Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Review Article(ISSN: 2690-5760) 
Lessons from the Early Phase of the COVID-19 Pandemic: Prevalence, Risk and Protective Factors for Psychological Morbidity– Systematic Review Volume 2 - Issue 4
Suleman Bakhshi1, Harry Kyriazis2 and Meagan E Brennan1,3*
- 1University of Notre Dame, School of Medicine, Sydney, Australia
- 2University of New South Wales, Department of Exercise Physiology, Faculty of Medicine, Sydney, Australia
- 3University of Sydney, Westmead Clinical School, Faculty of Medicine and Health, Sydney, Australia
Received: January 22, 2020 Published: February 23, 2021
Corresponding author: Meagan Brennan, PhD, School of Medicine, The University of Notre Dame Australia, Sydney, Australia
DOI: 10.32474/JCCM.2021.02.000150
Abstract
The COVID-19 pandemic has had a devastating impact on psychological well-being globally. Study aims were to examine the extent of psychological morbidity and to identify risk and protective factors that could be targeted with interventions. A systematic review was performed using PRISMA guidelines. Studies reporting depression, anxiety and COVID-related fear were included. 30 studies (43,634 participants) were included. Anxiety prevalence was 6.3–34% and depression 14.6%–43.7%. Higher levels of anxiety, depression and/or COVID-related fear were found in women, younger people, rural residents, areas with high rates of COVID-19 and people with poor general health. Quarantine and feeling overwhelmed with negative information were risk factors for COVID-related fear. Protective factors were: comfortable amount of information, good social support’ and confidence in doctor. Health professionals had high rates of psychological morbidity.
Risk and protective factors were identified in this study. These could be targeted with COVID-specific public health support and interventions.
What we already know
a. The COVID-19 pandemic has had a devastating impact on psychological well-being globally.
b. Rates of anxiety and/or depression over 35% have been reported during the pandemic.
c. Responding to mental health issues is a priority area of public health policy.
What this article adds
a. Risk groups for psychological morbidity have been identified, including health professionals, young people, women, people affected by quarantine and those living in hot-spot and rural areas.
b. Protective factors have also been identified, including good family and social supports, positive coronavirus news feeds and confidence in doctors.
c. This information can be used to target strategies to support the mental health of communities affected by COVID-19.
Keywords: Anxiety; COVID-19; Depression; Fear; Mental health; Psychological distress
Introduction
As the COVID-19 pandemic progresses and cases pass 21 million worldwide [1,2], concern about its psychological morbidity as well as its physical devastation is increasing. It is unsurprising that the rapid spread of such a lethal disease from which humans have no immunity and to which global society is extremely vulnerable causes fear. The grief related to loss of life and loss of livelihood, along with the loss of freedom and loss of social connection caused by lock-down and quarantine recommendations have made life extremely challenging for many people. Health care workers are experiencing job security and are currently regarded by many as heroes; however, they are particularly vulnerable to psychological harm as they are witnessing trauma, working long hours, worrying about becoming infected themselves and have concerns about bringing disease home to their family members [3,4].
Rates of anxiety and/or depression over 35% have been reported in several studies during the pandemic [3-5]. Understanding more about the context of these studies, identifying who is most at risk and appreciating the type of psychological morbidity experienced during the COVID-19 pandemic will allow the development and implementation of targeted strategies to attempt to address this problem.
The aims of this study were to (1) examine the extent of psychological morbidity by documenting the prevalence of anxiety, depression and/or other mental illness in different populations (such as health professionals and general populations); and (2) to identify risk groups and protective factors that could be targeted with psychological interventions during the COVID-19 pandemic. The research question was ‘In populations affected by the early phase of the pandemic, what is the prevalence of mental illness and are there any risk or protective factors that can be identified to potentially reduce psychological morbidity?
Methods
The study was registered with PROSPERO (CRD42020186894) [6]. Searches of the OVID MEDLINE, PsycINFO and PubMed databases were conducted.Studies were tracked using PRIMA methods [7]. Data were extracted from eligible studies, and each was allocated a ‘risk of bias’category using a standardised critical appraisal tool for prevalence studies.9Further methodological detail is provided in on-line Appendix (Supplementary File).
