Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Opinion(ISSN: 2690-5760) 
5 Modern Myths About Acute Pneumonia Volume 3 - Issue 5
Igor Klepikov*
- Pediatric surgeon, USA
Received:September 15, 2021; Published: September 29, 2021
Corresponding author:Igor Klepikov, Pediatric surgeon, USA
DOI: 10.32474/JCCM.2021.03.000172
Abstract
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
The solution of the AP problem directly depends on its concept, which sets the direction of research and development. The system of dominant views on the nature and mechanisms of AP development today does not agree with a number of fundamental foundations of medical science and the facts of real reality. The analysis of the 5 most common misconceptions, which are separate fragments of the teaching about the disease, is presented. Correction of existing ideas about the causes and pathogenesis of AP in accordance with scientific canons and objective facts is the basis for solving the problem and should precede the further research process
Keywords:Acute Pneumonia; Sepsis; Septic Shock; Pathogenesis; Antibiotics; Pathogens; Infusion Therapy; The Doctrine of Disease
Introduction
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
The history of treatment of acute pneumonia (AP) is divided into two fundamentally different periods. Initially, for many centuries, medicine accumulated information about the methods of treating this disease, which was scrupulously obtained empirically. The constructiveness of these searches was very difficult and limited due to a lack of scientific information and insufficient technical support for clinical trials and research. Nevertheless, for a long period of time, there was a certain trend in the set of means of providing assistance to this category of patients. The second period of this history, which began in the middle of the last century after the discovery of antibiotics, completely changed the principles of AP treatment. In the atmosphere of emotional uplift after the first successes of antibacterial therapy, the previous methods of helping these patients were discarded and ceased to be taken into account. In this situation, there was no place for a critical and balanced forecast of the long-term consequences of such “sterilizing” therapy, and the basis of AP treatment for a long time corresponded to the popular term “antibiotics alone”. The short-sightedness of such a strategy became more and more obvious every year, but the desire to restore the former effectiveness of antibacterial therapy prevailed over a reasonable and balanced analysis of the natural biological consequences of this drug intervention.
Over time, the use of antibiotics and their effect on the microflora that accompanies our body has significantly expanded not only as a result of medical prescriptions. For example, many people know about the use of these drugs in such branches of the food industry as animal husbandry, poultry farming and even fishing. In this regard, many countries have adopted laws and regulations that oblige manufacturers to provide information about the use of these medicines in the production of the final product (Figure 1). The widespread and long-term use of antibiotics could not remain without biological consequences, which continue to progress slowly but steadily. However, in this context, we are not talking about such well-known phenomena as an increase in the resistance of microflora and a decrease in the effectiveness of antibiotics. Such consequences of this therapy are well known and are often discussed not only in the specialized literature, but also in the mass media. A potentially more serious and difficult obstacle to solving the problem is the impact of antibiotics on the longterm training of medical personnel and the formation of a new AP ideology. The worldview on this problem, which has developed over the past few decades, declares concepts and ideas that contradict objective facts and the foundations of medical science. It should be borne in mind that the AP concept is the key to solving the problem and the actual guide to this search. In this regard, it is advisable to analyze some provisions of the modern AP doctrine, which are accepted in medical circles as irrefutable, despite the presence of counter arguments.
Myth 1: AP is an Infectious Disease
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
Throughout the centuries-old history of the AP, there was no evidence of the contagiousness of this disease and the danger of its transmission from a sick to a healthy person. Patients with AP were not subjected to isolation and other precautions necessary for infectious processes. There was only a seasonal difference in the frequency of this disease, but no AP epidemics were observed. The distortion of views on the nature of AP occurred gradually and in parallel with a decrease in the effectiveness of antibiotics and an increase in the resistance of microflora. During the initial success of penicillin, acute inflammation of the lung tissue continued to be considered as a non-specific process, which corresponded to the probability of participation in its occurrence of many symbionts around us. However, the further decrease in the effectiveness of antibiotics with persistent attempts to solve the problem of AP with the help of etiotropic therapy grew with each new generation of doctors and naturally accustomed them to the idea of the leading role of infection in this disease. In this regard, it is important to pay attention to the undoubted fact that the etiology and epidemiology of bacterial forms of AP have not undergone fundamental changes in recent decades, and the classification of this disease as infectious was not accompanied by a corresponding change in the epidemiological conditions and regime for such patients. Thus, the classification of bacterial forms of AP as infectious diseases was a reflection of an excessive perception of the role of the etiology of the process. The introduction of this term in the description of the AP does not have a reasoned scientific basis and further narrows the view of the problem, creating additional difficulties in solving it. In this context, it is useful to get acquainted with the materials on viral forms of AR, the pathogens of which require compliance with epidemiological conditions. The frequency of viral lung lesions has been steadily increasing in recent years [1-3], which seems quite a natural consequence of prolonged exposure to antibacterial drugs.
