Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Research Article(ISSN: 2690-5760) 
Preoperative Endoscopic Findings in Morbidly Obese Patients Volume 5 - Issue 2
Fernando Comunello Schacher1*, Amanda Pereira Medeiros1, Letícia Bernardon1, Fernanda Karlinski Fernandes Sacco1, Lucas Spadari Maggioni1, Leonardo Wagner Grillo1, Leonardo de Lima Lardi1, Myriam Moretto1, Ângelo Zambam de Mattos2, Carlos Kupski1, Claudio Cora Mottin3 and Ari Ben Hur Stefani Leão1
- 1Gastroenterology Unit of Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, Brasil
- 2Gastroenterology Unit of Universidade Federal de Ciências da Saúde de Porto Alegre, Porto Alegre, Brasil
- 3Metabolic Surgery of Hospital São Lucas, Porto Alegre, Brasil
Received:January 13, 2023; Published: January 27, 2023
Corresponding author: Fernando Comunello Schacher, MD, Gastroenterology Unit of Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, Ipiranga avenue 6690, Brasil
DOI: 10.32474/JCCM.2023.05.000206
Abstract
Background: Morbid obesity is considered a worldwide epidemic, affecting more than half a billion adults, thus having a large impact on morbidity and mortality.
Aim: Evaluated the endoscopic findings of patients with morbid obesity in a preoperative evaluation of bariatric surgery to verify the importance of performing upper digestive endoscopy in this population.
Methods: In this cross-sectional study, upper digestive endoscopies were evaluated in morbidly obese candidates for bariatric surgery regarding their preoperative endoscopic findings.
Results: Of the 1912 endoscopies evaluated, esophagitis was found in 660 patients (34.5% of the sample), the presence of Helicobacter pylori infection in 1174 patients (61.4% of the sample) and neoplasms in 3 patients (0.15% of the sample).
Conclusions: There was a high rate of esophagitis and H. pylori infection and a low prevalence of neoplasias in the present sample.
Keywords:Morbid obesity; perioperative endoscopy; H. pylori infection; endoscopic findings; esophagitis
Core TipThis is a retrospective study to evaluate the endoscopic findings of morbidly obese patients in the preoperative scenario. The findings suggest a high prevalence of esophagitis, as well as H. Pylori infection. There were three cases of neoplasms, which changed the surgery planning.
Introduction
Obesity is considered a worldwide epidemic, affecting more than half a billion adults [1]. In 2008, the prevalence of obese individuals was 34% in the United States population [2,3,4] as com pared to approximately 14% in the Brazilian population [5]. With regard to morbid obesity, defined as a body mass index greater than 40 kg/m2, the prevalence in the United States is 7% [6] and it is 2.8% in Brazil [7]. In addition to contributing to the development of various diseases, such as hypertension, diabetes mellitus and dyslipidemia, obesity has been associated with several benign gastrointestinal diseases, such as gastroesophageal reflux disease (GERD), Barrett’s esophagus, esophagitis, non-fatty liver disease (for instance, cholangiocarcinoma), hepatocellular carcinoma, pancreatic cancer, colorectal cancer and esophageal cancer [8]. In addition, obesity has the potential to reduce longevity by 22% [9]. Bariatric surgery, by providing sustained weight loss, is able to resolve comorbidities in up to 80% of cases [10,11]. There is also evidence that bariatric surgery is associated with reduced mortality [12]. There currently is a lack of consensus regarding the need of endoscopy in the preoperative scenario of bariatric surgery. While some medical associations recommend performing upper digestive endoscopy in the preoperative evaluation [6,13,14], there are authors that suggest a non-endoscopic approach [15,16]. In the present study, we evaluated the endoscopic findings of patients with morbid obesity in a preoperative evaluation of bariatric surgery to verify the importance of performing upper digestive endoscopy in this population.
Methods
Study design
In this cross-sectional study, upper digestive endoscopies performed between January 2010 and December 2015 were reviewed for the preoperative evaluation of consecutive candidates for bariatric surgery at the São Lucas Hospital of the Pontifical Catholic University in Rio Grande do Sul (HSL – PUCRS), which is one of the largest bariatric surgery centers in southern Brazil. The study was approved by the ethics committee of the hospital.
Patients
During the study period, 2307 endoscopies were performed in candidates for bariatric surgery. Of these, 1912 candidates were evaluated; the remaining candidates were excluded due to lack of data in the medical records.