Eligibility criteria for inclusion were: (1) primary studies published in peer-reviewed scientific journals AND (2) reportingprevalence of anxiety, depression, fear of COVID-19 or other mental health outcomes. Exclusion criteria were: (1) nonprimary studies (review articles, letters, correspondence, and abstract-only publications), AND (2) non-human studies. This review analysed the studies reporting anxiety, depression and COVID-19-related fear. Studies reporting other psychological outcomes were identified for future evaluation.
Results
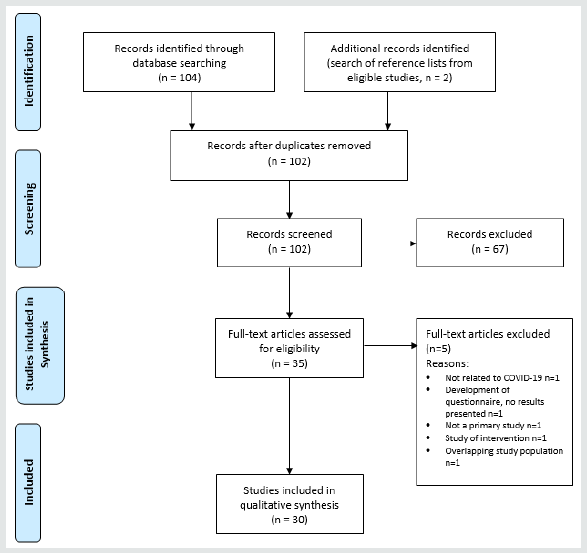
The initial search identified 104 studies; 33 abstracts met eligibility criteria. Two further studies were added from reference lists of eligible studies. Five studies were later excluded, leaving 30 for inclusion in data analysis. PRISMA flowchart [10] is shown in Figure 1. The study population, methodology, outcome measures and risk of bias score of eligible studies are shown in Table 1.
Study characteristics
The 30 eligible studies [3-5, 11-37] (Table 1) included assessment of psychological outcomes in 43,634 individual participants [3-5,11-37]. Studies were conducted between January and April 2020. They evaluated the main psychological outcomes of interest: general anxiety (22 studies) [3-5,11-14,16-22,24,25,28-30, 32,34,35], depression (14 studies) [3-5,12-14,16,17,19,21,22,28- 30,32] and COVID-19-related fear, anxiety and/or knowledge (10 studies) [4, 11, 17, 22, 30, 32].
Studies were conducted across six countries: China (22 studies), Spain (2 studies) [19,27], Italy (2 studies) [26 29], other (Iran [12], Israel [14], United Kingdom [13] and international [11], 1 study each). 18 studies were focused on general populations [4,5,12-14,18,19,22,23,26,27,29-32,36,37], ten on health professionals [3,11,15,20,21,24,25,28,33,35] and two on university students. [16,17] Most studies had a cross-sectional design, asking participants to self-administer an on-line questionnaire.
The risk of bias was ‘low’ in nine studies [12,16,17,21,22,25- 27,33], ‘medium’ in 15 studies [3-5,13,14,18-20,23,24,30-32,35,37] and ‘high’ in six studies [11,15,28,29,34,36]. Even in the studies where ‘risk of bias’ was low, none used random sampling of the population (for example from census data) to estimate prevalence. Therefore, these studies provide some insight into prevalence in individual, very defined groups but do not provide information about prevalence across the entire population (Table 1).
