Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Research ArticleOpen Access 
Knowledge & Attitude Towards Home Based Dialysis Therapy in Myanmar: The Way Forward! Volume 5 - Issue 2
Khin Phyu Pyar1*, Moe Zaw Myint2, Moe Htun Zaw3, Aung Phyoe Kyaw4, Kyaw Thu Yein Lwin3, Lay Maung Maung3, Ye Min Hein3, Lynn Htet Aung3, Myo Maung Maung3, Sai Aik Hla2, Soe Win Hlaing2, Aung Aung2, Zar Ni Htet Aung4, Nyan Lin Maung4, Soe Min Aung4, Thurein Win4, Han Lin Aung4, Kyaw Thet Maung4, Sai Su Phone4, Kyaw Zay Ya4, Zay Phyo Aung4, Myo Thant Kyaw4, Zaw Lin Oo4, Sit Min4, Htet Paing Aung4 and Thein Aung Moe4
- 1Professor and Head/ Senior Consultant Physician and Nephrologist, Department of Medicine/Nephrology, Defence Services Medical Academy/ No. (1) Defence Services General Hospital (1000-Bedded), Yangon, Myanmar
- 2Senior Consultant Physician, No. (1) Defence Services General Hospital (1000-Bedded), Yangon, Myanmar
- 3Consultant Nephrologist, Department of Nephrology, No. (1) Defence Services General Hospital (1000-Bedded), Yangon, Myanmar
- 4Consultant Physician, No. (1) Defence Services General Hospital (1000-Bedded), Yangon, Myanmar
Received: April 11, 2023 Published: April 25, 2023
Corresponding author: Khin Phyu Pyar, Professor and Head/ Senior Consultant Physician and Nephrologist, Department of Medicine/ Nephrology, Defence Services Medical Academy/ No. (1) Defence Services General Hospital (1000-Bedded), Yangon, Myanmar
DOI: 10.32474/JCCM.2023.05.000210
Abstract
Background: Home based dialysis therapy (HBDT) either CAPD (continuous ambulatory peritoneal dialysis) or home hemodialysis (HHD) is used for patients with ESRD (end stage renal disease) as renal replacement therapy. At present, in center hemodialysis (HD) is the main treatment option for patients with ESRD in Myanmar; the program on HBDT should be launched in future. This study aimed to explore the knowledge and attitude among patients attending in-center HD towards home based dialysis therapy (HBDT).
Methods: A cross-sectional descriptive study was conducted in February 2023 among patients on maintenance HD (MHD) at selected public hospitals in Myanmar. Data were collected by using standardized forms and analysis was done.
Results: This study involved 158 patients made up of 74 (46.8%) males and 84 (53.2%) females with a mean age of 50.52 ± 12.41 years. Duration of HD ranged from 3 months to 168 months. Most of the patients, 61.4% (97/158), were doing HD free of charge. Knowledge on home HD (HHD) was very low. Regarding CAPD, 67% (105/165) did not hear about it; only 6% (9/165) knew clearly. One fourth 27.85 % (44/165) just heard. The knowledge on CAPD was very low. Those who knew CAPD (6%) thought that the obstacles in CAPD were PD solution, PD catheter related problems, caregiver expertise, not having health care worker during HD and electricity. They knew the shortage of PD solutions which were imported from neighboring country. The advantages of home-based dialysis therapy over in-center dialysis were as follows: it did not impact occupation (95%); it saved travelling time and travel cost 94 (59.5 %). The majority (80%) knew that chances of getting COVID-19 infection from hospital environment was higher than home. Ninety-seven percent of them wanted to carry on in-center HD and less than 5% of them would change to HBDT/CAPD if opportunity were favorable with low cost. The preference between HHD and CAPD was not clear as less than 10% knew CAPD. Seventy percent of them wanted to learn about CAPD.
Conclusions: Majority of them had poor knowledge on HBDT and they knew that the hospital environment was high risk for infection like COVID-19. Their knowledge on advantages of HBDT over in-center HD was good. Their attitude to CAPD training was good. However, reluctancy to do HBDT showed their dependence on health care worker both physically and psychologically. It may be solved by practical training on HBDT and behavior therapy.