If earlier banal bacterial inflammations were often the result of respiratory viral diseases, during which the number of such patients increased, in recent years the viral expansion has grown so much that the development of AP periodically has the character of epidemics [4] and even pandemic. According to such characteristics as the transmission of the pathogen and the need to introduce anti-epidemic measures, the term “infectious” is suitable only for the viral etiology of AP. However, even with this variant of the disease, you should pay attention to one very significant indicator. For example, according to the statistics of the current SARSCOV- 2 pandemic, the causative agent of which experts assess as particularly virulent, the overwhelming number of infected people (up to 80%) overcome this contact without resorting to medical care, and in a fifth of them the infection is generally asymptomatic [5-8]. These data confirm the old rule that says that people do not get infected with pneumonia but get sick. Infection of the body means the transmission of a pathogen that does not belong to representatives of our microbiota, but this fact is not equivalent to the transmission of the disease, since additional conditions are necessary for the development of AP. In this regard, the emphasis on the word “infection” has a double meaning. Such terminology is relatively important only for the epidemiology of viral diseases. At the same time, the general meaning of this term for all variants of AP plays a negative role, unnecessarily focusing on the etiology of the process.
Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
The longer antibiotics were used, the more clearly the microflora around us demonstrated its biological ability to adapt. The decrease in the effectiveness of antimicrobial drugs was explained not only by the growing resistance of pathogens, but also by their special virulence. At the same time, the properties of individual microbes studied “in vitro” served as the basis for analogies and explanations of the clinical features of the disease. Such ideas about the clinical significance of the type and properties of the pathogen made it necessary to urgently determine the pathogen of AP for targeted antibacterial therapy. Attention to this characteristic of the disease only confirms its non-specific etiology and the possibility of participation in this process of a wide list of microorganisms.
For a long period, practical medicine has been trying to establish a microbiological diagnosis of AP, in the overwhelming number of observations, not being able to study the material from the field of inflammation. Therefore, the main tests used were studies of the microflora of the nose and oropharynx, as well as trace reactions in the form of determining the antigens of individual strains in the blood and even in the urine. However, the presence of certain microbes in the human body does not yet serve as proof of their participation in the inflammatory process. As a result, leading experts recognized that attempts to determine the pathogen of AP do not affect the results of treatment, and the appointment of antibiotics should be empirical [9]. The actual meaning of this conclusion means that the pathogen of the process remains unknown in the overwhelming number of patients with AP and there is no evidence explaining the severity of the disease by the special virulence of the bacterial factor. Recent events have presented one more counterargument against the fact that the properties of the pathogen determine the severity of the course of the disease. Each one of us, being a unique biological object, also reacts in a unique and individual way to the same stimuli. The emergence of a pandemic as a result of the spread of one pathogen shows us an infinite range of options for such contact, in which the infectious agent actually has constant characteristics in each observation, but the individual result of its penetration into the body is significantly different.
Myth 3: Sepsis and septic shock are common complications of AP
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
The idea of the leading role of the pathogen in the severity of clinical manifestations of AP, naturally, contributes to the expectation of septic complications in such patients. Complications, such as sepsis and septic shock, have been considered for many years as the main causes of the severe course of the disease. The modern interpretation of the manifestation of AР is based on the systemic inflammatory response syndrome (SIRS), which has certain clinical and laboratory criteria [10-12]. In previous years, this feature of the body’s response to the inflammatory process was considered in the form of three main forms of manifestation of its reactivity: hypoergic, normoergic and hyperergic. That is, this gradation divided one of the characteristics of inflammatory diseases into possible individual variants of the course of the process from cases with relatively slow development to the most aggressive and lightning-fast forms.
In the modern interpretation, the concept of SIRS in AP combines the reactions of the body that do not have the character of extreme manifestations of the disease. At the same time, lowsymptomatic forms of AP have actually ceased to be allocated to a separate group, and its more severe manifestations, depending on clinical and laboratory changes, are currently regarded as sepsis or septic shock [10]. The diagnosis of these complications in accordance with modern recommendations does not require such a cardinal confirmation of their septic nature as the detection of the pathogen in the blood. It is surprising that the etiology of the disease, which usually occupies the main place in the descriptions of AP, loses its significance just in those situations when it becomes a more important criterion. In the literature on this issue, only isolated reports of bacterial forms of AP can be found, in which the frequency of detection of bacteria in the blood of patients with this disease is only from 2-9% to 12%, including not only cases of sepsis and septic shock, but also bacteremia [9,13,14]. Analyzing septic complications of various diseases, some authors draw attention to the fact that bacteriological blood testing in patients with AP usually does not give results [15,16]. Even in patients with septic shock with pneumonia, the frequency of positive blood cultures is only from 13.2% to 18%, and the comparative mortality rates from this complication with positive and negative tests do not have significant differences [17,18].