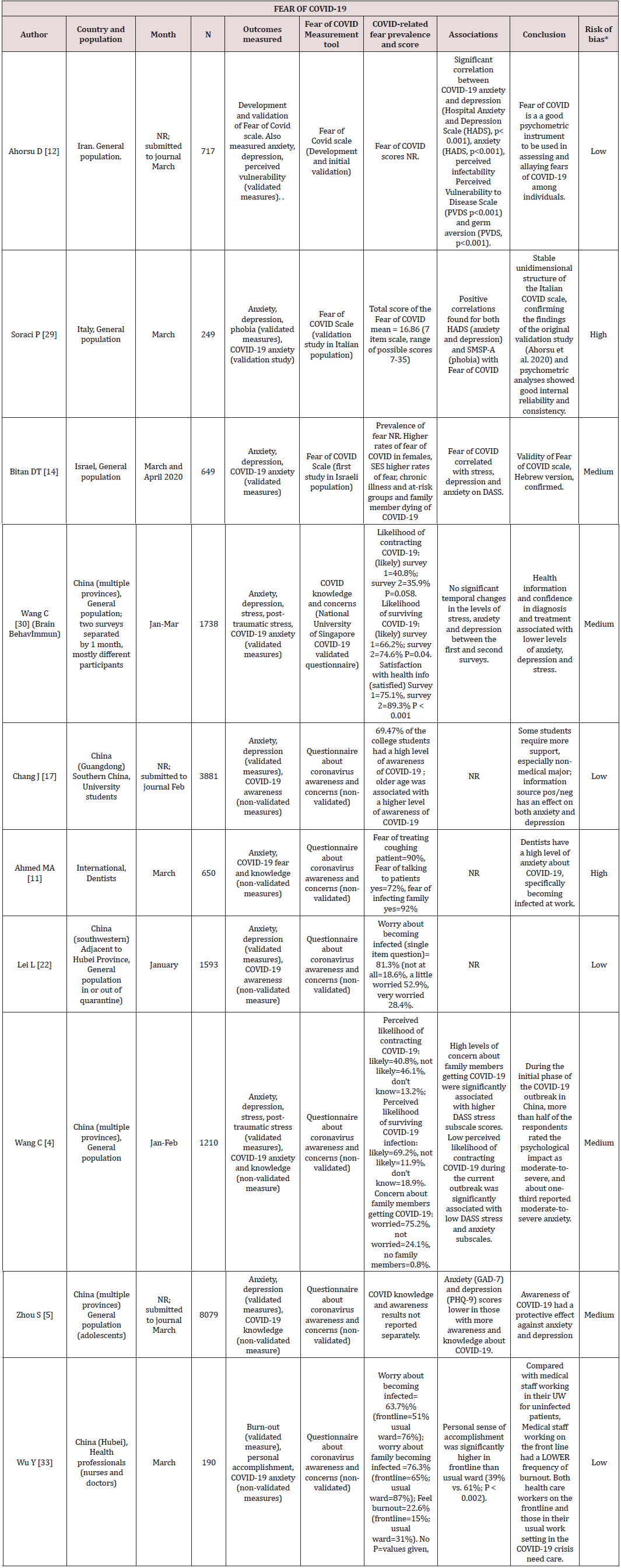
Table 1: Studies reporting psychological outcomes related to COVID-19 (n=30 studies, grouped by study population, and ordered by date of study).
NR- not reported. *Study by Yuan et al mixed population that included university students (66%). **Study by Chang et al mixed population of university students, health/medical students (86.6%)***Based on score derived using criteria by Joanna Briggs Institute (Reference: Joanna Briggs Institute. Critical Appraisal Instrument for Studies Reporting Prevalence Data [9].
