
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Case Report(ISSN: 2690-5760) 
Nodular COVID-19 Pneumonia with Wavy Triple Sign or Yasser’s Sign and Movable Phenomenon; Poor Prognostic Value but Dramatic Response: at Home Management Volume 3 - Issue 3
Yasser Mohammed Hassanain Elsayed*
- Critical Care Unit, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Egypt
Received:August 02, 2021 Published: August 17, 2021
Corresponding author:Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
DOI: 10.32474/JCCM.2021.03.000167
Abstract
Rationale: COVID-19 pandemic with severe acute respiratory manifestations had emerged in Wuhan, China in December 2019. Wavy triple sign or Yasser’s sign is a novel diagnostic and therapeutic sign for hypocalcemic patients. Interestingly, the tachypnea or hyperventilation syndrome presentation is an impact on respiratory alkalosis and subsequent hypocalcemia. Metastatic carcinoma is considered a serious differential diagnosis.
Patient concerns: A young-aged housewife female COVID-19 thin patient presented to physician outpatient clinic with nodular COVID-19 pneumonia with Wavy triple sign or Yasser’s sign and Movable phenomenon.
Diagnosis: Nodular COVID-19 pneumonia with Wavy triple sign or Yasser’s sign and Movable phenomenon. Interventions: Non-contrasted chest CT scan, electrocardiography, and oxygenation.
Outcomes: Dramatic of both clinical, electrocardiographic, and radiological improvement had happened.
Lessons: The nodular COVID-19 pneumonic presentation maybe carries poor prognostic value but a dramatic response. It signifies the role of anticoagulants, antiplatelet, anti-infective drugs, and steroids in COVID-19 patients with nodular COVID-19 pneumonia. The presence of the Wavy triple sign or Yasser’s sign and the Movable phenomenon of hypocalcemia with a COVID-19 pneumonic patient was reasonable
Keywords: COVID-19; Coronavirus; Nodular Pneumonia; Hypocalcemia; Wavy Triple Sign or Yasser’s Sign; Movable Phenomenon; Nodules
Abbreviations: CBC: Complete Blood Count; COVID-19: Coronavirus Disease 2019; CT: Computed Tomography; ECG: Electrocardiography; O2: Oxygen; POC: Physician Outpatient Clinic; SGOT: Serum Glutamic-Oxaloacetic Transaminase; SGPT: Serum Glutamic-Pyruvic Transaminase; VR: Ventricular Rate
Introduction
The essential appearance of a current Coronavirus-2 (COVID-19) that is causing serious acute respiratory syndrome (SARS) had emerged in Wuhan; China in December 2019 [1]. COVID-19 Disease is an extremely communicable; expeditiously spread; deadly worldwide disease [2]. The most common signs encountered are especially well-described in chest computed tomography (CT). Typical chest CT scanning includes bilateral; mainly peripheral and posterior; multi-lobar; ground-glass opacities (GGO) [3]. A nodule is an opacity less than 3 cm in diameter but with either regular or irregular borders. However, viral pneumonitis is characterized by the existence of nodules [4]. The recorded incidence of pulmonary nodules in cases with COVID-19 pneumonia is 3–13% [5] and may be accompanied by surrounding halo [6]. Yang et al. [7] reported that the presence of nodules in chest CT is a sign of progressive deteriorate course. Mediastinal lymph nodes may be enlarged if the short-axis diameter is 1 cm or more. In cases of COVID-19; mediastinal lymphadenopathy is not a typical finding; with the incidence of 1–6% [8]. Whatever the existence of enlarged lymph nodes is an indication sign for a severe or critical COVID-19 disease. Also, the presence of enlarged lymph nodes may indicate superimposed bacterial infection [8]. Currently, Valette et al. [9] found that there is a high incidence of lymphadenopathy (66%) in the admitted patients to ICU with severe respiratory distress syndrome (ARDS); especially with the presence of some large lymph nodes are considered a sign of critically ill COVID-19 disease [8]. Wavy triple an electrocardiographic sign (Yasser’s Sign) is a recently novel diagnostic sign innovated in hypocalcemia [10]. The analysis for this sign in the author interpretations are based on the following:
a. Different successive three beats in the same lead are affected.
