Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Editorial(ISSN: 2690-5760) 
Low Health Literacy (LHL) Facts Volume 5 - Issue 2
Abdul Kader Mohiuddin*
- Alumnus, Faculty of Pharmacy, Dhaka University, Bangladesh
Received:January 17, 2023; Published: January 30, 2023
Corresponding author: Abdul Kader Mohiuddin, Alumnus, Faculty of Pharmacy, Dhaka University, Bangladesh
DOI: 10.32474/JCCM.2023.05.000207
Abstract
In order to access, comprehend, and use information to make decisions about their health, people must possess certain personal traits and social resources, which are referred to as health literacy. Patients’ ability to engage in complex disease management and self-care is strongly related to their level of health literacy. It can help us stay healthy by preventing illness and effectively managing existing illnesses. Personal health literacy refers to a person’s ability to locate, comprehend, and apply information and services to support health-related decisions and actions for themselves and others. The World Health Organization recommends health literacy as a tool for achieving several key targets outlined in the Sustainable Development Goals. Low health literacy (LHL) is most commonly associated with mature patients with chronic health conditions who have limited education and are not necessarily from a lower income group. Furthermore, being literate in general does not imply being literate in health.
Keywords:Parental health literacy; necessary health education; understanding treatment guidelines; medication non-adherence; healthcare, avoidable medical costs, global health burden, COVID-19 vaccine neglegency
Introduction
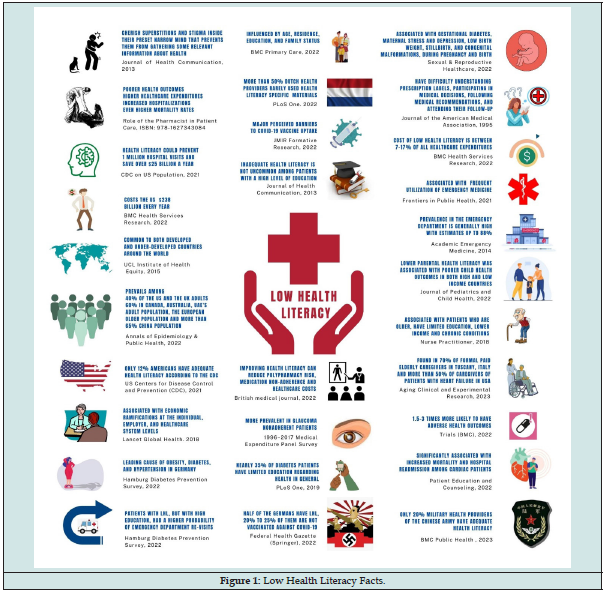
People with limited health literacy may find it difficult to manage their condition and prevent illness, which may lead to increased use of healthcare services. Furthermore, LHL is associated with increased hospitalizations, increased use of emergency care, decreased use of preventative services, and a worsened ability to understand labels and health messages, a worsened state of health, higher mortality, and more expensive medical care. Health literacy improves a population’s ability to care for themselves and aids in the reduction of health disparities. It has an impact on the use of health services, as well as on patient satisfaction and the physician-patient relationship. It is one of the major impediments to healthcare professionals adequately transmitting information to those under their care. Despite the negative implications of LHL, physicians are typically unaware of their patients’ health literacy levels and their subsequent effects on their patients’ outcomes (Figure 1).
Many studies reveal that patients from high-income countries are not adequately adhering to medications as they are prescribed. Forgetfulness, confusion about the duration required for medication use, and mistrust about the overall efficacy of medication are among the reasons for non-adherence to diabetes management protocols in Middle Eastern countries [1]. Conversely, after World War II, Taiwan faced severe poverty, but it is now the 8th largest economy in Asia and also the home of type 2 diabetes patients with more than 80% health literacy [2]. A cross-sectional study of 259 school leaders in Hong Kong carried out during the COVID-19 pandemic between April 2021 and February 2022 shows that more than 50% of participants had LHL, and their LHL was strongly associated with a negative attitude about vaccination, low information, and confusion about COVID-19-related information [3].