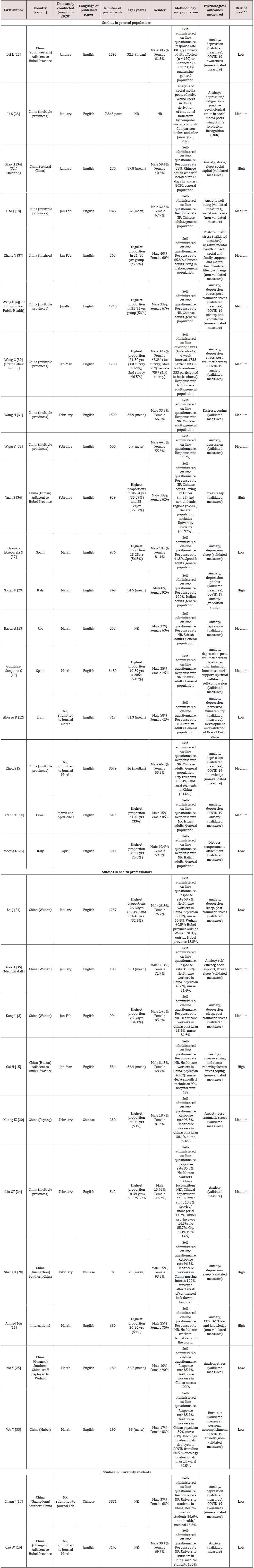
Anxiety
Twenty two studies reported anxiety (Table 2) [3-5,11-14,16- 22,24,25,28-30,32,34,35]. A variety of validated measurement tools were used: Zung Self-Rating Anxiety Scale (8 studies [20,22,24,25,28,32,34,35], General Anxiety Disorder Scale (GAD-7, 7 studies [3,5,13,16-18,21] and GAD-2, 1 study [19], Depression, Anxiety and Stress Scale (3 studies [4,14,30]), Hospital Anxiety and Depression Scale (2 studies [12,29]) and one non-validated questionnaire [11].
Table 2: Anxiety and depression related to COVID-19 (n=22 studies, grouped by measurement tool).

*Based on score derived using criteria by Joanna Briggs Institute [9].
There was heterogeneity in the reporting of anxiety prevalence and severity, with some reporting overall prevalence of ‘any level’ anxiety (mild, moderate or severe, 11 studies [4, 5,16-22,24,32]), and others reporting a mean anxiety score. In the studies reporting prevalence, three reported prevalence rates under 15%, all measured with SAS: 6.3% (study of 600 participants across China in February32), 8.3% (study of over 1500 participants in the general population in Wuhan in January [22]) and 12.5% (study of 512 health professionals across China in February [24]). All the remaining studies reported prevalence rates over 20%. These ranged from 21–27% (4 studies [16-18,20]) to the higher levels of 34% (study of over 8000 adolescents across China before March measured with GAD-7 [5]), 36% (study of over 1200 participants in the general population in Wuhan in January, measured with DASS-21 [4]) and 45% (study of over 1200 health professionals in Wuhan in January, measured with GAD-7 [21]). The highest quality studies reported prevalence rates of 8.3 [22], 24.9 [16] and 26.6% [17], representing results toward the middle of the overall range.
In 10 of the 11 prevalence studies, the proportion of mild, moderate and severe anxiety was also reported [3-5, 17,20-22,24,28,32]. The vast majority of participants had ‘mild’ anxiety and the higher-quality studies reported ‘mild’ anxiety in 21[16] and 23% [17]. The proportion in the ‘severe/high anxiety’ category was typically low. Seven of the 10 studies had a rate of severe anxiety in ≤2%, with the other 3 studies reporting 5% [21], 6% [14] and 8% [4].
Higher anxiety scores were reported in females in six studies [5, 19-22,32], in males in one study [31] with no difference in six studies [3, 16,18,19,24,28]. Younger age (<40 years) was associated with higher anxiety in three studies [3,18,32], and age had no effect in one study [24]. The exception to the younger age trend was the only study in adolescents, and this showed higher anxiety in older adolescents (senior high school years) than younger students [5].
In the studies of health professionals, nurses had higher anxiety levels than doctors in two studies [20,21], and no different in one study [3]. In China, anxiety was highest among workers in Wuhan and provinces adjacent to Hubei compared to other provinces, higher in front-line workers compared to others [21,24] and high in a population of nurses subject to hospital-based residential lock-down for work [28].
In the general population and students, associations with high anxiety levels were high stress and depression scores [12,14,29], poor sleep [34], poor self-perception of health [4,18,19,22,30], lower level of education [18,19], social media exposure [18], knowing someone with COVID-19 [16,19], living in Hubei province [5,18] or rural areas [5,16,17], affected by quarantine [22,34], economic loss [16,22] living alone/lonliness [16,19] Higher anxiety was reported where more than half of COVID-19 media information was negative [17] and self-perception of being 'over-informed' compared to ‘good’ or ‘not enough’ information [19].