b. All ECG leads can be implicated.
c. An associated elevated beat is seen with the first of the successive three beats; a depressing beat with the second beat; and an isoelectric ST-segment in the third one.
d. The elevated beat is either accompanied by ST-segment elevation or just an elevated beat above the isoelectric line.
e. Also, the depressed beat is either associated with ST-segment depression or just a depressing beat below the isoelectric line.
f. The configuration for depressions; elevations; and isoelectricities of ST-segment for the subsequent three beats are variable from case to case. So, this arrangement is nonconditional.
g. Mostly, there is no participation among the involved leads.
The author intended that is not conditionally included in an especial coronary artery for the affected leads [10].
The occurrence of a changeable Wavy triple electrocardiographic sign in ECG leads is a hallmark for the existence of the Movable phenomenon or Yasser’s phenomenon of hypocalcemia [11].
Tachypnea was a possible cause of hypocalcemia and subsequent Wavy triple electrocardiographic and Movable-weaning phenomenon of hypocalcemia [12].
Case Presentation
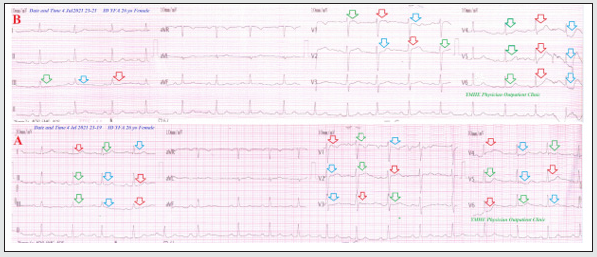
A 26-year-old married housewife Egyptian female patient presented to the physician outpatient clinic (POC) with fever; acute tachypnea; and cough. Generalized malaise; anorexia; loss of smell and taste; and generalized body pains were associated symptoms. The patient gave a history of the symptoms for 5 days. Currently, she had a history of contact with her neighbor who confirmed a COVID-19 patient in the past 12 days. Informed consent was taken. Upon general physical examination; generally; the patient was tachypneic; distressed; with a regular pulse rate (sinus arrhythmia with VR; 72 bpm); blood pressure (BP) of 100/60 mmHg; respiratory rate of 25 bpm; the temperature of 39 °C; and pulse oximeter of oxygen (O2) saturation of 93%. She appeared thin. The patient was tested for latent tetany which was positive. No more relevant clinical data were noted during the clinical examination. The patient was treated at home with COVID-19 pneumonia with hypocalcemia. Initially, the patient was treated with O2 inhalation by O2 cylinder (100%; by nasal cannula; 5L/min). The patient was maintain treated with cefotaxime; (1000 mg IV every 8hours); azithromycin (500 mg PO single daily dose); oseltamivir (75 mg PO twice daily only for 5 days); and paracetamol (500 mg IV every 8 hours as needed). SC enoxaparin 80 mg twice daily); aspirin tablet (75 mg; once daily); clopidogrel tablet (75 mg; once daily); and hydrocortisone sodium succinate (100 mg IV every 12 hours) were added. The patient was daily monitored for temperature; pulse; blood pressure; and O2 saturation. The initial ECG was done within 8 days of the presentation showing sinus arrhythmia of VR of 72 with Wavy triple sign or Yasser’s sign in I; II; III; and V1-6 leads (Figure 1A). The second ECG tracing was done within 2 minutes of initial ECG tracing showing sinus arrhythmia of VR of 75 with Movable phenomenon or Yasser’s phenomenon and Wavy triple sign or Yasser’s sign in I; V1; V2; V4; V5; and V6 leads (Figure 1B). The initial complete blood count (CBC); Hb was 10.3 g/dl; RBCs; 3.99*103/mm3; WBCs; 22.1*103/mm3 (Neutrophils; 82.7 %; Lymphocytes: 12.3%; Monocytes; 4%; Eosinophils; 1% and Basophils 0%); Platelets; 285*103/mm3. S. Ferritin was high; 663 ng/ml. D-dimer was high (847 ng/ml).