However, in this editorial, I would like to present a few more sensational facts in the form of an infographic model about LHL:
a) LHL is associated with people who cherish superstitions and stigma within their preset narrow mind, which prevents them from gathering relevant health information from their surroundings [4].
b) LHL has a significant impact on patients’ treatment guideline compliance, or, more directly, medication adherence, which leads to poorer health outcomes, higher healthcare costs, increased hospitalizations, and even higher mortality rates [5].
c) Only 12% of Americans have adequate health literacy, and improving health literacy could prevent nearly 1 million hospital visits and save more than $25 billion per year, according to the US Centers for Disease Control and Prevention (CDC) [6].
d) The global economic cost of illiteracy is estimated to be $1.19 trillion, but LHL alone costs the US economy $238 billion per year [7].
e) Both are found in both developed and developing countries around the world, and socioeconomic factors are not the only cause of LHL [8].
f) Surprisingly, nearly 40% of US and UK adults have LHL, compared to around 50% of Europeans, 60% of adults in Canada, Australia, and the UAE, and nearly 70% of Chinese [9].
g) In China, health literacy increased from 6.48% of the population in 2008 to 23.15% in 2020 [10]. However, only 1 in 5 military health providers of the Chinese People’s liberation Army had adequate health literacy, found in a recent survey published in BMC Public Health [11].
h) Evidence suggests that LHL has significant economic consequences at the individual, employer, and healthcare system levels [12].
i) The authors of the Hamburg Diabetes Prevention Survey, a population-based cross-sectional study in Germany, concluded that LHL is a significant risk factor for the metabolic syndrome’s three conditions: obesity, diabetes, and hypertension [13].
j) Age, place of residence, education, and family status all have an impact on health literacy [14].
k) More than half of Dutch health providers use health literacy-specific materials only infrequently [15].
l) Mistrust and LHL perceptions were linked to high levels of vaccine hesitancy, providing evidential support for portraying these factors as perceived barriers to COVID-19 vaccine uptake [16].
m) LHL is not uncommon among patients with a high level of education or with well-off patients. Moreover, patients with LHL, but with high education, had a higher probability of emergency department re-visits [7].
n) According to patient-centered interventions, improving health literacy can reduce the risk of polypharmacy, medication non-adherence, and healthcare costs [17].
o) According to the 1996-2017 Medical Expenditure Panel Survey (Cheng & Tanna, 2022), LHL was more prevalent in glaucoma patients, and patients with LHL were prescribed more medications and had higher medication costs [18].
p) Nearly 35% of diabetic patients worldwide have limited health-related education [19].
q) LHL is linked to gestational diabetes, maternal stress and depression, low birth weight, stillbirth, and congenital malformations during pregnancy and birth, all of which have negative consequences for the woman and her child [20].
r) Empirical research based on a conceptual model estimated that low health literacy costs between 7 and 17% of total healthcare expenditures [7].
s) The prevalence of LHL in the emergency department (ED) varies greatly, with estimates as high as 88% depending on the patient mix and screening instruments used [21].
t) In both low and high-income countries, low parental health literacy was linked to poorer child health outcomes [22].
u) Patients who are older, have less education, a lower income, and have chronic conditions are more vulnerable [23].
v) LHL was discovered in more than 70% of formal paid caregivers of non-self-supporting older adults in Tuscany, Italy, and in more than 50% of caregivers of heart failure patients in the United States [24].
w) People with low health literacy may have 1.5-3 times the number of serious health outcomes, such as higher mortality, hospitalization rates, and disease management ability, as those with adequate health literacy [25].
x) In cardiac patients, it has been linked to increased mortality, hospital readmission, and lower quality of life [26].
y) LHL represents nearly 50% of Germans [27]. In Germany, every fourth to fifth person is not immunized against COVID-19 [28].
z) According to a Waystar (Health Care Billing Software) report from 2019, nearly 40% of healthcare consumers were unaware that the cost of their healthcare varied across facilities [29].