Protective effects against anxiety were high ‘social capital’/ social support [19,34], spirituality [19],being employed [4], better ‘COVID awareness [5,14], higher education level [19], confidence in doctor’s ability to diagnose/ treat COVID-19 and perceived low likelihood of contracting/ dying from COVID-19 [30].
No trends emerged in prevalence rates between general and health professional populations, between times of studies (month) of studies, sizes of studies or measurement tools (Table 2).
Depression
Fourteen studies reported depression are (Table 2) [3-5,12-14,16,17,19,21,22,28-30,32]. A variety of validated measurement tools were used: Zung Self-Rating Depression Scale (three studies [22,28,30]), Patient Health Questionnaire (PHQ-9, four studies [3,5,17,21] and PHQ-2, one study [19]), Depression, Anxiety and Stress Scale (3 studies [4,14,30] Hospital Anxiety and Depression Scale (2 studies [12,29]), and Beck Depression Inventory II (one study) [13].
There was heterogeneity in the reporting of depression prevalence and severity, with some reporting overall prevalence of ‘any level’ depression (mild, moderate or severe, six studies [4,5,17,19,22,32]), and others reporting a mean or median depression score [13,21,28,30]. In the studies reporting prevalence, the reported rates were ≤21% in four studies [17,19,22,32], 30.3% (study of 1210 participants in general population in China in January/February [4]) and 43.7%(study of over 8000 adolescents across China) [5]. There was only one ‘low risk of bias’ study to report depression and this showed a prevalance of 14.6% [22].
In five of the six prevalence studies, the proportion of mild, moderate and severe depression was also reported [4,5,17,22,32]. In all of these studies, the majority of participants had ‘mild’ depression. The proportion in the ‘severe depression category was low, with the highest being 4.3% with severe depression in the same study in China that had an overall high prevalence of depression at 30.3% [4].
Females had higher prevalence of depression than males in five studies [5,17,19,22,30], lower in one [4] and no different in two [28,32]. Higher rate of depression was associated with younger age [19], financial loss [22], being affected by quarantine [22,30], drinking alcohol [17], rural residence [5], and personal poor health [4,22,30]. Higher level of education was a risk factor in one study [32] and a protective factor in two others [4,19]. In adolescents, depression was higher in the older high school age group [5]. Health professionals working on the front-line (versus ‘second-line’) had a higher rate of depression, as did those working in Wuhan (versus other provinces in China) and working in a secondary (versus tertiary) hospital [32].
Lower rates of depression were associated with industrial occupations (compared to professionals) [32], having more social support and higher ‘spiritual well-being [19], having confidence in doctor’s ability to diagnose COVID-19 and feeling likely to survive COVID-19 [30].
Receiving information about COVID-19 had an effect on depression; excessive negative information about COVID-19 was associated with a higher rate of depression [17] and feeling satisfaction with information about COVID-19 was associated with a lower rate of depression [30]. COVID-19 related fear was strongly correlated with depression in one study [29] and weakly correlated in another [14].
COVID-19-related anxiety and other outcomes
Ten studies reported COVID-19-related anxiety and/or knowledge (Table 3) [4, 11,17,22,30,32]. A new ‘Fear of COVID’ scale (seven-item Likert scale) was developed [12] then validated in general populations in Iran [12], Italy [29] and Israel [14]. It showed suitable properties for ongoing use [12]. Fear of COVID-19 was correlated with high levels of anxiety and depression measured by HADS [12,14] and DASS-21 [29]. The remaining seven studies used non-validated questionnaires to assess specific issues related to COVID-19. A study of medical professionals in China also showed that the biggest concern for doctors and nurses was being responsible for their family becoming infected [33].
The other psychological outcomes reported were: sleep disturbance(9 studies) [3,5,21,25,28,32,34-36], distress/post-traumatic stress (8 studies) [3,19,21,26,30,31,37], stress [15,25,24,35], social support [19,34,35], coping [15,31], vulnerability [12], attachment [26], self-efficacy [35], burnout [33] and spiritual well-being [19]. These outcomes were not analysed in detail in this review but were included in the analysis of anxiety, depression and fear of COVID-19 where they also reported these (Table 3).