Data collection
Data was collected through the electronic medical records of the patients. The following variables were evaluated: sex, age, smoking, BMI, H. pylori infection, Los Angeles classification, Barrett’s esophagus and the presence of other endoscopic changes (eosinophilic esophagitis, gastric or duodenal ulcers, subepithelial lesions, celiac disease and other changes in the duodenal bulb, such as duodenitis or polyps).
Statistical analysis
Continuous variables were described as the means and standard deviations (SD) if they had a normal distribution or as the medians and interquartile ranges if they had a non-normal distribution. Categorical variables were described as absolute numbers and percentages. Descriptive analyses were performed using SPSS 21.0 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.) and Excel 2011.
Results
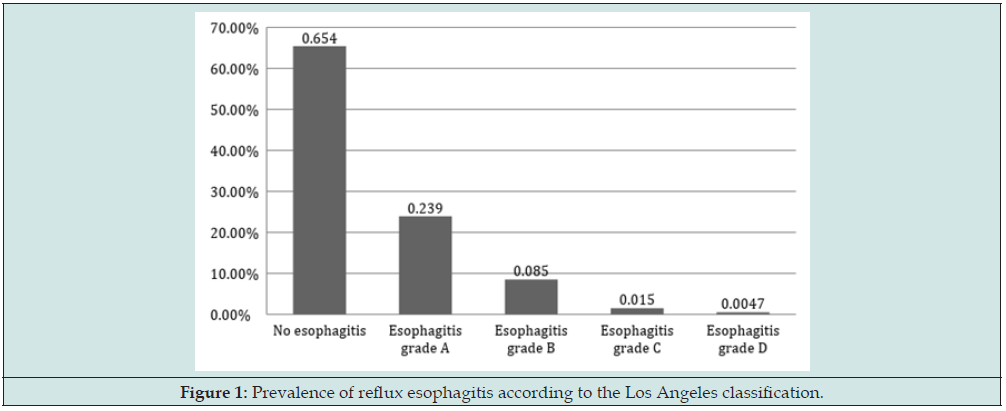
Of the 1912 patients analyzed, the mean age was 38.13 years (± 10.24). Four hundred eighty-five patients were male (25.4%). The mean BMI was 46.26 kg/m2 (± 7.24). The majority of the patients were non-smokers (1224 patients, 64%), whereas 26.4% (506 patients) were former smokers, and only 9.4% (181 patients) were active smokers. The data are presented in Table 1. Because of the protocol, it is necessary to analyze the presence of H. pylori prior to bariatric surgery, and all patients underwent biopsies. In 89% of the sample (1703 patients), the urease test was performed. In the remaining 11% (209 patients), histopathological analysis was per formed using Giemsa staining. The prevalence of individuals infected with H. pylori was 61.4% (1174 patients). Of the other variables studied, in 660 patients (34.5%), there were signs of some degree of peptic esophagitis by endoscopy according to the Los Angeles classification (Figure 1). Hiatal hernias were present in 7.5% of the cases (147 patients): 6.6% were small hernias (with a length between 2 and 3 cm), 0.8% were medium-sized hernias (with a length between 3 and 5 cm), and 0.1% were large hernias (with a length greater than 5 cm).
Mucosal alterations compatible with endoscopic gastritis were evaluated using the Sydney system and were identified in 43.8% of cases (840 patients), regardless of their subclassification. Gastric subepithelial lesions were also found in 0.5% of cases (11 patients). When we analyzed other relevant findings, three cases of malignant neoplasms were observed: one case of esophageal neoplasia and two cases of gastric neoplasms, which represented 0.15% of the sample. In addition, 30 cases of gastric ulcers and 12 cases of duodenal ulcers (2.1% of patients) were detected. Gastric polyps were found in 4.9% of patients (94 cases), and Barrett’s esophagus, confirmed by biopsies, was identified in 0.5% of the sample (11 patients). The other findings are described in Table 1.
Discussion
This study describes the largest published sample of morbidly obese patients who are candidates for bariatric surgery regarding their preoperative endoscopic findings. The largest samples described prior to this study were comprised of 801 [17] and 626 [18] patients, which makes clear the contribution from our data obtained from 1912 patients. In this context, among our findings, we highlight a high prevalence of esophagitis, gastritis and H. pylori infection as well as a low prevalence of malignant neoplasms among morbidly obese patients. In the present study, we found a significant female predominance among patient candidates for bariatric surgery (about two-thirds of the sample), which is similar to the findings from other studies [7,19].