Keywords: Home based dialysis therapy (HBDT); CAPD (continuous ambulatory peritoneal dialysis); Home hemodialysis (HHD); ESRD, renal replacement therapy (RRT); knowledge; attitude
Introduction
Chronic kidney disease (CKD) is a global problem that causes significant burden not only to the healthcare system but also to patients and their family [1]. CKD is a progressive condition; about 10 % of the general population suffer from CKD [2] and 5 % of them need RRT. An estimated 2–7 million people with kidney failure worldwide die prematurely as they do not have access to kidney replacement therapy (dialysis or transplantation) (WHO). The number of people who were on kidney replacement therapy exceeded 3 million in 2017 and is projected to grow to 5·4 million by 2030 (the Lancet). ESRD is causing challenges for both patient and their family as well as the government. The population of Myanmar is 55 million and the number of chronic kidney disease is expected to be 5 million; the number requiring RRT would be 2.5 million. As living donor renal transplant is limited in Myanmar; renal replacement therapy either HD or CAPD can contribute to numerous clinical benefits. RRT as maintenance hemodialysis has been initiated in Myanmar since 1970 in Government hospital with one machine. Later, the number of HD machines and Hemodialysis Centers (HDC) increased gradually. In private sector, HD was launched in 1996. Peritoneal dialysis (PD) was first use in Myanmar in 1970 particularly for acute kidney injury.
Hemodialysis (HD) was first used in Myanmar as a treatment option for ESRD. The number of HD centers have been increasing. Regarding the location of HD centers, there were at least one center per State or Division as Myanmar has 14 State and Divisions. The number of HD centers increased dramatically over 20 years; some are run by public and some by private. However, they were situated mainly in major cities. Nearly 98% of cases on MHD were doing in-center HD in Myanmar [3]; the number on HHD was less than 10 cases. The reports mentioned that equity of access to dialysis facilities was not easy even in developed countries [4]. Hemodialysis, which is capital intensive to set up and requires infrastructures and facilities such as electricity, intense water consumption and buildings, seems to have upstaged peritoneal dialysis both in demand and supply. In developing countries, the cost of one session of HD in-center was 30-35 USD; it rose to 40-45 USD if transport charges were included. In Myanmar, the number of patients on HHD was less than 10; on the other hand, the number on continuous ambulatory peritoneal dialysis (CAPD) was less than 100 in the whole country. Being developing country, it was not easy to get in-center HD in recommended dose-3 time per week. Moreover, the cost of injection erythropoietin was 10 USD per dose [3]. This study aimed to explore the knowledge and attitude among patients on in-center maintenance hemodialysis (MHD) towards home based dialysis therapy (HBDT).
Methods
Study design and population
A cross-sectional descriptive study was conducted in February 2023 in selected public Hemodialysis Centers (HDC): Yangon (lower part of Myanmar), Nay Pyi Taw (central part of Myanmar), and Aung Ban (Eastern part of Myanmar). Data was collected by using standardized forms and analysis was done.
Operational definitions
Maintenance hemodialysis (MHD) was defined as hemodialysis done either twice a week or three times a week for more than two months in patients with end stage renal disease. Duration of maintenance hemodialysis was defined as total duration since first HD. End stage renal disease was defined as patients with chronic kidney disease stage 5. Cost of HD was defined the average amount of money need to be given by patient for each HD. Travel time to HD center was defined as the duration of total travel time from the patient’s residence to HDC which included the waiting time for public transport. Travel cost was defined the average amount of money used for travelling from their residence to HD center and both private and public transport were included. Cost of injection erythropoietin was defined as average amount of money to buy for one vial of erythropoietin irrespective of different brand.
Knowledge on machine related obstacles like HD machine, dialysate solution, RO water, electricity, power generator, and disposal of waste was acquired by ‘Yes or No’ question. Knowledge on man-related obstacles like needle insertion, monitoring, and adjusting flow rate was acquired by ‘Yes or No’ question. Knowledge on money related materials like cost for machine and consumables was acquired by ‘Yes or No’ question. Knowledge on emergency handling during HD like hypotension, hypertension, cramps, sweating, and giddiness was acquired by ‘Yes or No’ question. Knowledge and possible obstacles on CAPD such as PD solution, PD catheter related problems, caregiver expertise, not having health care worker during HD, electricity and sustainability was acquired by ‘Yes or No’ question. The advantage of home dialysis over incenter dialysis was acquired by ‘Yes or No’ question. The infectivity risk of COVID-19 infection in home dialysis over in-center dialysis, their preference between in-center HD and HBDT and preference between HHD and CAPD, and their willingness to training on CAPD) were acquired by ‘Yes or No’ question.