The main reason for the negative results of bacteriological blood tests in most patients with AP with sepsis and septic shock is explained by the effect of preliminary antibacterial therapy [15,19,20]. The paradoxical nature of this conclusion is obvious, since it turns out that, on the one hand, antibiotics effectively destroy bacteria, but, on the other hand, they are not able to prevent the development of septic complications. This strange and illogical explanation could arise only on the basis of the complete dependence of the ideas about the clinical manifestations of AP on the leading role of its pathogen. The idea of the causes of the severity of clinical manifestations of AP changes dramatically if we recall the fundamental features of inflammation of the lung tissue. In modern publications, the mechanism accompanying inflammation in the lungs is not given due attention, so cases of sepsis and septic shock in patients with AP are not analyzed as a separate group. The general material of the analysis of these complications usually includes information about various diseases, in which patients with lung tissue inflammation account for up to 40-50% [12]. The combination of diseases with diametrically opposite pathogenetic mechanisms is a very serious misconception about such analytical work.
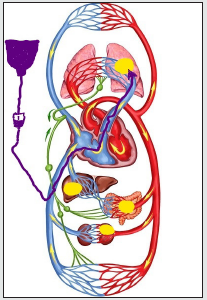
In connection with the above, it is necessary, first of all, to recall the main mechanisms of inflammatory transformation of tissues in the affected area. The basis of the pathological restructuring of tissue structures is the indispensable development of a consistent reaction of blood vessels with impaired blood flow and increased permeability of their walls, as well as the mandatory accompaniment of these changes with five classic signs of inflammation (heat, pain, redness, swelling and loss of function). The last sign, a violation of the function of the affected organ, plays a leading role in the clinical manifestations of the disease. But, the main feature of the topic under discussion is the fact that AP is the only representative of inflammatory processes occurring in the small circle of blood circulation, unlike all other nosologies localized in the large circle. The inverse proportion of the functional state between the two circulatory circles with their inseparable anatomical and functional connection and interdependence clearly indicates fundamental differences in the pathological mechanisms accompanying the different localization of the primary focus of inflammation. In this regard, the interpretation of the pathogenesis of AP by analogy with other forms of acute inflammation can in no way have the same scenario. The assessment of the identified deviations of the vital functions of the body should also have a different understanding. The appearance of a focus of acute inflammation in the vessels of the small circle is a disaster for the body and the cause that disrupts the balance between the two halves of the circulatory system. The localization of this zone not only creates a physical obstacle to the main blood flow, which is ejected by the right half of the heart (see explanation 1 to the Figure 2), but also is a source of reflex spasm of the pulmonary vessels [21-24]. The capacity of the small circle decreases, and the pressure in its vessels increases. To correct this situation and avoid asynchronous operation of the cardiovascular system, the body changes the parameters of the large circle of blood circulation, reducing the pressure in it and increasing its volume for a sudden “excess” of circulating blood (the Schwiegk’s reflex).
a) The comparative value of foci of acute inflammation (yellow fields) for different departments and volumes of blood flow, depending on the possible localization.
b) The initial route of intravenous administration of solutions (dark purple arrow).
Autonomous regulation of blood circulation is one of the fundamental materials of medical science, and the described mechanism allows the body to avoid hemodynamic shifts in the AP that become incompatible with life. The more aggressive the inflammatory process develops, the less time the body has to adapt and the more serious deviations are observed as a result. In such situations, the hyperergic reaction of the body to a sudden problem has long been considered as sepsis, although no evidence of the generalization of the infectious onset is given. In the most critical situations, secondary changes in peripheral hemodynamics fully correspond to the definition of shock, the origin of which is associated with damage to the pulmonary vessels and the body’s attempt to restore the proportions between the two circles of blood circulation and the synchronicity of their work. This variant of shock is not caused by a septic factor, and it would be more correct to designate it as a pulmonal shock [25].
Incorrect interpretation of the cause of severe AP increases the concentration of attention on the etiology of the process in many cases without specifying a specific pathogen and leaves aside the true causes and mechanisms of critical situations. These misconceptions are further deepened as a result of existing approaches to assessing the condition of patients. The lesion of the vessels of the small circle is an indispensable result of inflammation of the lung tissue and the source of the resulting catastrophe of blood circulation. However, the idea of the septic nature of generalized circulatory disorders involves diagnosis, interpretation and their subsequent correction based on the parameters of peripheral blood flow. These principles, which are quite acceptable in other localities of the primary focus of inflammation, have the opposite meaning in patients with AP, when shifts in peripheral blood circulation are secondary and more reflect the adaptation process, rather than the initial manifestations of the disease.
