
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Review Article(ISSN: 2690-5760) 
The Connate Anomalism-Ecchordosis Physaliphora Volume 3 - Issue 3
Anubha Bajaj*
- Consultant Histopathologist, AB Diagnostics, India
Received:July 16, 2021 Published: July 23, 2021
Corresponding author:Anubha Bajaj, Consultant Histopathologist, AB Diagnostics, A-1 Ring Road, Rajouri Garden New Delhi, India
DOI: 10.32474/JCCM.2021.03.000162
Preface
Notocord represents a primitive vertebral column which engenders development of prospective vertebrae and inevitably configures nucleus pulposus of the intervertebral disc. Ectopic remnants of notochord tissue were observed within the posterior clivus by Hubert von Luschka in 1856. “Ecchordosis physaliphora” as a terminology for denominating benign neoplasm arising from remnants of the notochord was introduced by Rippert in 1894. Ectopic notochordal rests are generally discerned at the clivus, base of skull or anterior pons. Ecchordosis physaliphora is a congenital, benign hamartoma-like neoplasm emerging as a derivative of remnants of notochord. As a congenital, benign hamartoma engendered from remnants of notochord, ecchordosis physaliphora commonly incriminates the retroclival prepontine region. Intradural chordoma may be misinterpreted and contemplated as an enlarged ecchordosis physaliphora. Nevertheless currently, chordoma, notochordal remnant lesions and ecchordosis physaliphora are considered to be distinct entities with a common genesis.
Disease Characteristics
An estimated ~2% of autopsies demonstrate the occurrence of ecchordosis physaliphora. Following embryogenesis, ecchordosis physaliphora arises along the axis of vertebral column from remnants of notochord cells [1,2]. Ecchordosis physaliphora appears as a miniature, gradually progressive predominantly intradural neoplasm. Generally, the neoplasm is situated within the retroclival, prepontine region although no area of vertebral column is exempt, and the lesion may be discerned within a comprehensive zone ranging from base of skull to the sacrum. Tumefaction of magnitude varying from few millimetres to two centimetres can be confined to the prepontine region, subarachnoid space or subdural space [1,2].
Clinical Elucidation
Ecchordosis physaliphora commonly appears as a midline, non-malignant, gelatinous neoplasm which originates from remnants of the notochord. The benign, asymptomatic, intradural tumefaction depicts a stalk in contiguity with the clivus [1,2]. Direct compression from the neoplasm and enhanced intracranial pressure contributes to pertinent clinical symptoms, as assessed by magnetic resonance imaging (MRI) of the brain. Ecchordosis physaliphora predominantly appears as an asymptomatic neoplasm [1,2]. Although ecchordosis physaliphora is generally an asymptomatic neoplasm, the lesion may engender symptoms such as headache, pneumocephalus, persistent diplopia, spontaneous cerebrospinal fluid (CSF) rhinorrhoea with meningitis and palsy of the abducens (sixth) cranial nerve [3,4]. Acute, severe headache and sudden-onset diplopia may be observed. Cranial neuropathies are exceptional. Intracranial hypertension may ensue [3,4].
Histological Elucidation
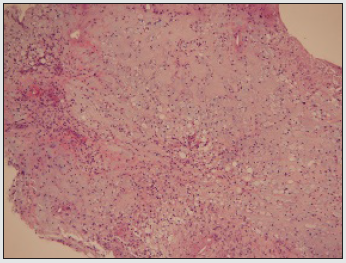
Upon gross examination, a discrete, gelatinous nodule may be exemplified. The neoplasm can depict a bony stalk [3,4]. On histological assessment ecchordosis physaliphora simulates a chordoma, especially while examining miniature, fragmented tissue specimens. Nevertheless, chordoma usually demonstrates an infiltrative tumour perimeter [5,6]. Tumefaction is non-destructive, non-infiltrative and lacks a lobular architecture. Tumefaction is composed of aggregates of physalifarous cells nesting atop a pedicle constituted of mature cartilaginous cells. Physaliferous cells incorporate copious intracytoplasmic vacuoles and circumscribing extracellular pools of mucin [5,6]. Tumour cells are uniform, non variable and appear devoid of cellular and nuclear pleomorphism. Foci of necrosis or mitotic activity are absent. However, mucinous pools imbued with syncytial cords of cells may be absent [5,6]. Ecchordosis physalifora is composed of physalifarous cells admixed with an infiltrate of chronic inflammatory cells such as lymphocytes which appear to invade the adjacent soft tissue [5,6]. Immunohistochemistry depicts tumour cells intensely immune reactive to cytokeratin (AE1/AE3) and weakly immune reactive to S100 protein [5,6].
Figure 1: Ecchordosis physaliphora depicting lobular aggregates of physaliferous cells imbued with bubbly, vacuolated cytoplasm and a singular, uniform nuclei (10).