Data Collection and Procedure
cross-sectional hospital based descriptive study was conducted among patients doing in-center dialysis at government hospital; they were interviewed by physicians and nephrologists using structured questions in February 2023. The timing of interview was end of HD session. The questions were based on key 7 elements. First was related with baseline characteristics (age, sex, duration of HD, cost of HD, travel time, travel cost, cost of injection erythropoietin). Second was knowledge on home HD (HHD) such as machine related obstacles like HD machine, dialysate solution, RO water, electricity, power generator, disposal of waste; manrelated obstacles like needle insertion, monitoring, adjusting flow rate; money related like cost for machine and consumables; and emergency handling during HD like hypotension, hypertension, cramps, sweating, giddiness. Third portion was knowledge and possible obstacles on CAPD such as PD solution, PD catheter related problems, caregiver expertise, not having health care worker during HD, electricity and sustainability. Fourth part was the advantage of home dialysis over in-center dialysis. Fifth element was infectivity risk of COVID-19 infection in home dialysis over in-center dialysis; sixth was their preference between in-center HD and HBDT and preference between HHD and CAPD. Seventh/ Last part was their willingness to training on CAPD). The data were checked by two medical officers and then, supervision, completeness, and consistency of collected data were performed by the principle investigator. Data were collected by using standardized forms and analysis was done.
Statistical Analysis
The collected data were entered into Microsoft Excel 2016 and exported to IBM SPSS Statistics for Windows, Version 23.0 (Armonk, NY: IBM Corp) for analysis. Descriptive statistics were presented as frequency and percentage for categorical variables and mean (standard deviation, SD) for continuous variables.
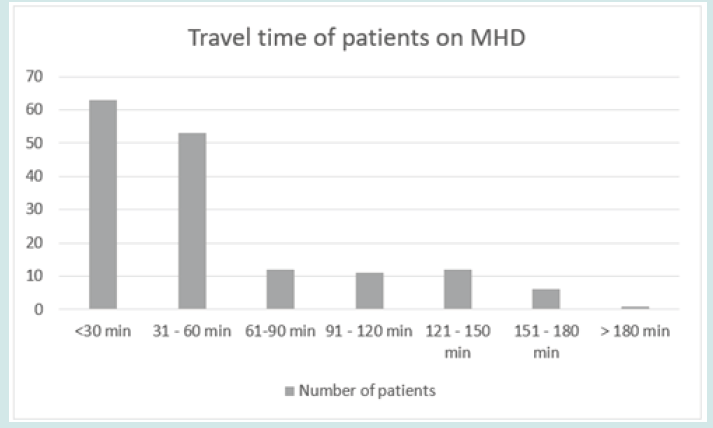
Results
A cross-sectional descriptive study was conducted in February 2023 among patients on MHD at selected public hospitals in Myanmar. This study involved 158 patients made up of 74 (46.8%) males and 84 (53.2%) females with a mean age of 50.52 ± 12.41 years. Duration of HD ranged from 3 months to 168 months. Most of the patients, 61.4% (97/158), were doing HD free of charge; however, 25% (40/158) had to share cost for tubing and dialyzer (10 USD per session). The travelling time ranged from less than 30 minutes to more than 3 hours. Cost of erythropoietin was 10 USD per one vial. Knowledge on home HD (HHD) such as machine related obstacles like HD machine, dialysate solution, RO water, electricity, power generator was very low as they only knew the cost per HD session in private HD center. Their opinion on man related obstacles like needle insertion, monitoring the whole process, adjusting flow rate and saline flush were absolutely impossible at home because they did not have close health care workers at home. Even after training, they were very reluctant to do needle placement by their selves. The cost for HD machine and related consumables were not known too; however, the cost was cheaper if the dialyzer was reused. The disinfection and sterilization process of reusable dialyzer was not easy too. They did not have any ideas on handling emergency problems during HD like hypotension, hypertension, cramps, sweating, giddiness.