The inverse relationship of blood pressure indicators in the small and large circles of blood circulation has been known for a long time, but the significance and role of this phenomenon in the pathogenesis of AP is not even mentioned today. Modern recommendations and protocols for the diagnosis and treatment of AP complications are focused on the leading role of the etiological factor in the development and course of the disease. The main cause and the beginning of the inflammatory process is considered to be its pathogen, and the further dynamics and development of complications are explained by its aggressive properties. The existing principles allow us to freely use such diagnoses as” sepsis” and” septic shock “ on the basis of clinical and laboratory, and not bacteriological АP. The ideology of this misconception continues to spread today to COVID-19 pneumonia. The severity of this form of the disease is explained by the development of viral sepsis and viral shock, which are considered as causes only by analogy with the existing concept of АР, without any attempts at objective diagnosis [26,27]. And H.C. Prescott and T.D. Girard [28], analyzing the features of COVID-19 pneumonia among hospitalized patients, frankly note that viral sepsis in them resembles (!) bacterial and develops in 20% of these observations, but they do not confirm these figures with any microbiological arguments. Thus, the clinical manifestation of AP is due to the body’s reaction to the onset of the inflammatory process, which is currently called SIRS. It should only be noted that SIRS has a huge range of individual manifestations from barely noticeable signs to the most aggressive forms of the disease. It is the latter variants of the clinical picture that are classified as septic complications, although these manifestations do not depend on the characteristics of the pathogen and are due to the rapid development of the general mechanisms of the process with insufficient compensation for violations.
Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
Currently, almost all urgently hospitalized patients immediately get access to the venous bed and begin to receive an infusion of solutions. This priority of this procedure is due not only to the need to have the most effective way of administering medications, but also to compensate for the loss of fluid, which in acute diseases has many reasons for this. Further recommendations for the correction of water-electrolyte and volume losses and the choice of the infusion rate are determined by the general criteria for their diagnosis in accordance with the parameters of the large circle of blood circulation. Considering AP, first of all, as a result of infection and not focusing on the localization of the process, modern medicine does not make exceptions in this therapeutic direction for patients with inflammation of the lung tissue.
For many years, fever and tachypnea were considered the main causes of fluid deficiency in patients with AP [29]. But the role of these factors in the occurrence of inconspicuous losses is hardly worthy of comparison with the consequences of homeostasis disorders that accompany such diseases as, for example, enterocolitis or peritonitis, when the body really loses large volumes of fluid and these losses are quite noticeable and can be assessed both quantitatively and qualitatively. Despite such a significant difference between demonstrative and hidden losses, the recommendations regarding the volume and speed of infusions in severe patients with septic complications of inflammatory diseases are the same, regardless of the location of the primary focus [11,12,26,30]. From my point of view, the lack of liquid in the AP, which occurs in a short time as a result of evaporation, is clearly exaggerated. Practical medicine does not have precise methods for determining the losses expected as a result of perspiration. At the same time, one of the main reasons for the appointment of infusion therapy for AP is the tendency of these patients to hypotension. It is this sign that serves as a guideline for intravenous infusions, since the next recommendation after the start of bolus infusions, which often do not achieve the expected effect, is the introduction of vasopressors to these patients. The mechanism of hypotension in the large circle of blood circulation in AP, as a result of damage to the pulmonary vessels, was presented above. This sign of the disease is especially manifested in the aggressive development of the process. In this situation, it is not difficult to imagine the role played by infusions that increase venous return and additional blood flow to the focus of inflammation (Figure 2). However, the effect of infusion therapy on the development of AP is a much more complex process than its visual version shown in the figure.
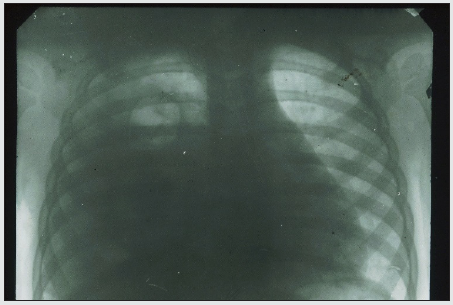
The need to clarify the role of infusion therapy in the dynamics of the development of lung inflammation arose in our work many years ago, when the most aggressive bacterial forms of AP began to be purposefully hospitalized in the our department during the initial period of the disease. The concentration of a large number of such patients was accompanied by the rapid development of pleural complications and high mortality in them. A typical example of such a development of events is our following observation. A 2-year-old girl was taken to the clinic with abdominal pain and shortness of breath 12 hours after their appearance. According to her medical history, the child was healthy, but in the last few days she had a mild respiratory syndrome with a runny nose and a cough without fever. Upon admission to the clinic, the patient was diagnosed with AP (Figure 3). Intensive treatment was immediately started, including intravenous administration of two antibiotics and intravenous fluids up to 30 ml / kg / hour for 2 hours, followed by a decrease in the infusion rate to 10 ml/ kg/ hour. Despite the treatment, the child’s condition did not improve, and a control radiograph was diagnosed with pyopneumothorax 36 hours after hospitalization (Figure 4). The pus obtained from the pleural cavity during drainage was subjected to bacteriological and microscopic examination, but no microflora was found in it. The presented observation cannot be an absolute proof of the negative effect of infusion therapy on the dynamics of the inflammatory process in the lung. The results of the observed transformation in the area of inflammation only allow us to assume such a dependence and draw appropriate conclusions on an empirical basis. Therefore, in order to find additional arguments in favor of such an assumption, which cannot be obtained in clinical conditions, animal experiments were conducted. The volume of the description of experimental studies does not allow us to present them in the framework of a journal article. However, if it is necessary to obtain this information, it can be found in available sources [31,32]. Only the section of the study that is directly relevant to the issue under discussion is given here.