Nonetheless, it goes without saying that health literacy is beneficial in addressing the health needs of even the most disadvantaged and marginalized communities. To improve adherence, patients need to clearly and appropriately understand health information related to their specific illness or disease. This understanding may be essential to helping patients generate the motivation, beliefs, and appropriate health behaviors needed to improve overall adherence. LHL is a curse; it has to be minimized. All healthcare providers, stakeholders, and even government and community authorities should work on it.
Acknowledgement
Dr. Rayhan A. Tariq, Drexel University College of Medicine for taking the time to review my paper and for his insightful comments.
For lending me books, journals, and newsletters, the seminar library of the University of Dhaka’s Faculty of Pharmacy and Bangladesh’s BANSDOC Library are also to be thanked.
Declarations
The current research was carried out exclusively to look into problems associated with low health literacy. With time and the availability of newer investigations in the same field, the statistical evidence or variables presented here may transform.
Funding
The author has not received any funds from any authority.
Author Contributions
The corresponding author is the sole contributor and the only author.
Conflicts of Interest
The author declares that he has no competing interests.
References
- Mohiuddin AK (2022) Medication adherence: Fact or fictions? Current Research in Public Health 2(1): 18-21.
- Lovrić B, Placento H, Farčić N, Metka Lipič Baligač, Štefica Mikšić, et al. (2022) Association between Health Literacy and Prevalence of Obesity, Arterial Hypertension, and Diabetes Mellitus. Int J Environ Res Public Health 19(15): 9002-9010.
- Lau SSS, Shum ENY, Man JOT, Ethan T H Cheung, Padmore Adusei Amoah, et al. (2022) COVID-19-Related Health Literacy of School Leaders in Hong Kong: A Cross-Sectional Study. Int J Environ Res Public Health 19(19): 12790-12795.
- van der Heide I, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, et al. (2013) The relationship between health, education, and health literacy: results from the Dutch Adult Literacy and Life Skills Survey. J Health Commun 18 Suppl 1(Suppl 1): 172-184.
- Mohiuddin AK (2020) Chapter 11. The Enigma of Patient Behavior. The Role of the Pharmacist in Patient Care: Achieving High Quality, Cost-Effective and Accessible Healthcare Through a Team Based, Patient-Centered Approach, Universal-Publishers pp. 189-210.
- (2021) US CDC. Health Literacy Basics-Talking points about health literacy. Centers for Disease Control and Prevention.
- Shahid R, Shoker M, Chu LM, Frehlick R, Ward H, et al. (2022) Impact of low health literacy on patients' health outcomes: a multicenter cohort study. BMC Health Serv Res 22(1): 1148-1152.
- (2015) UCL Institute of Health Equity/Public Health England. Local action on health inequalities-Improving health literacy to reduce health inequalities. UK Government Publishing Service, UK.
- Mohiuddin AK (2022) Low Health Literacy: Treacherous Foe of Patient Compliance in Developed Countries. A Epidemiol Public Health 5(2): 1097-1099.
- Li Y, Lv X, Liang J, Dong H, Chen C (2022) The development and progress of health literacy in China. Front Public Health 10(1): 1034907-1034910.
- Rong H, Lu L, Wang L, Cairu Liu, Ling Zhang, et al. (2023) Investigation of health literacy status and related influencing factors in military health providers of Chinese People's liberation Army, a cross-sectional study. BMC Public Health 23(1): 4-8.
- Kruk ME, Gage AD, Arsenault C, Keely Jordan, Hannah H Leslie, et al. (2018) High-quality health systems in the Sustainable Development Goals Era: Time for a revolution. The Lancet Global Health 6(11): e1196-e1252.
- Tajdar D, Schäfer I, Lühmann D, Regina Fertmann, Tim Steinberg et al. (2022) The Link Between Health Literacy and Three Conditions of Metabolic Syndrome: Obesity, Diabetes and Hypertension. Diabetes Metab Syndr Obes 15(1): 1639-1650.
