Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Opinion(ISSN: 2690-5760) 
Anomaly of High COVID-19 Cases in a State with Better Health Care Volume 3 - Issue 5
Velayudhan Mohan Kumar*
- Kerala Chapter, National Academy of Medical Sciences, India
Received:September 29, 2021; Published: October 20, 2021
Corresponding author:Velayudhan Mohan Kumar, Kerala Chapter, National Academy of Medical Sciences (India), New Delhi, India
DOI: 10.32474/JCCM.2021.03.000175
Abstract
Thickly populated Kerala was the first Indian state to get affected by COVID-19 on 2nd Feb 2020. The number of cases here rose much faster than in the rest of India. The containment measures adopted by the state, which brought the infection rate to near zero by the first week of May 2020, were internationally acclaimed. When the expatriates started returning to the state, with the lifting of the lockdown in May 2020, there was again a steep increase in the number of cases. This state with only 2.5% of the Indian population, now accounts for 62% of all the Covid cases in the country. While experts are struggling to explain the anomaly by attributing it to the lower IgG positivity rate in serological surveys and delta variant, some put the blame on the laxity of the people and the indifference of political parties. Others think that the state government had failed to manage institutional quarantine, and to ensure good home quarantine. At the same time, the better health care facility in Kerala is evident from the lower mortality rate, as compared to the rest of India. The Kerala government claims that it is in a comfortable position in terms of ICU and ventilator occupancy, as more than half of them are still lying vacant.
Keywords: Kerala Model; COVID-19; Community Spread; Contact Tracing; Quarantine; Containment Measures; Pandemic
Introduction
Kerala was the first Indian state to get affected by COVID-19 on 2 Feb 2020. The ability of the state to deal effectively with COVID-19 was evident from the detailed guidelines issued by the Department of Health and Family Welfare of Kerala on 5th January 2020, i.e., much earlier than the first case detection in India. Most of the initial cases came from the Gulf countries. Of the 500 plus cases reported from Kerala, the number of people who got the disease through local contact was just about 150 only. The main reasons for this achievement were efficient contact tracing, aggressive testing, and effective quarantine of the infected persons. Special care was also taken to isolate and monitor those who had come in contact with the infected persons. Though the cases in Kerala rose up to 500, much faster than in the rest of India, it dropped to near zero by the first week of May 2020. The effective containment measures adopted by the state, came to be acclaimed as the ‘Kerala Model’ of dealing with COVID-19 [1-3]. The nation-wide lockdown was enforced from midnight of 24th March 2020 [4]. Though the lockdown helped to prevent the spread of the disease, it produced untold miseries to blue-collar workers [5]. Large numbers of migrant laborers from north Indian states, who were deprived of their daily wages, were stranded in Kerala, after the sudden nationwide shutdown from the midnight of 24th March 2020. Most of them, who live in unhygienic conditions, were provided quarantined shelter in a healthier environment, and were given access to entertainment like TV and indoor games. Millions of cooked meals were distributed not only to them but also to those, whose daily earnings were affected [6]. Financial help was provided to small traders and other affected people in the unorganized sectors. These social support measures ensured that the lockdown measures of the government were complied with by the distressed section of society.