Figure 3: X-ray photograph of 2 y.o. girl 12 hours after the first signs of AP with abdominal pain syndrome were discovered. There is homogeneous shading in a middle-right pulmonary field.
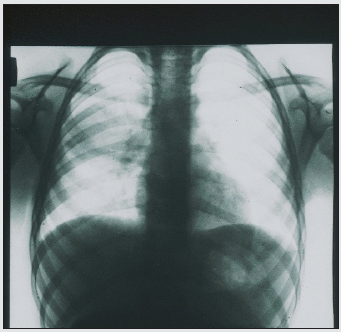
Figure 4: X-ray of the same patient (see Fig. 3), 36 hours after the start of inpatient treatment. There is an intense uniform darkening of almost the entire right hemithorax with a displacement of the mediastinum to the left, as well as a cavity with a fluid level in the upper pulmonary field.
First of all, a model of the bronchogenic form of AP was created. At the same time, in order to reduce the charismatic etiology of the disease and to assess the significance of other factors, cultures of microbes that are usually not considered as pathogens of AP were used. The choice was made in favor of Escherichia coli and Staphylococcus epidermidis. When a statistically reliable stable production of the AP model was obtained, in the final series of experiments, intravenous infusions of solutions were administered to rabbits during the occurrence of inflammation in the lungs. The volume of infusions was 30 ml / kg / hour and was performed once a day for 3 days. In addition, in 6 cases, the addition of a methylene blue dye to the infusion solution was used. This technique was borrowed from the experiments of V. Mеnkin, who discovered the permeability factor [33]. The results obtained after euthanasia of animals on the fourth day of the experiment showed the following. Reproduction of the AP model without subsequent intravenous infusions was accompanied by the development of local inflammation of the lung tissue with a slight pleural reaction in some cases. Intravenous infusions in all cases were accompanied by the development of parapneumonic pleurisy. In two cases, pyopneumothorax was detected, the cause of which was small foci of destruction in the lung tissue. After infusions with the addition of dye, weakly colored lung tissues were found along the periphery of the inflammatory focus (Figure 5).
Figure 5: Macro-preparation of the lung (experiment, series 4b). Massive focus of the inflammation in a pulmonary surface (red arrow), surrounded by the additional sections of infiltration with blue shading (blue arrows). Explanations in the text.
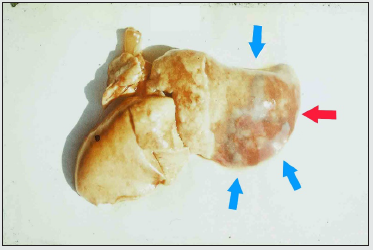
Thus, the results of the experiments allowed us to obtain additional and undoubted confirmation of the negative role of intravenous infusions in AP. The use of the dye demonstrated a visual effect of the spread of inflammatory infiltration in the lung tissue, which is a consequence of increased blood flow to the area with increased vascular permeability. In addition, it should be emphasized that, despite the strict repetition of the experimental conditions in each specific case, the final results represented a number of different variants of pathology. The presented information allows us to analyze the reasons for the continued growth of pleural empyema in patients with AP from a different angle, even in regions with advanced healthcare systems [34,35]. Such an analysis will allow us to evaluate one of the pathogenetic mechanisms of AP and understand why community-acquired pneumonia occurs with parapneumonic effusions in 20-50% of cases, and pleural empyema often turns out to be sterile in microbiological studies [36].
Myth 5. Antibiotics are the Main Treatment for AP
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
In the middle of the last century, a significant event occurred in medicine, the biological role and didactic significance of which are still not fully understood. We are talking about the discovery and the beginning of the use of antibiotics, which changed not only the basic principles of the treatment of inflammatory processes, but also had a specific impact on the formation of professional ideas about them. The first experience of treating many severe inflammatory diseases with antibiotics has brought fantastic results that could not even have been expected before. These drugs have saved millions of lives, and despite the loss of their initial effectiveness, they continue to retain their therapeutic value when properly used.