Discussion
This study has examined the first 30studies assessing psychological outcomes from 43,634people around the world during the early stages of the COVID-19 pandemic. Studies were conducted between January and April and published by the end of May 2020. Most of the studies were in Chinese populations.
While it is expected that levels of anxiety and depression would be high in the early stages of a pandemic, the extent of the psychological morbidity found in this review was notable. The anxiety prevalence in this review was 6.3–34% overall [4,5,16-22,24,32], with severe anxiety in up to 8% of cases [22]. However, it should be noted that ideal methodology (random sampling of a population based on census or similar data) was not used in any studies. The higher quality studies reported prevalence rates of 8.3 [22] to 26.6% [17]. These rates are much higher than reported in studies of prevalence in normal Chinese populations of 4-6% [38,39,40], in pre-pandemic times. In this review, depression prevalence was 14.6%–30.3% in adult populations and 43.7% in the adolescent study [5], also much higher than the 7.0% reported in a normal Chinese population [41]. While the overall prevalence is high in this review, in 9 out of the 10 studies that reported severity, all were in the ‘mild’ category [4,5,17,20-22,24,28,32].
Populations at higher risk of anxiety and depression were identified. These include women [20,22,32], people in rural areas [5,16,17], those living in areas with high rates of COVID-19 (such as Hubei province) [18,21] or with a family member who has been affected by COVID-19 [16,19] and people with poor general health [4,30]. The negative impact of quarantine on psychological well-being has also been shown in this review [22,30], even in the very early stages of the pandemic. The identification of these risk groups can be used to target specific interventions. Examples of interventions could be the inclusion of family members in the support that is provided for people diagnosed with COVID-19. The specific exclusion of relatives from visiting patients in hospital due to concern about exposing them to infection will provide challenges to providing such support, however remote interventions could be used. People with poor general health are likely to be in contact with health providers, and this interaction for usual health care can be used as an opportunity to provide specific support for COVID-19 related fear and anxiety.
Protective factors were also identified in this review. The presence of a strong social/family network [19,34] was protective against psychological morbidity. Other protective factors were a comfortable level of COVID-19 awareness [5,14] and confidence in the health system to diagnose and treat COVID-19 [30]. These factors can be used in public health messaging to create a sense of security rather than panic around the disease.
Heath professionals, especially nurses [20,21], had high levels of psychological morbidity in this review. This is consistent with previous research that demonstrated anxiety prevalence over 26% in physicians [42] and 40% in nurses [43] in China in non-COVID times. Similarly high rates were found in Australian nurses, who had a prevalence of 32.4% for anxiety and 41.2% for depression [43]. Workers in front line positions during the epidemic may demonstrated high levels of anxiety and depression [21], however, workers in ‘less-front-line’ positions (such as those working in their normal oncology ward [33] and those in ‘secondary’ rather than ‘tertiary’ hospitals [21]) were also at risk. This may suggest that workers may feel they are well protected with personal equipment when working with COVID-19 patients or that they feel a sense of control or contribution that workers in other areas lack. Therefore, any strategies that target psychological well-being in health professionals must include all, and not just target workers in areas with a high number of COVID-positive patients. Strategies to address the fear that health professionals have of infecting their family members also need to be considered as this was one of their main causes of concern [11,33].
Information about COVID-19 emerged as a factor in both anxiety and depression. People who felt well-informed about the illness had lower levels of both anxiety and depression. However, a feeling of having ‘too much’ information, or having a majority of negative information about the illness was associated with higher levels. Also, high use of social media was a risk factor for psychological morbidity. This can be considered when public health programs are being developed. It may be possible to provide a limited amount of clear, concise and accurate information that can be repeated often, and to recommend that that people at risk of mental illness avoid using social media and new channels that may be providing a high proportion of ‘negative’ news stories rather than offering positive stories and hope. ‘Confidence in doctors’ emerged as a protective factor. It is possible, then, that a strong relationship with a GP can assist in the prevention of mental health problems and encouraging people to see their GP regularly is an important health message.