Regarding CAPD, 67% (105/165) did not hear about it; only 6% (9/165) knew clearly. One fourth 27.85 % (44/165) just heard. Less than 10 patients on MHD knew CAPD. Those who knew CAPD thought that the obstacles were shortage of PD solution 81.6%, difficulty in supply of RO water 67.1%, PD catheter related problem 66.5%, expertise of care giver 57%, electricity problem 45% and not having health care worker during PD 42.4%. They knew the main problem was PD solutions as they were imported from neighboring country. uncertainty on sustainability. Their knowledge of advantages of home-based dialysis therapy over incenter dialysis was excellent; it did not impact occupation (95%); it saved travelling time and travel cost 94 (59.5 %). The infectivity risk of COVID-19 infection in home dialysis over in-center dialysis was ‘majority (80%) knew that chances of getting COVID-19 infection from hospital environment was higher than home; home dialysis could prevent infection 55.1 % (87/165)’. Their preference between in-center HD and HBDT was ‘97% (151/165) wanted to carry on in-center HD and less than 5% of them would change to HBDT/CAPD if opportunity were favorable with low cost’. The preference between HHD and CAPD was not clear as less than 10% knew CAPD. Half of them desired for HHD in their dream. The willingness to get training on CAPD was recorded in only seventy percent of them; they wanted to learn about CAPD.
Discussion
There are 14 States and Divisions in Myanmar. Seven States occupy hilly regions where they are less populated: Shan State, Kachin State, Chin State, Rakhine State, Kayah State, Kayin State and Mon State. Seven Divisions are non-hilly areas; thus, they are densely populated: Yangon Division, Naypyitaw Division, Mandalay Division, Sagaing Division, Bago Division, Magway Division and Irrawaddy Division. Current total population in Myanmar is 55.39 million (Myanmar Population Clock); and it is 53.4 million in 2017. As ESRD population is growing, most of the countries are facing big economic issue for RRT. Tackling dialysis burden around the world is a global challenge; therefore, it would be more challenging in developing countries. It was not easy to invest most of the budget for RRT. On the other hand, the number of health care workers was not enough to run HD center. Therefore, all cases of ESRD could not get access to RRT for various reasons even in developed countries. Therefore, in this study 25% patients had to share the cost to support material shortage. However, it was less than one third of cost in private hospital. It could explain the cost for erythropoietin too. In view of transport expense, 1-10 USD for each HD, the price of fuel was rising trend world-wide. To maintain long term HD, the accessibility is the main issue in government HD centers. The longer travel time caused poor adherence to HD. In this study, 75% of patients had acceptable time of 60 minutes and below. For the remaining 25%, either new HD center or HBDT was recommended. CAPD (continuous ambulatory peritoneal dialysis) would be better than home hemodialysis (HHD) in resource poor setting [3]. One report mentioned that cost of PD was less than, or at least as expensive as HD [5]. The study from Australia identified the importance of financial hardships though HDC were supported by government [6]. Socio-economic equity was emphasized in findings from Indonesia study; higher frequency of hemodialysis use wes directly affected by higher family income, distance < 20 km, working in informal sector, beneficiary of government subsidy, longer duration of hemodialysis, severe condition of illness, and living in urban area [7].
Study from both France and UK highlighted the importance of travel time to HDC [8,9]. The researchers from Australia found that geographical barriers were important in long term adherence [6]. Half of the patients required an hour travel time to HDC. The findings from United Kingdom pointed out that the adherence to treatment, hemodialysis, was inversely proportionate with travel time; they also recommended to build a new HDC if travel time was more than 45 minutes (Figures 1-3). Therefore, we need more HDC and human resources. Reallocation of man, materials and money to kidney health by modification of health policy should be done; same suggestions by other study [10]. The role of policies was the main key player in achieving equity in dialysis care and outcomes. Tackling dialysis burden around the world was a global challenge [11]. Therefore, we need more HDC and human resources. If possible, home based dialysis therapy (HBDT) should be launched. Non-medical reasons that influence PD utilization were reported as HD availability, number of HD center, distance to HDC, availability of dialysis partner, structure of dialysis program, PD experience, attitude towards home-based dialysis therapy (HBDT), and attitude towards chronic disease [12]; therefore, shared decision with the patient for choosing in-center HD or HBDT was the best option. However, the study from Switzerland showed that the majority love in-center hemodialysis.