Аntibiotics are still one of the most popular medicines. Their action, unlike other representatives of the pharmacopoeia, is directed not at the structures and substances of the body, but at its microflora. At the same time, each representative of the microbial world is itself a separate biological object. It is these circumstances that can explain the fact that the same antibiotic can help as a general therapeutic agent for diseases that are completely incomparable in pathogenesis. Today, as in the initial period of the use of antibiotics, their positive effect is considered as the main condition for success in the treatment of AP, but with such a narrowly focused therapy, the elimination of functional and morphological disorders remains completely a problem of the body. The action of antibiotics cannot be used only against suspected pathogens of AP. Their introduction into the body affects those representatives of the microflora who are sensitive to this drug. In this regard, antimicrobial treatment can create biological side effects. It is impossible to avoid such results of antibacterial therapy, and their stability and prevalence with the further use of antibiotics retain the prerequisites for strengthening these negative consequences. Today, the discussion of antibiotic-resistant strains of pathogens, a whole galaxy of which has appeared in recent decades and continues to grow, has become commonplace. The detection of such strains in healthy people during testing, if necessary, is no longer a non-standard situation. Dysbacteriosis has become a habitual probability of long-term treatment with antimicrobial drugs.
Finally, during the period of widespread use of antibiotics, a change of leaders among the pathogens of AP began to be observed. In the literature, it was not possible to find special studies confirming the effect of this therapy on the dynamics of the etiology of the disease. However, this phenomenon, which was not so obvious in the past, is quite consistent with the prescription of antibiotics. Prolonged suppression of the dominant pathogen of AP leads to a gradual predominance of other microorganisms in the development of this process. This frequency of change of AP pathogens is another indirect proof that the causes of the disease remain the same and do not have a direct dependence on the microflora. To the above, it is necessary to add such an undoubted statistical fact as the steady increase in the incidence of AP of viral etiology, which has been observed in recent decades [1-3]. The shift in the etiology of lung inflammation towards viral forms is another result of the long-term suppression of the microbial segment of our microbiological support. This postulate cannot be accepted as an absolute argument, but further events should show the trends existing in this section. In the meantime, it can be stated that over the past couple of decades, the coronavirus epidemics have turned into a pandemic, and vaccinations do not give a full guarantee and require their repetition due to the appearance of new and new strains. This picture suggests that humanity is entering the era of viral diseases. If the future begins to confirm these gloomy assumptions, then their results should be considered a side effect of our achievements and efforts. The peculiarities of antibiotics that have only an antibacterial effect and do not affect the vital links of pathogenesis do not allow us to consider them as the leading and even more so the only means of treating AP. But for many years, the bulk of these patients were treated on the principle of “only antibiotics”, isn’t it? If we add to this the above-mentioned side effects of this method, then the further use of drugs of this group should be carried out under much stricter control than it is being carried out now. However, in this situation, an insurmountable obstacle arises, due to many years of didactic traditions. Medical training based on the expected benefits of antimicrobial principles today orients therapeutic efforts in the same direction, despite changing conditions, logic and meaning.
At the moment, the recommendations of specialists and specific approaches to treatment demonstrate a subconscious desire to preserve old stereotypes, despite the change in the etiology of AP and the inadequacy of antibacterial therapy to new conditions. The appearance of a large number of patients with COVID-19 pneumonia led to the fact that antibiotics that do not have an antiviral effect automatically lost their purpose. However, this logical assessment does not correspond to the real state of affairs. Currently, bacterial co-infection, the methods of determining which cause great doubts about their reliability, is detected only in a few percent of cases among patients with COVID-19 pneumonia. At the same time, antibiotic treatment is carried out in more than 70-80% of these patients [37-42]. The role of old stereotypes of medical care in the new conditions becomes even more convincing when they are not subjected to the necessary revision at all, and patients with coronavirus infection are automatically included in the treatment regimen for community-acquired pneumonia [43,44]. However, it is no secret that such treatment regimens are based on antibiotics. While continuing to consider antibiotics as the main therapeutic agent for AP, no one focuses on those facts that contradict such an assessment of their role. After a long period of antibiotic use, they are still prescribed empirically [9,42,45-47]. The target choice of medicines remains “blind”, depending on the experience of the attending doctors, the capabilities of the local pharmacy and often as a happy coincidence. The dubious accuracy of determining the pathogen has not changed for the better for many years, and in the first hours and days of treatment, the etiology of AP is usually unknown. The same antibiotic is taken as the basis for the treatment of completely different diseases, incomparable from the point of view of the mechanism of development, when the medical duty is performed by distributing one drug between different categories of patients. Long-term efforts to improve treatment outcomes with long-term courses have been replaced in recent years by recommendations for antibacterial therapy for 3-5 days [9,48-50].
