of telemedicine by Romanian family doctors during the COVID-19 pandemic. International journal of general medicine 14(1): 1575-1587.
- Johnsen TM, Norberg BL, Kristiansen E, Zanaboni P, Austad B, et al. (2021) Suitability of video consultations during the COVID-19 pandemic lockdown: cross-sectional survey among Norwegian general practitioners. Journal of medical Internet research 23(2): e26433- e26438.
- Chang JE, Lai AY, Gupta A, Nguyen AM, Berry CA, et al. (2021) Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post‐COVID era. The Milbank Quarterly 99(2): 340-368.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