- Šulinskaitė K, Zagurskienė D, Blaževičienė A (2022) Patients' health literacy and health behaviour assessment in primary health care: evidence from a cross-sectional survey. BMC Prim Care 23(1): 223-228.
- Murugesu L, Heijmans M, Rademakers J, Fransen MP (2022) Challenges and solutions in communication with patients with low health literacy: Perspectives of healthcare providers. PLoS One 17(5): e0267782-e0267785.
- Weerakoon SM, Henson Garcia M, Valerio Shewmaker MA, Messiah SE, Knell G (2022) Contributions of Trustworthiness, Health Literacy, and Self-Efficacy in Communicating With COVID-19 Vaccine-Hesitant Audiences: Web-Based Survey Study. JMIR Form Res 6(8): e38076-e38079.
- Shebehe J, Montgomery S, Hansson A, Hiyoshi A (2022) Low health literacy and multiple medications in community-dwelling older adults: a population-based cohort study. BMJ Open 12(2): e055117-e055119.
- Cheng BT, Tanna AP (2023) Association of Health Literacy and Healthcare Utilization Among Glaucoma Patients. J Glaucoma 32(2): 139-144.
- Abdullah A, Liew SM, Salim H, Ng CJ, Chinna K (2022) Prevalence of limited health literacy among patients with type 2 diabetes mellitus: A systematic review [published correction appears in PLoS One 17(1): e0261430-e0261435.
- Meldgaard M, Gamborg M, Maindal HT (2022) Health literacy levels among women in the prenatal period: A systematic review. Sexual & Reproductive Healthcare 34(1): 100796-100799.
- Griffey RT, Kennedy SK, McGownan L, Goodman M, Kaphingst KA (2014) Is low health literacy associated with increased emergency department utilization and recidivism? Academic Emergency Medicine 21(10): 1109-1115.
- Zaidman EA, Scott KM, Hahn D, Bennett P, Caldwell PH (2023) Impact of parental health literacy on the health outcomes of children with chronic disease globally: A systematic review. J Paediatr Child Health 59(1): 12-31.
- Hickey KT, Masterson Creber RM, Reading M, Robert R Sciacca, Teresa C Riga, et al. (2018) Low health literacy: Implications for managing cardiac patients in practice. Nurse Pract 43(8): 49-55.
- Lorini C, Buscemi P, Mossello E, Annamaria Schirripa, Barbara Giammarco, et al. (2023) Health literacy of informal caregivers of older adults with dementia: results from a cross-sectional study conducted in Florence (Italy). Aging Clin Exp Res 35(1): 61-71.
- Gan W, Zhang Q, Yang D, Jinyu Yin, Yujie Wang, et al. (2022) A behavior change wheel-based interactive pictorial health education program for hypertensive patients with low blood pressure health literacy: study protocol for a randomized controlled trial. Trials 23(1): 369-375.
- Kanejima Y, Shimogai T, Kitamura M, Ishihara K, Izawa KP (2022) Impact of health literacy in patients with cardiovascular diseases: A systematic review and meta-analysis. Patient Educ Couns 105(7): 1793-1800.
- Achstetter K, Köppen J, Haltaufderheide M, Hengel P, Blümel M, et al. (2022) Health Literacy of People with Substitutive Private Health Insurance in Germany and Their Assessment of the Health System Performance According to Health Literacy Levels: Results from a Survey. Int J Environ Res Public Health 19(24): 16711-16718.
- Bosle C, Orth B, Reibling N, Merkel C, Muschalik C, et al. (2022) [Health information behaviour and health literacy on COVID-19 vaccination of the general population in Germany-findings from the CoSiD study] Federal Health-Gazette Health-Research-Health Protection (Springer) 65(12): 1289-1298.
- O Mara CS, Young JP, Winkelmann ZK (2022) Financial Health Literacy and the Shared Decision-Making Process in Healthcare. Int J Environ Res Public Health 19(11): 6510-6515.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...