Figure 2: Various transportation cost (MMK) for each HD session of patients on MHD (MMK= Myanmar Kyats) (3,000 MMK= 1 USD).
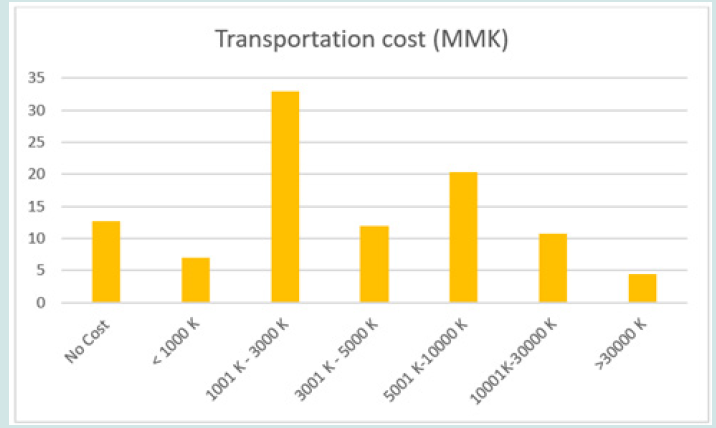
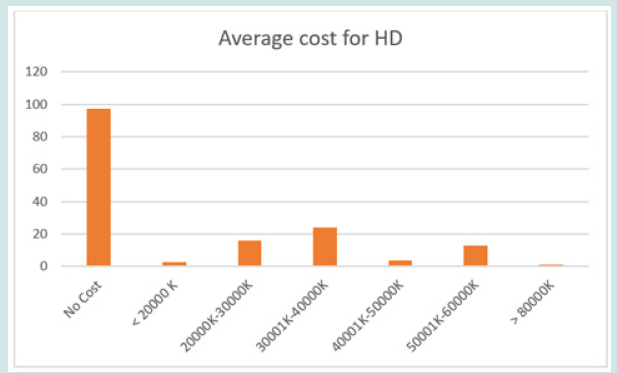
Figure 3: Cost (MMK) for each HD session of patients on MHD (MMK= Myanmar Kyats) (3,000 MMK= 1 USD).
Knowledge on home HD (HHD) such as machine related obstacles like HD machine, dialysate solution, RO water, electricity, power generator was very low as they only knew the cost per HD session in private HD center. It was not strange because the patients were not direct buyer of machine. It was the job of owner either government or private hospital. As the training program for HBDT (HHD or CAPD) was not launched in Myanmar, having limited knowledge on HBDT (HHD or CAPD) was not surprising. Knowledge and attitude on HBDT were significantly improved through web based education [13]. Therefore, to improve their knowledge, education program is urgently needed. Their opinion on man related obstacles like needle insertion, monitoring the whole process, adjusting flow rate and saline flush were absolutely impossible at home because they did not have close health care workers at home. Even after training, they were very reluctant to do needle placement by their selves. It was sensible as the patients were non-medics. One third of normal population had needle phobia. The study in Iran pointed out that health education (group discussion and teach-back self-care education) on the knowledge, attitude, and performance of hemodialysis patients had significant improvement. The cost for HD machine and related consumables were not known too; however, the cost was cheaper if the dialyzer was reused. The disinfection and sterilization process of reusable dialyzer was not easy too. It was acceptable that thorough disinfection and sterilization process required proper training to get real practice. They did not have any ideas on handling emergency problems during HD like hypotension, hypertension, cramps, sweating, giddiness. It could be handled with improvement in telemedicine and health system.
Regarding CAPD, only 6% (9/165) knew clearly and one fourth 27.85 % (44/165) just heard. Less than 10 patients on MHD knew CAPD. The reports proved that the knowledge on CAPD could be promoted by workshops, hands-on training [14] and web teaching [13]. The study done in Brazil showed that socioeconomic conditions were related to knowledge, attitudes, and practice by caregivers of children and adolescents with chronic kidney disease undergoing hemodialysis or peritoneal dialysis (Batista et al., 2016). In this study, 25% were graduates and half were unemployed. It was hard to agree with the study from Brazil because the total number of patients on CAPD in Myanmar was less than a hundred in whole population. Current total population in Myanmar is 55.39 million (Myanmar Population Clock); and it is 53.4 million in 2017. The number of ESRD cases requiring HD was approximately 2.5 million. CAPD program was not developed yet. Those who knew CAPD had good thought on obstacles; shortage of PD solution 81.6%, difficulty in supply of RO water 67.1%, PD catheter related problem 66.5%, expertise of care giver 57%, electricity problem 45% and not having health care worker during PD 42.4%. They knew the main problem was PD solutions as they were imported from neighboring country. uncertainty on sustainability. The problem should be solved at ministry level; Ministry of Health, Ministry of Electricity.