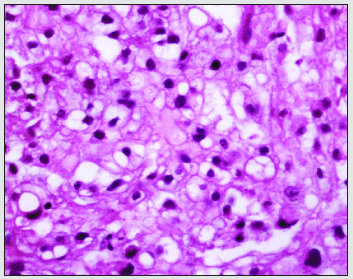
Figure 2: Ecchordosis physaliphora delineating nests of vacuolated cells traversed by fibrous tissue septa and a predominantly lobular architecture (11).
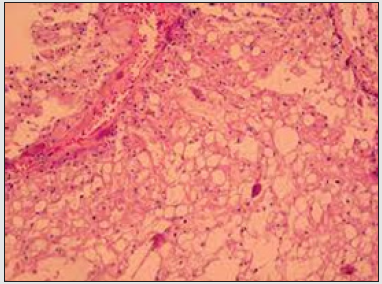
Figure 3: Ecchordosis physaliphora exhibiting uni-vacuolated or multi-vacuolated cells subdivided by fibrous tissue septa preponderantly enunciating a lobular architecture (12).
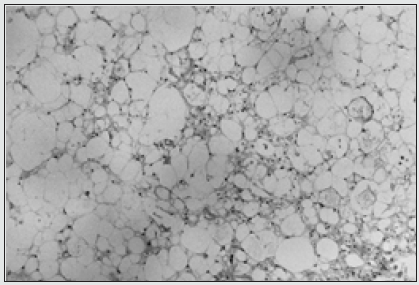
Figure 4: Ecchordosis physaliphora delineating vacuolated, physaliferous cells imbued with bubbly cytoplasm and uniform nuclei (13).
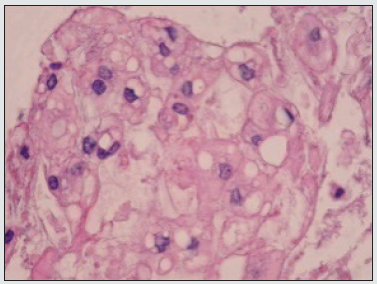
Figure 5: Ecchordosis physaliphora exhibiting lobules of vacuolated cells with bubbly, uni-vacuolated or multi-vacuolated cytoplasm and subdividing fibrous tissue septa (14).
Differential Diagnosis
Ecchordosis physaliphora requires a segregation from diverse retroclival, intradural lesions such as
a) Chordoma which is a malignant, aggressive, symptomatic neoplasm. The lobulated tumefaction demonstrates cellular aggregates, miniature cords, dense sheets, nests and singular cells entrapped within a preponderantly extracellular mesenchymal matrix. Epithelioid cells are predominant and are incorporated with abundant, glycogen-rich, clear to eosinophilic or bubbly, vacuolated cytoplasm [7,8]. Fibrous tissue septa traversing the neoplasm demarcate tumour parenchyma into lobules. Physaliferous tumour cells are imbued with bubbly cytoplasm and appear intermingled with an extensive myxoid stroma. Mitotic figures are infrequent. Tumour perimeter is infiltrative. Chordoma depicts an enhanced signal intensity upon magnetic resonance imaging following administration of radioactive contrast [7,8].
b) Benign notochordal cell tumour (BNCT) incriminates bone or vertebral bodies wherein the architecture of bone trabeculae is maintained. Essentially, the neoplasm is composed of solid areas, nests or sheet-like proliferation of uni-vacuolated or multi-vacuolated physaliferous cells. Generally, physaliferous cells are imbued with a singular vacuole [7,8]. Tumour cells permeate between existing bone trabeculae, supplant the bone marrow and invade medullary spaces between bone trabeculae although trabecular architecture is well preserved. Islands of hematopoietic cells or mature adipose tissue aggregates confined to the bone marrow appear intermingled with sheets of neoplastic cells [7,8].
c) Metastasis upon skull base delineates tumour cells which display diverse morphological configurations pertaining to the primary neoplasm. Epithelial neoplasms articulate tumour acini, sheets, columns and cords of epithelial cells which configure a solid or papillary pattern. Tumour cells exhibit morphological and functional similarity to the parent neoplasm and enunciate features of malignant metamorphosis such as loss of polarity, pleomorphism, enhanced nucleo-cytoplasmic ratio, anisonucleosis, anisocytosis, hyperchromasia and significant mitotic activity with atypical mitosis. Multinucleated tumour giant cells or enlarged tumour cells with singular, bizarre nuclei are observed [7,8].
d) Dermoid cyst is layered with stratified squamous epithelium incorporated with cutaneous adnexa such as hair follicles and sebaceous glands. Eccrine sweat glands and apocrine glands are also exemplified. Occasionally, smooth muscle may be discerned although cartilage and bone are absent [7,8].
e) Epidermoid cyst or a sub-epidermal cyst may or may not communicate with the superimposed epidermis. The cyst is layered with stratified squamous epithelium demonstrating a prominent granular layer. Cyst wall is devoid of eccrine glands, sebaceous glands or hair follicles. The cystic cavity is incorporated with abundant keratin flakes. Rupture of the cyst frequently evokes an inflammatory and foreign body giant cell reaction [7,8].
f) Arachnoid cyst communicates with the subarachnoid space, simulates signal intensity of cerebrospinal fluid (CSF) and lacks image enhancement. Cyst wall is configured of delicate fibrous connective tissue and appears focally or diffusely layered by meningothelial cells [7,8].