Figure 1: ECG tracings; A. tracing was done within 8 days of the presentation showing sinus arrhythmia of VR of 72 with Wavy triple sign or Yasser’s sign in I, II, III, and V1-6 leads (red, green, and blue arrows). B. tracing was done within 2 minutes of A. tracing showing sinus arrhythmia of VR of 75 with Movable phenomenon or Yasser’s phenomenon and Wavy triple sign or Yasser’s sign in I, V1, V2, V4, V5, and V6 leads (red, green, and blue arrows).
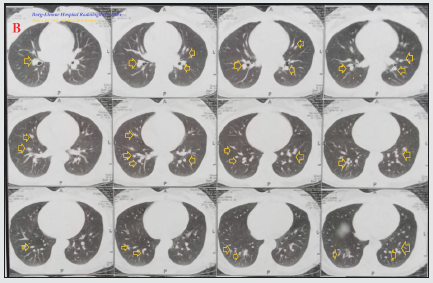
CRP was high (26 g/dl). LDH was normal (196 U/L). SGPT was normal (24 U/L); SGOT was normal (32 U/L). Serum creatinine was normal (1 mg/dl) and blood urea was normal (29 mg/dl). RBS was normal (104 mg/dl). Ionized calcium was slightly low 0.77 mmol/L). The troponin test was negative. After 11 days of management; RBS was normal (97 mg/dl). CBC; Hb was 11.1 g/dl; RBCs; 4.7*103/mm3; WBCs; 15.1*103/mm3 (Neutrophils; 71 %; Lymphocytes: 23%; Monocytes; 5%; Eosinophils; 1% and Basophils 0%); Platelets; 332*103/mm3. Serum ferritin was normal (138 ng/ ml). D-dimer was normal (100 ng/ml). CRP was borderline (0.6 g/ dl). LDH was normal (281U/L). SGPT was normal (39 U/L); SGOT was normal (42 U/L). Serum creatinine (1.3 mg/dl) and blood urea (41 mg/dl) were normal. Ionized calcium was slightly low; 0.9 mmol/L. The troponin test had still negative. A plain CXR film was done within 10 days of the presentation showing multiple central and paracentral round nodular ground-glass opacities (Figure 2A). The first chest CT without contrast was done within 10 days of the presentation showing multiple central and paracentral round nodular ground-glass opacities (Figure 2B). Chest CT without contrast was repeated within 12 days of treatment showing complete resolution of the above abnormalities. Nodular COVID-19 pneumonia with Wavy triple sign or Yasser’s sign and Movable phenomenon was the most probable diagnosis. Within 15 days of the above management; the patient finally showed nearly complete clinical; radiological; and laboratory improvement. The patient was continued on aspirin tablet (75 mg; once daily) for three months and calcium with vitamin D oral preparations for 2 weeks with follow-up. Further recommended cardiac chest; and endocrinal follow-up was advised.
Figure 2A: Plain CXR film was done within 10 days of the presentation showing multiple central and paracentral round nodular ground-glass opacities (lime arrows).
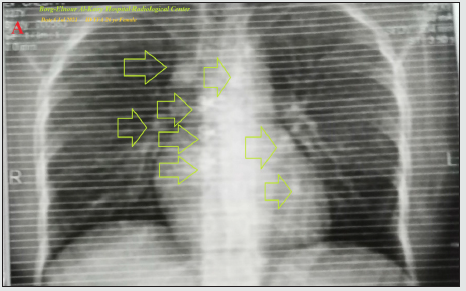
Figure 2B: Chest CT without contrast was done within 10 days of the presentation showing multiple central and paracentral round nodular ground-glass opacities (golden arrows).
Discussion
Overview
A young-aged housewife female COVID-19 thin patient presented to POC with nodular COVID-19 pneumonia; Wavy triple sign or Yasser’s sign; and Movable phenomenon.
The primary objective
For my case study was the presence of a patient with nodular COVID-19 pneumonia; Wavy triple sign or Yasser’s sign; and Movable phenomenon in POC.