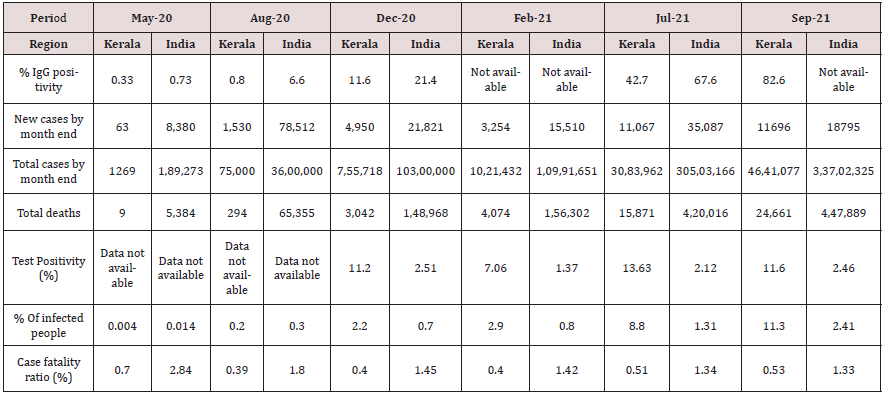
When the lockdown was lifted in May 2020, the Keralites stranded outside the state started returning, and the cases went up very steeply (Table 1 & Figure 1). The state was maintaining a strict surveillance of the returnees and was employing testing procedures to ensure the lowest possible spread of the disease. ‘Break the chain’ campaign and other containment measures were more efficiently implemented in Kerala than in the rest of India. The state government scaled up testing and quarantine facilities, as the number of expatriates steadily increased. Those who showed signs of the disease, at the entry point, were sent to corona care hospital facilities. But those with no signs of the disease were first sent to quarantine facilities for 7 days. At the end of this period, they were tested for COVID-19. If the test was negative, they were allowed to go home and they were instructed to remain isolated in their homes for the next 7 days. Pregnant ladies, senior citizens above 75 years, and children below 10 years were sent home in special cabs and instructed to remain isolated in their own homes for 14 days. Airlines staff and airport personnel, including security staff, were given special training and provided with personal protection equipment. These were some of the pre-emptive, multipronged strategies that any nation could take to deal with global health emergencies such as a pandemic. Though Kerala was successful in controlling the initial spread of the disease, the state did not fare that well later. The initial increase in the COVID-19 cases was due to infected people coming from outside, but they were soon outnumbered by people getting infected through local contact. Kerala became the first state in India where community spread of COVID-19 was officially confirmed.
Figure 1: Number of COVID-19 cases reported from the state of Kerala and the total number of daily cases from the entire India. Cases reported from India do include those from Kerala also. Y axis: number of cases; X axis: period.
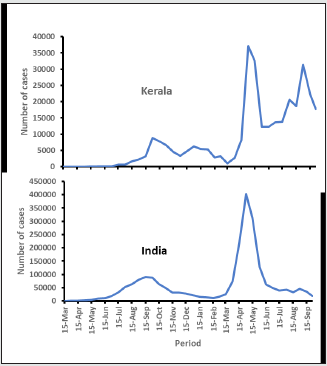
When the cases came down in rest of India, by the tail end of the first wave in February 2021, the number of Covid-19 cases remained high in Kerala. The same pattern was seen during the second wave of the disease which started by February/March 2021. When the Covid cases and test positivity rate (TPR) came down to a low level (2.12) on an all-India average by July 2021, in Kerala it not only remained high in July (13.63), but it also even crossed 20 by the end of August 2021. The estimated population of Kerala (34.8 million), forms only 2.5% of the estimated population of India (1,393 million). But Kerala accounted for nearly one fifth of the daily reported cases in India by Feb 2021, when the first wave nearly came down to a plateau. The state accounted for nearly one third of the daily reported cases by July 2021; it almost reached to 62% of all the cases in India (Table 1 & Figure 1). Moreover, of all the breakthrough infections (infections in fully vaccinated people) reported in the country, close to 50 % of the cases were reported from Kerala [7]. By August 2021 the number of cases went higher, along with the test positivity rate (Table 1). Though the large number of breakthrough infections in the state has raised questions regarding virus mutations that managed to escape the immunity offered by vaccines, genetic studies conducted on breakthrough infections did not support such a possibility [7]. Though questions were raised regarding the possible virus mutations that had managed to escape the immunity offered by the vaccines, genetic studies conducted on breakthrough infections did not support such a possibility [7].