Our data suggest a high rate of H. pylori infection (61.4%). Data from H. pylori infection in the obese population are sparser than those from the general population, showing a wide range in the prevalence. In evaluations of obese populations in developed countries, there is a prevalence of 8.7% in Germany [20] up to 29.7% in the USA.[28] However, our findings are close to those found in developing countries, where there is up to 80% prevalence [21]. Regarding the finding of erosive esophagitis in our sample (34.5%), our data are consistent with the literature, which suggests that obesity increases the probability of erosive esophagitis by 2.5 times [22]. In our sample, we found one case of esophageal tumor and two cases of gastric tumors. Considering the importance of proceeding rapidly to cancer treatment and uncertainty regarding the prognosis of patients, it was decided not to perform bariatric surgery in these cases, leaving to re-evaluate this indication after the end of oncological treatments. This highlights the importance of endoscopy prior to bariatric surgery, since obesity is a risk factor for several neoplasms.
There is a recommendation by some medical societies to perform an upper digestive endoscopy together with the rest of the preoperative evaluation in obese candidates for bariatric surgery, even in asymptomatic patients [6,13,14]. However, some authors have suggested that a non-endoscopic approach be performed in asymptomatic patients [15,16]. Nevertheless, the role of endoscopic evaluation would be justified by the following factors: to potentially identify pathologies or lesions that must be treated prior to surgery; to change the surgical technique to be performed; to predict the possibility of postoperative anastomotic complications; or even to contraindicate the operation [23]. In addition to these possible findings, another advantage is the evaluation of the presence of H. pylori, which would allow an infection to be treated prior to surgery [6], as it is associated with an increase in the incidence of gastric cancer [24] and anastomotic ulcers [6]. According to previous evaluations [17], despite the low prevalence of conditions that may contraindicate or alter the surgical decision, as corroborated by our study, the performance of upper gastrointestinal endoscopy prior to surgery has the potential to identify lesions and to evaluate the presence of H. pylori. We believe that a cost-effectiveness study could be useful for decisions making regarding the indication of routine upper gastrointestinal endoscopy prior to bariatric surgery. Our work has limitations. The study design did not include the evaluation of a control group, which prevented the comparison of our findings with those of a non-obese population, making this a descriptive study. In addition, the study was performed from secondary data, which resulted in the loss of a small portion of cases that had incomplete medical records. However, we believe that the size of the sample evaluated, which is the largest ever published to date, makes our findings robust and reliable [25-30].
Conclusion
In the present study, we describe the endoscopic findings from morbidly obese candidates for bariatric surgery, reporting a high prevalence of reflux esophagitis, gastritis and H pylori infection as well as a low prevalence of malignant neoplasms. Conditions that contraindicated bariatric surgery were infrequent, but the absence of preoperative diagnosis could have serious consequences. Thus, we conclude that a cost-effectiveness analysis would be important to define the role of upper gastrointestinal endoscopy in the evaluation of patients who are candidates for bariatric surgery.
Authors contributions
Schacher FC designed, performed the research and wrote the paper; Medeiros AP designed and performed the research; Bernardon L performed the research; Sacco FKF performed the research; Maggioni LM, Grillo LW, Lardi LL, Moretto M and Mottin CC provided clinical advice and supervised the report; Mattos AZ provide clinical advice, wrote the paper; Leao ABS deigned the research, provided clinical advice and supervised the report.
Supported Foundations
There was no funding.
Institutional Review Board Statement
This study was reviewed and approved by the Ethics Committee of the São Lucas Hospital of the Pontifical Catholic University in Rio Grande do Sul.
Informed Consent Statement
Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict of Interest Statement
We have no financial relationships to disclose.
Data Sharing Statement
No additional data is available.
References
- (2016) World Health Organization. Obesity and overweight.
- Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 307(5): 491-497.
- Ogden CL, Carroll MD, Kit BK, Flegal KM (2012) Prevalence of obesity in the United States, 2009-2010. NCHS Data Brief 82(1): 1-8.
- Ogden CL, Carroll MD, Kit BK, Flegal KM (2013) Prevalence of Obesity Among Adults: United States, 2011-2012. NCHS Data Brief 131(1): 1-8.
- (2000) Brasil, Ministério da Saúde . Portaria GM/MS no 196 de 29 de fevereiro de 2000. Distrito Federal, Brasí
- Anderson MA, Gan SI, Fanelli RD, Baron TH, Banerjee S, et al. (2008) Role of endoscopy in the bariatric surgery patient. Gastrointest Endosc 68(1): 1-10.