They knew very well about the advantages of home-based dialysis therapy over in-center dialysis; impact on occupation, travelling time and travel cost. The fact that chances of getting COVID-19 infection from hospital environment was higher than home was excellent as they had experienced on COVID-19 infection in recent pandemics. Their preference between in-center HD and HBDT was strange as 97% wanted to carry on in-center HD and less than 5% of them would change to HBDT/CAPD if opportunity were favorable with low cost. It showed both physical dependence and psychological dependence on health care workers and hospital. The study from Germany confirmed that the importance of personal attitude of patients and uptake of CAPD; making commitment for their treatment decision responsibility for their dialysis [15]. Another study done in early mentioned the relationship exists between the psychosocial characteristics of the CAPD patient and the occurrence of infectious complications [16-20]. Therefore, education program which could change the knowledge as well as attitude of the patients should be initiated prior to implementation of HBDT in Myanmar. The preference between HHD and CAPD was not clear as less than 10% knew CAPD. Half of them desired for HHD in their dream. The willingness to get training on CAPD was recorded in only seventy percent of them; they wanted to learn about CAPD. Non-medical reasons that influence PD utilization were reported as HD availability, number of HD center, distance to HDC, availability of dialysis partner, structure of dialysis program, PD experience, attitude towards home-based dialysis therapy (HBDT), and attitude towards chronic disease [12]; therefore, shared decision with the patient was the best option. However, the study from Switzerland showed that they favored in-center hemodialysis. It was influenced by national policy.
Limitation of Study
There are several limitations in this study. The sample size was small as it was conducted in three Government HD centers. The analysis would be better if larger number of patients as well as number of HDC were included. Moreover, only government funded centers were included in the study as the doctors from private HDC did not give informed consent. The socioeconomic status may be different from that of private center. It is clear that the cost of one session of HD in the private center is expensive- USD 50. And the government servant cannot afford to do HD in private center. Though the travelling distance was constant, the travel time was variable. The waiting time for public transport (bus) varied from 20 to 30 minutes unlike the transport system in developed countries. Moreover, inflation status determined the consumables like dialyzer, tubing, erythropoietin injection and dialysates [21-23].
Conclusions
The need for transition to HBDT exists and a good strategic plan to improve knowledge about and to prepare for HBDT is required [24-27]. Majority of them had limited knowledge on HBDT and they knew that the hospital environment was high risk for COVID-19 infection. Their knowledge on advantages of HBDT over in-center HD was good. However, reluctancy to do HBDT showed their dependence on health care worker both physically and psychologically. It may be solved by practical training on HBDT and behavior therapy. Their attitude to CAPD training was good [28-30].
Recommendations
To improve accessibility to HD, new HDC is required if travel time is more than 60 minutes. On the other hand, HBDT with reasonable price should be second option [31-33]. As CAPD is relatively cheaper than HHD, expansion of CAPD program should be done at ministry level. Transport and communication services should be promoted. Sustainability of dialysis fluids, tubing and dialyzer should be maintained. To promote affordability, dialyzers and dialysis solutions should be produced locally to cut down the costs of hemodialysis and CAPD. To improve knowledge and attitude on HBDT, web based education program are recommended [13]. Implementation of HBDT at national level is essential like making policy for HBDT, social security measures and reimbursement rates. It should be followed by implementation at regional level (preand post-graduate education to doctors and medics) and unit or township level (education and communication, logistics) [34-36].
Acknowledgment
We are thankful to Professor Ko Ko Lwin, Professor Kyaw Zay Ya, Directorate of Medical Services; Professor Myint Zaw (Yangon HDC), Professor Aung Myat Kyaw (NayPyi Taw HDC), Professor Myo Thant, Professor Saw Yan Naing for their administrative support & Professor Tin Moe Mya for laboratory support. We are also grateful to all patients and health care personnel included in this study.