The strength of this study is the robust systematic review methodology, including PRISMA protocol, broad search strategy, pre-determined inclusion and exclusion criteria and data extraction/checking by two investigators. The limitations include the heterogeneity of the methodology of the included studies, contributed to by the broad inclusion criteria, precluding meta-analysis and limiting generalisable conclusions. The majority of studies were from China and this may limit the applicability of the results to Western countries. Also, as the included studies were conducted in the early part of the pandemic, the results may be less applicable to the current situation where there the world is more experienced in the management of the virus and people have longer experience with the challenges of lock-down. Further research is required to evaluate whether the psychological morbidity identified in this review increases or decreases over the duration of the pandemic.
Conclusions
Studies of psychological outcomes in the early months of the COVID-19 pandemic have demonstrated high levels of anxiety and depression in some populations and have identified risk groups. Women, young adults, older adolescents and people living in and outbreak epicentre are particularly vulnerable. Health professionals, whether or not they are working on the front line, are at risk of anxiety and depression. The quality and nature of information that people receive also has an effect on psychological outcomes and is an area that could be targeted to reduce morbidity.
References
- Medicine JHU (2020) COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Coronavirus Resource Centre.
- World Health Organization (2020) WHO Coronavirus Disease (COVID-19) Dashboard.
- Kang L, Ma S, Chen M, Jun Yang, Ying Wang, et al (2020) Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun87: 11-17.
- Wang C, Pan R, Wan X,Yilin Tan, Linkang Xu, et al. (2020) Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health17(5): 1729.
- Zhou SJ, Zhang LG, Wang LL, Zhao Chang Guo, Jing Qi Wang, et al. (2020) Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry 29(6): 749-758.
- National Institute for Health Research (2020). PROSPERO prospective register of systematic reviews.
- Liberati A, Altman DG, Tetzlaff J, Cynthia Mulrow (2009) The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med6(7):1000100.
- Joanna Briggs Institute (2020) Critical Appraisal Instrument for Studies Reporting Prevalence Data.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6(7): 97.
- Ahmed MA, Jouhar R, Ahmed N,Samira Adnan, Marziya Aftab, et al.(2020) Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int J Environ Res Public Health17(8):2821.
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, et al. (2020) The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict1-9.
- Bacon AM, Corr PJ (2020) Coronavirus (COVID-19) in the United Kingdom: A personality-based perspective on concerns and intention to self-isolate. Br J Health Psychol 25(4): 839-848.
- Bitan DT, GrossmanGiron A, Bloch Y, Mayer Y, Shiffman N, et al. (2020) Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Research289: 113100.
- Cai H, Tu B, Ma J, Limin Chen, Lei Fu, et al. (2020) Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan Between January and March 2020 During the Outbreak of Coronavirus Disease 2019 (COVID19) in Hubei, China. Med Sci Monit26:924171.
- Cao W, Fang Z, Hou G, Mei Han, Xinrong Xu, et al. (2020) The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res287:112934.
- Chang J, Yuan Y, Wang D (2020) Mental health status and its influencing factors among college students during the epidemic of COVID-19. Journal of Southern Medical University40(2):171-176.
- Gao J, Zheng P, Jia Y,Hao Chen, Yimeng Mao, et al. (2020) Mental health problems and social media exposure during COVID-19 outbreak. PloS one15(4):0231924.
- GonzalezSanguino C, Ausin B, Castellanos MA,Jesus Saiz, Aida Lopez Gomez, et al. (2020) Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 87: 172-176.
- Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP (2020) Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi38(3):192-195.
- Lai J, Ma S, Wang Y,Zhongxiang Cai, Jianbo Hu, et al. (2020) Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open3(3):203976.
- Lei L, Huang X, Zhang S, Yang J, Yang L, et al. (2020) Comparison of Prevalence and Associated Factors of Anxiety and Depression Among People Affected by versus People Unaffected by Quarantine During the COVID-19 Epidemic in Southwestern China. Med Sci Monit26:924609.
- Li S, Wang Y, Xue J, Zhao N, Zhu T (2020) The Impact of COVID-19 Epidemic Declaration on Psychological Consequences: A Study on Active Weibo Users.Int J Environ Res Public Health 17(6): 2032.