The emergence of the pandemic has led to an increase in the number of cases of the disease with a coronavirus etiology. New conditions with a sharp increase in the risk of spreading the pathogen only strengthened the etiotropic problem-solving strategy and preserved its tactical principles. In bacterial forms of AP, efforts were made to more quickly determine the pathogen and choose the most effective antimicrobial agent. Having failed in this longterm search, practical medicine is currently trying to narrow down the range of research. Now, with COVID-19 pneumonia with one variant of the pathogen, but the lack of effective etiotropic agents, the search for a suitable antibiotic against it begins. The monopoly of old ideas in conducting modern research on the problem of AP remains a very big obstacle to achieving success. For example, the antibiotic “azithromycin” has been used in medicine for more than 30 years not only for bacterial forms of AP, but also for middle ear inflammation, streptococcal pharyngitis and even diarrhea [51]. Currently, this drug, which does not have proven antiviral activity, is being tested in clinical conditions against coronavirus [52]. Only the lack of other ideas for solving the problem and confusion can explain the fact that, having received no evidence of the beneficial effect of this antibiotic against the coronavirus, the authors suggest continuing this study. Thus, antibiotics, even in the initial period of their maximum effectiveness, were not a specific means of helping with AP and cannot correspond to the concept of the main, and even more so the only method of treating this disease. To date, the long-term use of antibiotics has reached a period when the preservation of their effectiveness can no longer be supported only by the development of new-generation drugs. The side effects of antibacterial therapy continue to change the microbiological environment around us. One of the consequences of this type of treatment is the growing tendency to change the pathogens of AP with the growth of viral forms of the disease and a decrease in the role of antimicrobials themselves. The biological consequences of the widespread use of antibiotics have already passed the point of no return. They should be perceived as a persistent phenomenon that can only develop further. However, in order to understand the depth and significance of these consequences for the future, as well as to level the observed trends, it is necessary to realize the didactic negative impact of this type of therapy on the formation of a professional worldview. This is the only consequence of antibiotics that can be corrected, and its correction completely depends on each of us.
Conclusion
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
Optimal ways of providing care to patients with AP for several decades remain one of the most discussed, but almost unchanged areas of therapeutic medicine. In the last couple of years, interest in this section has increased dramatically as a result of the development of the pandemic and the appearance of a large number of patients with COVID-19 pneumonia. The loss of the usual treatment regimens for this form of AP turned into a wide search for new etiotropic drugs, although the effectiveness of the previous treatment of this group of patients caused deep concern among experts. The research conducted today continues to be based on the previous concept of the disease, which frankly contradicts a number of fundamental provisions of medicine. The continuation of this path in solving the AP problem excludes the guarantee of success and progress in the future. A radical revision of the AP doctrine is the first and inevitable step of further research.
References
- Abstract
- Introduction
- Myth 1: AP is an Infectious Disease
- Myth 2: The Severity of the AP Course is Due to the Properties of its Pathogen
- Myth 3: Sepsis and septic shock are common complications of AP
- Myth 4: AP is Accompanied by a Significant Loss of Fluid
- Myth 5. Antibiotics are the Main Treatment for AP
- Conclusion
- References
- Rudan I, Boschi Pinto C, Biloglav Z, Mulholland K, Campbell H (2008) Epidemiology and etiology of childhood pneumonia. Bull World Health Organ 86(5): 408-416.
- (2004) WHO Revised global burden of disease 2002 estimates.
- Ruuskanen O, Lahti E, Jennings LC, Murdoch DR (2011) Viral pneumonia. Lancet 377 (9773): 1264-75.
- https://en.wikipedia.org/wiki/Severe_acute_respiratory_syndrome
- Ing AJ, Cocks C, Green JP (2020) COVID-19: in the footsteps of Ernest Shackleton. Thorax 75(8): 693-694.
- Z Wu, J M McGoogan (2020) Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China. Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 323(13): 1239-1242.
- Merad M, Martin JC (2020) Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol 20: 355-362.
- Ra SH, Lim JS, Kim G, Min Jae Kim, Jiwon Jung, et al (2021) Upper respiratory viral load in asymptomatic individuals and mildly symptomatic patients with SARS-CoV-2 infection. Thorax 76(1): 61-63.
- J P Metlay, G W Waterer, A C Long, Antonio Anzueto, Jan Brozek, et al (2019) Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. American Journal of Respiratory and Critical Care Medicine 200(7): e45-e67.
- Singer M, Deutschman CS, Christopher Warren S, M Shankar Hari, Djillali A, et al (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8): 801-810.
- Rhodes A, Evans LE, Waleed Alhazzani, Mitchell M Levy, Massimo Antonelli, et al (2017) Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Medicine 43(3): 304-377.
- A Ceccato, A Torres (2018) Sepsis and community-acquired pneumonia. Ann Res Hosp 2: 7-15.
- Sanjay Sethi (2020) Community-Acquired Pneumonia. Merck Manual for the Professional.
- GW Waterer, MW Quasney, RM Cantor, RG Wunderink (2001) Septic shock and respiratory failure in community-acquired pneumonia have different TNF polymorphism associations. AJRCCM 163(7): 1599-1604.
- Lin GL, McGinley JP, Drysdale SB, A J Pollard (2018) Epidemiology and immune pathogenesis of viral sepsis. Front Immunol 9: 2147-2153.
- Weiss SL, Peters MJ, Alhazzani W, Michael S D Agus, Heidi R Flori, et al.(2020) Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med 46(Suppl 1): 10-67.
- Garcia Vidal C, Ardanuy C, Tubau F, D Viasus, J Dorca, et al (2010) Pneumococcal pneumonia presenting with septic shock: host- and pathogen-related factors and outcomes. Thorax 65(1): 77-81.