Ethical Consideration
The data collection using standardized case report forms was approved by Hospital Ethics Review Committee of Defence Services General Hospital, Mingaladon. Informed consent was taken from both patients and their attending nephrologists and physicians. Privacy and confidentiality of information was maintained throughout the study process.
Conflict of Interest
There was no COI.
Funding
No funding was obtained.
References
- (2020) Global, regional, and national burden of chronic kidney disease, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England) 395(10225): 709-733.
- Kovesdy CP (2022) Epidemiology of chronic kidney disease: An update 2022. Kidney International Supplements 12(1): 7-11.
- Pyar KP (2022) Equity of Maintenance Hemodialysis in Myanmar: Cross-Sectional Descriptive Study. Journal of Biomedical Research & Environmental Sciences 3(9): 1045-1053.
- Richard JB, Aldigier JC, Le Mignot L, Glaudet F, Ben Said M, et al. (2009a) Equity of accessibility to dialysis facilities. Studies in Health Technology and Informatics 150(1): 777-781.
- Karopadi AN, Mason G, Rettore E, Ronco C (2013) Cost of peritoneal dialysis and haemodialysis across the world. Nephrology Dialysis Transplantation 28(10): 2553-2569.
- Scholes Robertson NJ, Gutman T, Howell M, Craig J, Chalmers R, et al. (2022a) Clinicians’ perspectives on equity of access to dialysis and kidney transplantation for rural people in Australia: A semistructured interview study. BMJ Open 12(2): e052315-e052319.
- Kukuh Ardian, Endang Sutisna Sulaeman, Arief Suryono (2017) Social Economic Equity in the Utilization of Hemodialysis Among Patients with Chronic Renal Failure Under National Health Insurance Plan at Dr. Moewardi Hospital, Surakarta. Journal of Health Policy and Management 2(1): 28-41.
- Richard JB, Aldigier JC, Le Mignot L, Glaudet F, Ben Said M, et al. (2009b) Equity of accessibility to dialysis facilities. Studies in Health Technology and Informatics 150(1): 777-781.
- White P, James V, Ansell D, Lodhi V, Donovan KL (2006a) Equity of access to dialysis facilities in Wales. QJM: An International Journal of Medicine 99(7): 445-452.
- Crews DC, Novick TK (2020) Achieving equity in dialysis care and outcomes: The role of policies. Seminars in Dialysis 33(1): 43-51.
- Li PKT, Chan GCK, Chen J, Chen HC, Cheng YL, et al. (2021a) Tackling Dialysis Burden around the World: A Global Challenge. Kidney Diseases 7(3): 167-175.
- Wauters JP, Uehlinger D (2004) Non-medical factors influencing peritoneal dialysis utilization: The Swiss experience. Nephrology Dialysis Transplantation 19(6): 1363-1367.
- Bennett PN, Jaeschke S, Sinclair PM, Kerr PG, Holt S, et al. (2014) Increasing home dialysis knowledge through a web-based e-learning program. Nephrology (Carlton, Vic.) 19(6): 345-351.
- Shiff B, Pierrato A, Oliver MJ, Jain AK, McCormick B, et al. (2014) Knowledge, attitudes, and practices with regard to PD access: A report from the Peritoneal Dialysis Access Subcommittee of the Ontario Renal Network Committee on Independent Dialysis. Peritoneal Dialysis International: Journal of the International Society for Peritoneal Dialysis 34(7): 791-795.
- Schellartz I, Ohnhaeuser T, Mettang T, Scholten N (2021) The role of personal attitudes of control and responsibility for the uptake of peritoneal dialysis- a national survey among dialysis patients. BMC Nephrology 22(1): 107-109.
- Pressly KB (1995) Psychosocial characteristics of CAPD patients and the occurrence of infectious complications. ANNA Journal 22(6): 563–572; discussion 573-574.
- Batista AF, Caminha MFC, Silva CC, Sales CCS (2016) Knowledge, attitudes, and practice by caregivers of children and adolescents undergoing hemodialysis or peritoneal dialysis. Rev Eletr Enf 18(1): e1164-e1175.
- Bonenkamp AA, Hoekstra T, Hemmelder MH, van Eck van der Sluijs A, Abrahams AC, et al. (2022) Trends in home dialysis use differ among age categories in past two decades: A Dutch registry study. European Journal of Clinical Investigation 52(1): e13656- e13662.