Possible Reasons for High Infection Rate
The upward spiral of fresh Covid cases has put a question mark over the effectiveness of the quarantine measures in the state [8]. While institutional quarantine was the rule in the initial phases of the COVID-19 pandemic, government machinery found it difficult to manage the situation when the number of patients increased. Moreover, with the passage of time, people become increasingly reluctant to move to institutional quarantine. A health department study has found that 35% of the new infections recorded were household ones. According to the State Health Minister Veena George “When a person becomes infected, all the other family members pick up the disease.” The central government too has voiced its concern at the effectiveness of home quarantine, as 80% of the Covid patients are taking treatment at their homes in this state [9]. Though contact tracing was very efficient in the beginning, the administration found it challenging to monitor all the cases when the numbers went up. The presence of the delta variant, though universally present, has added to the misery of the state. According to Kerala Government Medical Officers’ Association, the presence of many asymptomatic people has also complicated effective quarantining [11]. According to them, the over-reliance by the public on the less sensitive rapid antigen tests, has further complicated the containment strategy. Though the health department’s guideline is to conduct an RT-PCR test if a symptomatic person is shown negative in a rapid antigen test, doctors complain that people hesitate to repeat the test. According to Kerala Chief Minister Pinarayi Vijayan “Apart from high population density, Kerala has several risk factors for Covid spread when compared to other places, like constant inflow of people from other states and countries” [10]. Despite the worsening situation, Chief Minister reiterated that Kerala is a model state with regard to Covid management [12]. He pointed out that the case fatality ratio (CFR) is still among the lowest in the country. It achieved a low CFR by overcoming negative factors such as high population density, presence of more senior citizens and widespread presence of lifestyle diseases. He was emphatic in pointing out that no one in Kerala died because of lack of ventilators or short supply of oxygen.
Serological surveys were held in May, August and December 2020, and July 2021 by the Indian Council of Medical Research, to find out the percentage of people with IgG positivity in the population. The seroprevalence in Kerala was much lower than in the rest of India, in all the four surveys (Table 1). It showed that more than one-fifth of the country’s population had been infected by COVID-19 by December 2020, and two-thirds of Indians were exposed to COVID-19 by July 2021. On the other hand, in Kerala only 11.6% people were exposed to COVID-19 by December 2020, and 42.7% by July 2021 [13-15]. The studies on humoral immune response to COVID-19 have shown that IgG elevation, initiated with infection, plays a key role in long-term immune memory [16-18]. Those with high antibody status (in IgG antibody testing), are at a lower risk of being infected by this contagious virus [19]. This immunity, acquired by the general population in the rest of India, may be a reason for the lower number of cases (Table 1 and Figure 1). But the Kerala Government claims that this shows the effectiveness of their containment measures [20]. As per experts in the state, breakthrough infections are the highest among healthcare workers [21]. After vaccination, many countries including the US, UK and Israel had reported a high number of breakthrough infections, especially among healthcare workers, that had put at risk the patients that they were treating. Though vaccinated people have a lower risk of infection compared to those who are unvaccinated, the level of protection from infection by vaccines is lower against the Delta variant. Delta variant is now the predominant strain of SARSCoV- 2 virus in the world. Maximum breakthrough infections were reported with the spread of the Delta variant.
Multiple studies indicate that the Delta variant infection results in a higher viral load compared to infection by the original strain and other variants [22]. So, the delta variant could also be playing a role in the spread of Covid in the state. Though the government has its own limitations, lowering of guard by the public might have also contributed to the situation. It was reported that even those patients under home care in the high-risk category have also not gone for timely treatment. The delay in approaching hospitals in time results in complications and deaths, thereby putting a question mark on the home care system itself. Medical experts feel that the state government went wrong in some aspects of the Covid management [12]. Despite warnings about the risks of huge gatherings, the state government had allowed social and religious festivals to go ahead, drawing people from around the state. The state government and all the political parties organised political rallies, with complete disregard for the COVID-19 mitigation measures. Though all these are lapses on the part of Kerala government, the other states were more guilty on all these accounts. So, to say that the spurt in Covid cases in Kerala is due to these faults may not be fully justified.