- Liu CY, Yang YZ, Zhang XM,Xinying Xu, QingLi Dou, et al. (2020) The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol Infect 148: 98.
- Mo Y, Deng L, Zhang L, Qiuyan Lang, Chunyan Liao, et al. (2020) Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag 28(5): 1002-1009.
- Moccia L, Janiri D, Pepe M,Luigi Dattoli, Marzia Molinaro, et al. (2020) Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: An early report on the Italian general population. Brain Behav Immun 87: 75-79.
- OzamizEtxebarria N, DosilSantamaria M, PicazaGorrochategui M, IdoiagaMondragon N (2020) Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica 36(4): 00054020.
- Sheng X, Liu F, Zhou J, Liao R (2020) Psychological status and sleep quality of nursing interns during the outbreak of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 40(3): 346-350.
- Soraci P, Ferrari A, Abbiati FA,Elena Del Fante, Rosanna De Pace, et al. (2020) Validation and Psychometric Evaluation of the Italian Version of the Fear of COVID-19 Scale. Int J Ment Health Addict1-10.
- Wang C, Pan R, Wan X,Yilin Tan, Lin kang Xu, et al. (2020) A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 87: 40-48.
- Wang H, Xia Q, Xiong Z,Zhixiong Li, Weiyi Xiang, et al. (2020) The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: A web-based survey. PloS one15(5): 0233410.
- Wang Y, Di Y, Ye J, Wei W (2020) Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med 26(1): 13-22.
- Wu Y, Wang J, Luo C,Sheng Hu, Xi Lin, et al. (2020) A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J Pain Symptom Manage 60(1): 60-65.
- Xiao H, Zhang Y, Kong D, Li S, Yang N (2020) Social Capital and Sleep Quality in Individuals Who Self-Isolated for 14 Days During the Coronavirus Disease 2019 (COVID-19) Outbreak in January 2020 in China. Medical Science Monitor 26: 923921.
- Xiao H, Zhang Y, Kong D, Li S, Yang N (2020) The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit 26: 923549.
- Yuan S, Liao Z, Huang H,Boyue Jiang, Xueyan Zhang, et al. (2020) Comparison of the Indicators of Psychological Stress in the Population of Hubei Province and Non-Endemic Provinces in China During Two Weeks During the Coronavirus Disease 2019 (COVID-19) Outbreak in February 2020. Med Sci Monit 26: 923767.
- Zhang Y, Ma ZF (2020) Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int J Environ Res Public Health17(7): 2381.
- Ying DG, Jiang S, Yang H, Zhu S (2010) Frequency of generalized anxiety disorder in Chinese primary care. Postgrad Med 122(4): 32-38.
- Yu W, Singh SS, Calhoun S, Zhang H, Zhao X, et al. (2018) Generalized anxiety disorder in urban China: Prevalence, awareness, and disease burden. J Affect Disord 234: 89-96.
- Phillips MR, Zhang J, Shi Q,Zhiqiang Song, Zhijie Ding, et al. (2009) Prevalence, References, and associated disability of mental disorders in four provinces in China during 2001-05: An epidemiological survey. The Lancet 373(9680): 2041-2053.
- Shen YC, Zhang MY, Huang YQ,Yan Ling He, Zhao Rui Liu, et al. (2006) Twelve-month prevalence, severity, and unmet need for References of mental disorders in metropolitan China. Psychological Medicine 36(2): 257-267.
- Gong Y, Han T, Chen W,Hassan H Dib, Guoan Yang, et al. (2014) Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: A Cross-sectional study 9(7): 103242.
- Gao YQ, Pan BC, Sun W, Wu H, Wang JN, et al. (2012) Anxiety symptoms among Chinese nurses and the associated factors: A cross sectional study. BMC Psychiatry 12: 141.
- Maharaj S, Lees Ty, Lal S (2018) Prevalence and Risk Factors of Depression, Anxiety, and Stress in a Cohort of Australian Nurses. Int J Environ Res Public Health 16(1): 61.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...