The secondary objective
For my case study was the question of; How did you manage the case at home?
a) There was a history of direct contact to confirmed the COVID-19 case.
b) The presence of direct contact to confirmed the COVID-19 case; and bilateral nodular ground-glass consolidation on top of acute tachypnea will strengthen the COVID-19 diagnosis.
c) The tachypnea and electrocardiographic (ECG) Wavy triple sign or Yasser’s sign and Movable phenomenon are highly suggestive of associated hypocalcemia.
d) An early stoppage of prescribed medication without consultation of the manager doctor was the cause of reappearance of the symptoms and patient deterioration.
e) Cession of prescribed medications without return to the manager doctor was unreasonable.
f) Rapid return to the above-prescribed treatment regimen had improved the condition and saved the patient.
g) The dramatic reversal of clinical; electrocardiographic; and radiological after anticoagulants; antiplatelet; anti-infective drugs; and steroids had happened.
h) A nearly complete clinical; radiological; and laboratory improvement that occurred after the management of nodular COVID-19 pneumonia with anti-infective drugs; anticoagulants; steroids; and antiplatelet strongly implies their effects.
i) Mediastinal lymphadenopathy and metastatic carcinoma were the possible differential diagnosis for the current case study.
I can’t compare the current case with similar conditions. There are no similar or known cases with the same management for near comparison. The only limitation of the current study was the unavailability of echocardiography.
Conclusion and Recommendations
a) The nodular COVID-19 pneumonic presentation may be mimic metastatic carcinoma.
b) It signifies the role of anticoagulants; antiplatelet; antiinfective drugs; and steroids in COVID-19 patients with nodular COVID-19 pneumonia.
c) The presence of Wavy triple sign or Yasser’s sign and Movable phenomenon of hypocalcemia with a COVID-19 pneumonic patient was reasonable.
Conflicts Of Interest
There are no conflicts of interest.
Acknowledgment
I wish to thanks my wife to save time and improving the conditions for supporting me.
References
- Zhu N, Zhang D, Wang W, Xingwang Li, Bo Yang, et al (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382(8): 727-733.
- (2020) Coronavirus disease (COVID-19) Situation Report-165. WHO.
- Guiot J, Danthine D, Deprez L, Louis R, Lovinfosse P, et al (2020) [Chest radiological lesions in COVID-19:from classical imaging to artificial intelligence]. Rev Med Liege 75(S1): 81-85.
- Franquet T (2011) Imaging of pulmonary viral pneumonia. Radiology 260(1): 18-39.
- Pan Y, Guan H, Zhou S, Wang Y, Li Q, et al (2020) Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol 30(6): 3306-3309.
- Li X, Zeng X, Liu B, Yu Y (2020) COVID-19 infection presenting with CT halo sign. Radiol Cardiothorac Imaging 2(1): e200026-e200035.
- Yang Z, Shi J, He Z, Ying Lü, Qingnian Xu, et al (2020) Predictors for imaging progression on chest CT from coronavirus disease 2019 (COVID-19) patients. Aging (Albany NY) 12(7): 6037-6048.
- Hefeda M M (2020) CT chest findings in patients infected with COVID-19: review of literature. Egypt J Radiol Nucl Med 51: 239-248.
- Valette X, Du Cheyron D, Goursaud S (2020) Mediastinal lymphadenopathy in patients with severe COVID-19 [published online ahead of print, 2020 Apr 21]. Lancet Infect Dis 20(11): 1230-1238.
- Elsayed YMH (2019) Wavy Triple an Electrocardiographic Sign (Yasser Sign) in Hypocalcemia. A Novel Diagnostic Sign; Retrospective Observational Study. EC Emergency Medicine and Critical Care (ECEC) 3(12): 1-20.
- Elsayed YMH (2021) Movable-Weaning off an Electrocardiographic Phenomenon in Hypocalcemia (Changeable Phenomenon or Yasser’s Phenomenon of Hypocalcemia)-Retrospective-Observational Study. CPQ Medicine 11(1): 01-35.
- Elsayed YMH (2021) A COVID-19 extensive bilateral pneumonia, variants ischemic heart disease, and Movable-weaning phenomenon of hypocalcemia or Yasser’s phenomenon; dramatic reversal at home management. J Clin Images Med Case Rep 2(2): 1035-1041.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