Investigative Assay
Computerized tomography (CT) is an insensitive technique for assessing congenital hamartomas as ecchordosis physaliphora as the lesion may be obscured by artefacts of posterior fossa and may depict a density akin to cerebrospinal fluid (CSF). However, discontinuity of the bony clivus can be visualized as a well demarcated, smoothly corticated zone which is devoid of aggressive neoplastic features. Occasionally, a pathognomonic, osseous stalk is discerned at the base of the lesion [7,8]. Magnetic resonance imaging (MRI) of the brain along with or in the absence of contrast administration is an optimal investigative modality for assessing ecchordosis physaliphora. Tumour enhancement upon contrast administration is exceptional [7,8]. MRI with administration of contrast is a preferred diagnostic modality for distinguishing ecchordosis phyaslifora from malignant chordoma. Appropriate discernment of ecchordosis physaliphora can be challenging in the absence of an MRI [8,9]. Magnetic resonance imaging (MRI) demonstrates a non-enhancing lesion at specified sites with a stalklike contiguity to the clivus. A mass effect can be delineated upon ventral pons and associated cranial nerves [8,9]. Features upon MRI are usually nonspecific with the exclusion of ascertained, typical tumour locations as encountered with retroclival, prepontine or intradural lesions. Characteristically, MRI is a superior technique for segregating echordosis physaliphora from chordoma and diverse malignant, clivus neoplasms [8,9]. A heterogeneously hypo-intense signal intensity upon T1 weighted imaging and a heterogeneously hyper-intense signal intensity upon T2 weighted imaging is observed [8,9]. Upon administration of gadolinium contrast, a variable signal intensity is exemplified although majority of instances lack substantial image enhancement [8,9]. Cerebrospinal fluid obtained from a lumbar puncture demonstrates intracranial hypertension wherein idiopathic intracranial hypertension requires a demarcation from tumour engendered intracranial hypertension [8,9].
Therapeutic Options
Management of benign, asymptomatic ecchordosis physaliphora is usually conservative, especially with preliminary neoplasms. Aggressive surgical procedures are adopted for treating instances with absence of tumour amelioration upon conservative therapy or deterioration of clinical symptoms [8,9]. Symptomatic ecchordosis physaliphora is extremely exceptional and can be appropriately managed with diverse surgical strategies contingent to tumour site, tumour magnitude and the mandated, comprehensive surgical resection of the neoplasm [8,9]. Administration of corticosteroids as a treatment strategy for managing ecchordosis physaliphora remains debatable [8,9].
References
- Sun R, Ajam Y, Gerald Campbell, Todd Masel (2020) A Rare Case of Ecchordosis Physaliphora Presenting with Headache, Abducens Nerve Palsy and Intracranial Hypertension. Cureus 12(6): e8843.
- Ilorah C, Bond B, Jorge C Kattah, Bahareh Hassanzadeh (2017) An Incidental Finding of Ecchordosis Physaliphora in a Case of Abducens Nerve Palsy: Case Report. Neuroophthalmology 42(4): 233-236.
- Ghimire P, Shapey J, Istvan Bodi, Steve Connor, Nicholas Thomas, et al (2020) Spontaneous tension pneumocephalus and pneumoventricle in ecchordosis physaliphora: case report of a rare presentation and review of the literature. Br J Neurosurg 34(5): 537-542.
- Galloway L, Hayhurst C (2019) Spontaneous cerebrospinal fluid rhinorrhoea with meningitis secondary to ecchordosis physaliphora. Br J Neurosurg 33(1): 99-100.
- Ahn SS, Han J (2016) Ecchordosis physaliphora presenting with abducens nerve palsy. J AAPOS 20(3): 266-268.
- Park HH, Lee KS, Sung Jun Ahn, Sang Hyun Suh, Chang-Ki Hong (2017) Ecchordosis physaliphora: typical and atypical radiologic features. Neurosurg Rev 40(1): 87-94.
- Yamamoto T, Yano S, Takuichiro Hide, Jun Ichi Kuratsu (2013) A case of ecchordosis physaliphora presenting with an abducens nerve palsy: a rare symptomatic case managed with endoscopic endonasal transsphenoidal surgery. Surg Neurol Int p. 4- 13.
- Alkan O, Yildirim T, Osman Kizilkiliç, Meliha Tan, Melih Cekinmez (2009) A case of ecchordosis physaliphora presenting with an intratumoral haemorrhage. Turk Neurosurg 19(3): 293-296.
- Ciarpaglini R, Pasquini E, Diego Mazzatenta, Andrea Ambrosini Spaltro, Vittorio Sciarretta, et al (2009) Intradural clival chordoma and ecchordosis physaliphora: a challenging differential diagnosis: case report. Neurosurgery 64(2): 387-388.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