Number of Cases May Not Necessarily Reflect Efficiency of Health Care
Covid vaccination that started in India on 16th January 2021, could not have played any major role in the decrease in the number of Covid cases in rest of India. Though the central government had tried to make equitable distribution of vaccine throughout the country, the number of people vaccinated in Kerala was higher. This was due to the better utilisation (zero wastage) of vaccine supplied to the state, and preferential supply of vaccine to the state by the central government to contain the rising infection. All throughout, the mortality rate in Kerala had been lower than the national average. Kerala government claims that the state is in a comfortable position in terms of ICUs and ventilators, as they are now only at 38% and 32% occupancy respectively [11]. According to Padmanabha Shenoy, an immunologist and public health expert, “The percentage of active cases requiring ICU and ventilator has halved over last two months when the percentage of fully vaccinated adult population has increased from 6 to 24 %. This is similar to the trend what we see in the United Kingdom.”
The credit for lower mortality rate should go to the better health care facility in Kerala, rather than to the ‘Kerala Model’ of dealing with COVID-19. If we go by the total number of cases in the state, in comparison to the national average, we may have to conclude that the initial effective containment measures had actually increased the number of people vulnerable to Covid infection, by producing a lower herd immunity. Presence of delta variant and failure of containment measures in home quarantine could have played a role in the high infection rate in Kerala. At the same time, the positive side is that the cases have not gone beyond the capacity of the health facilities of the state to manage. In many other states in India, it went beyond the capacity of the government to provide emergency health care facility to COVID-19 patients [23]. It is possible that the measures taken by the state government would have helped in flattening the curve of COVID-19 infected.
Conflict of Interest and Disclosure Statement
There is no conflict of interest.
References
- Pandi Perumal SR, Gulia KK, Gupta D, Kumar VM (2020) Dealing with a pandemic: the Kerala Model of containment strategy for COVID-19. Pathog Glob Health 114(5): 232-233.
- Gulia KK, Kumar VM (2020) Reverse quarantine in Kerala: managing the 2019 novel coronavirus in a state with a relatively large elderly population. Psychogeriatrics 20(5): 794-795.
- Chathukulam J, Tharamangalam J (2021) The Kerala model in the time of COVID19: Rethinking state, society and democracy. World Dev 137: 105207.
- COVID-19 lockdown in India-Wikipedia.
- (2020) The unspoken impact of lockdown on India’s silent majorities.
- Kerala calling April 2020 - Government of Kerala.
- (2021) Breakthrough COVID infections: Kerala government set for genetic studies in three districts.
- Covid is enemy within family: Veena George on home isolation cases.
- (2021) Health dept shares blame for Covid surge, but points to other factors, Kerala.
- (2021) Better immunity, improved vaccine coverage help Kerala avoid stringent Covid curbs.
- (2021) Covid containment measures: Pinarayi asks critics to suggest alternative model.
- Pinarayi calls for calm amid Covid surge in Kerala, counts on vaccine.
- (2021) ICMR sero survey says two-thirds of Indians exposed to Covid.
- (2021) Technical paper COVID-19, ICMR-Serological Surveillance Report. Department of Health & Family Welfare Government of Kerala p. 1-6.
- (2021) Serosurvey shows exposure to coronavirus lower in Kerala against national average.
- Hou H, Wang T, Zhang B, Luo Y, Mao L, et al (2020) Detection of IgM and IgG antibodies in patients with coronavirus disease 2019. Clinical & Translational Immunology 9(5): 1136-1139.
- Schmidt SB, Grüter L, Boltzmann M, Rollnik JD (2020) Prevalence of serum IgG antibodies against SARS-CoV-2 among clinic staff. PLoS ONE 15(6): 235417.
- Kumar MS, Bhatnagar T, Manickam P, Kumar V S, Rade K, et al (2020) National sero-surveillance to monitor the trend of SARS-CoV-2 infection transmission in India: Protocol for community-based surveillance. Indian J Med Res 151(5): 419-423.
- (2021) COVID-19 What the Third National Sero-Survey Result Does and Doesn’t Tell Us. The Sciences (Health).
- Health Services, Official web portal, Government of Kerala, India.
- (2021) COVID-19: Breakthrough infections in Kerala not alarming, say experts.
- (2021) Study in Vietnam showed that Delta infection results in a higher viral load compared to earlier strains, not that vaccinated people are more infectious than unvaccinated people.
- Editorial (2020) India under COVID-19 lockdown. The Lancet 395(10233): 1315-1319.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...