- Kelles SMB, Machado CJ, Barreto SM (2014) Arq Bras Cir Dig 27(1): 261-267.
- Nam SY (2016) Obesity-Related Digestive Diseases and Their Pathophysiology. Gut Liver 11(3): 323-334.
- Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB (2003) Years of Life Lost Due to Obesity. JAMA 289(2): 187-193.
- Kopelman PG (2000) Obesity as a medical problem. Nature 404(6778): 635-643.
- Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, et al. (2009) Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 122(3): 248-256.
- Sjostrom L, Narbro K, Sjöström CD, Karason K, Larsson B, et al. (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 357(8): 741-752.
- Sharaf RN, Weinshel EH, Bini EJ, Rosenberg J, Sherman A, et al. (2004) Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg 14(10): 1367-1372.
- Sauerland S, Angrisani L, Belachew M, Chevallierv JM, Favretti F, et al. (2005) Obesity surgery: evidence-based guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc 19(2): 200-221.
- Loewen M, Giovanni J, Barba C (2008) Screening endoscopy before bariatric surgery: a series of 448 patients. Surg Obes Relat Dis 4(6): 709-712.
- Peromaa Haavisto P, Victorzon M (2013) Is routine preoperative upper GI endoscopy needed prior to gastric bypass? Obes Surg 23(6): 736-739.
- Wolter S, Duprée A, Miro J, Cornelia Schroeder, Marie Isabelle Jansen, et al. (2017) Upper Gastrointestinal Endoscopy prior to Bariatric Surgery-Mandatory or Expendable? An Analysis of 801 Cases. Obes Surg 27(8): 1938-1943.
- Muñoz R, Ibáñez L, Salinas J, Escalona A, Pérez G, et al. (2009) Importance of routine preoperative upper GI endoscopy: why all patients should be evaluated? Obes Surg 19(4): 427-431.
- Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, et al. (2004) Bariatric Surgery: A Systematic Review and Meta-analysis. JAMA 292(14): 1724-1737.
- Küper MA, Kratt T, Kramer KM, Zdichavsky M, Schneider JH, et al. (2010) Effort, safety, and findings of routine preoperative endoscopic evaluation of morbidly obese patients undergoing bariatric surgery. Surg Endosc 24(8): 1996-2001.
- Crowe SE (2016) Bacteriology and epidemiology of Helicobacter pylori infection. UpToDate pp. 1-6.
- El Serag HB, Graham DY, Satia JA, Rabenec L (2005) Obesity Is an Independent Risk Factor for GERD Symptoms and Erosive Esophagitis. The American Journal of Gastroenterology 100(6): 1243-1250.
- Abd Ellatif ME, Alfalah H, Asker WA, El Nakeeb AE, Magdy A, et al. (2016) Place of upper endoscopy before and after bariatric surgery: A multicenter experience with 3219 patients. World J Gastrointest Endosc 8(10): 409-417.
- Malfertheiner P, Megraud F, O Morain CA, Atherton J, Axon ATR, et al. (2017) Management of Helicobacter pylori infection-the Maastricht IV/ Florence Consensus. Gut 61(1): 646-664.
- Sturm R, Hattori A (2013) Morbid obesity rates continue to rise rapidly in the United States. Int J Obes (Lond) 37(6): 889-891.
- Ellulu MS (2017) Obesity, cardiovascular disease, and role of vitamin C on inflammation: a review of facts and underlying mechanisms. Inflammopharmacology 25(3): 313-328.
- (1998) National Institutes of Health. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. Obes Res 6(Suppl 2): 51S-209S.
- Almeida AM, Cotrim HP, Santos AS, Bitencourt AG, Barbosa DB, et al. (2008) Preoperative upper gastrointestinal endoscopy in obese patients undergoing bariatric surgery: is it necessary? Surg Obes Relat Dis 4(2): 144-149.
- Wilson LJ, Ma MSW, Hirschowitz BI (1999) Association of obesity with hiatal hernia and esophagitis. American Journal of Gastroenterology 94(10): 2840-2844.
- Verma S, Sharma D, Kanwar P, Sohn W, Mohanty SR, et al. (2013) Prevalence of Helicobacter pylori infection in bariatric patients: a histologic assessment. Surg Obes Relat Dis 9(5): 679-685.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...