- Choi SJ, Obi Y, Ko GJ, You AS, Eriguchi R, et al. (2020) Comparing Patient Survival of Home Hemodialysis and Peritoneal Dialysis Patients. American Journal of Nephrology 51(3): 192-200.
- Griffith DM, Umeukeje EM (2022) Navigating to Kidney Health Equity. Journal of the American Society of Nephrology 33(7): 1242-1244.
- Hajj JJ, Laudanski K (2017) Home Hemodialysis (HHD) Treatment as Effective yet Underutilized Treatment Modality in the United States. Healthcare (Basel, Switzerland) 5(4): 90-95.
- Hsu CM, Weiner DE, Aweh G, Salenger P, Johnson DS, et al. (2021) Epidemiology and Outcomes of COVID-19 in Home Dialysis Patients Compared with In-Center Dialysis Patients. Journal of the American Society of Nephrology 32(7): 1569-1573.
- Huria T, Palmer S, Beckert L, Williman J, Pitama S (2018) Inequity in dialysis related practices and outcomes in Aotearoa/New Zealand: A Kaupapa Māori analysis. International Journal for Equity in Health, 17(1): 27-35.
- Li PKT, Garcia Garcia G, Lui SF, Andreoli S, Fung WWS, et al. (2020) Kidney health for everyone everywhere: From prevention to detection and equitable access to care. Journal of Nephrology 33(2): 201-210.
- Lockridge R Jr, Weinhandl E, Kraus M, Schreiber M, Spry L, et al. (2020) A Systematic Approach to Promoting Home Hemodialysis during End Stage Kidney Disease. Kidney360 1(9): 993-1001.
- Manns BJ, Garg AX, Sood MM, Ferguson T, Kim SJ, et al. (2022) Multifaceted Intervention to Increase the Use of Home Dialysis: A Cluster Randomized Controlled Trial. Clinical Journal of the American Society of Nephrology 17(4): 535-545.
- Moosa MR, Norris KC (2021) Sustainable social development: Tackling poverty to achieve kidney health equity. Nature Reviews Nephrology 17(1): 3-4.
- Nadeau Fredette AC, Tennankore KK, Perl J, Bargman JM, Johnson DW, et al. (2020) Home Hemodialysis and Peritoneal Dialysis Patient and Technique Survival in Canada. Kidney International Reports 5(11): 1965-1973.
- Noyes J, Roberts G, Williams G, Chess J, Mc Laughlin L (2021) Understanding the low take-up of home-based dialysis through a shared decision-making lens: A qualitative study. BMJ Open 11(11): e053937-e053940.
- Powe NR (2023) A Step Forward for Precision Equity in Kidney Disease. New England Journal of Medicine 388(11): 1043-1044.
- Rizzolo K, Cervantes L, Shen JI (2022) Racial and Ethnic Disparities in Home Dialysis Use in the United States: Barriers and Solutions. Journal of the American Society of Nephrology 33(7): 1258-1261.
- Rydell H, Ivarsson K, Almquist M, Segelmark M, Clyne N (2019) Improved long-term survival with home hemodialysis compared with institutional hemodialysis and peritoneal dialysis: A matched cohort study. BMC Nephrology 20(1): 52-55.
- Schreiber MJ, Chatoth DK, Salenger P (2021) Challenges and Opportunities in Expanding Home Hemodialysis for 2025. Advances in Chronic Kidney Disease 28(2): 129-135.
- Van Biesen W, Jha V, Abu Alfa AK, Andreoli SP, Ashuntantang G, et al. (2020) Considerations on equity in management of end-stage kidney disease in low- and middle-income countries. Kidney International Supplements 10(1): e63-e71.
- Wayne WD (1995) Daniel, Wayne W.: Biostatistics—A Foundations for Analysis in the Health Sciences. Wiley & Sons, New York—Chichester—Brisbane—Toronto—Singapore, 6th ed. 1995, 780 S., £58.—, ISBN 0–471–58852-0 (cloth). Biometrical Journal 37(6): 744-744.
- Wu HHL, Dhaygude AP, Mitra S, Tennankore KK (2023) Home dialysis in older adults: Challenges and solutions. Clinical Kidney Journal 16(3): 422-431.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...