- Hadil A AlOtair, Mohammed A Hussein, Mohamed A Elhoseny, Abdulaziz H Alzeer, Muhammad F Khan, et al (2015) Severe pneumonia requiring ICU admission: Revisited. Journal of Taibah University Medical Sciences 10(3): 293-299.
- Liapikou A, Ferrer M, Polverino E, Valentina Balasso, Mariano Esperatti, et al (2009) Severe Community-Acquired Pneumonia: Validation of the Infectious Diseases Society of America/American Thoracic Society Guidelines to Predict an Intensive Care Unit Admission. Clin Infect Dis 48(4): 377-385.
- Restrepo MI, Mortensen EM, Rello J, Jennifer Brody, Antonio Anzueto (2010) Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest 137(3): 552-557.
- Schwiegk H (1935) Der Lungenentlastungsreflex. Pflügers Arch. ges. Physiol 236: 206-219.
- Klepikov I (2017) The Meaning of Pulmonary Reflexes in the Pathogenesis of Acute Pneumonia. Intern Med 7(1): 232-234.
- Klepikov I (2018) Acute Pneumonia is More Cardiovascular than Respiratory Disaster. J Emerg Med Care 1(1): 105-107.
- Thillai M, Patvardhan C, Swietlik EM, Tom McLellan, Jan De Backer, et al (2021) Functional respiratory imaging identifies redistribution of pulmonary blood flow in patients with COVID-19. Thorax 76(2): 182-184.
- Klepikov I (2018) Shock in Acute Pneumonia and its Mechanism. EC Emergency Medicine and Critical Care 2(2): 52-53.
- Alhazzani W, Morten Hylander Moller, Yaseen M Arabi, Mark Loeb, Michelle Ng Gong, et al (2020) Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Medicine 46: 854-887.
- L J Schlapbach, N Kissoon, A Alhawsawi, Maha H Aljuaid, Ron Daniels, et al (2020) World Sepsis Day: a global agenda to target a leading cause of morbidity and mortality. AJP Lung Cellular and Molecular Physiology 319(3): L518-L522.
- Prescott HC, Girard TD (2020) Recovery From Severe COVID-19: Leveraging the Lessons of Survival From Sepsis. JAMA 324(8): 739-740.
- D A Berlin, R M Gulick, F J Martinez (2020) Severe Covid-19. N Engl J Med 383(25): 2451-2460.
- Lim TK, Chew MY (2018) Management of severe community acquired pneumonia in the emergency department. J Emerg Crit Care Med 2(1): 2-12.
- Klepikov I (2020) Acute pneumonia. New doctrine and first treatment results. Lambert Academic, USA.
- Igor Klepikov (2021) How many Pneumonias exist in nature? Generis Publishing, USA.
- Menkin Valy (1940) “Dinamics of inflammation”. Macmillan, USA.
- Arnold D, Hamilton F, Morris T, R Payne, NA Maskell (2019) S12 The changes in incidence and management of pleural empyema in England over the last decade. Thorax 74(Suppl2): A9-A10.
- Bobbio A, Bouam S, Frenkiel J, Kevin Zarca,Ludovic Fournel, et al (2021) Epidemiology and prognostic factors of pleural empyema. Thorax.
- Hassan M, Patel S, Sadaka A S, Bedawi EO, Corcoran J P, et al (2021) Recent Insights into the Management of Pleural Infection. International Journal of General Medicine 14: 3415-3429.
- B Beović, M Doušak, J Ferreira Coimbra, Kristina Nadrah, Francesca Rubulotta, et al (2020) Antibiotic use in patients with COVID-19: a ‘snapshot’ Infectious Diseases International Research Initiative (ID-IRI) survey. Journal of Antimicrobial Chemotherapy 75(11): 3386-3390.
- Kim D , Quinn J , Pinsky B, Nigam H Shah, Ian Brown (2020) Rates of co-infection between SARS-CoV-2 and other respiratory pathogens. JAMA 323(20): 2085-2086.
- Ocampo Torres Moisés (2020) Characterization of Mortality by Covid-19 in a Health System in Central Mexico. EC Pulmonology and Respiratory Medicine 9(12): 20-22.
- Rawson TM, Moore LSP, Zhu N, Nishanthy Ranganathan, Keira Skolimowska, et al (2020) Bacterial and fungal co-infection in individuals with coronavirus: A rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis 71(9): 2459-2468.
- Alejandro David Bendala Estrada, Jorge Calderón Calderón Parra, Eduardo Fernández Carracedo, Antonio Muiño Míguez, Antonio Ramos Martínez, et al (2021) Inadequate Use of Antibiotics in the Covid-19 Era: Effectiveness of Antibiotic Therapy, Research Square p. 1-46.
- Puzniak L, Finelli L, Yu KC, Karri A Baue, Pamela Moise, et al (2021) A multicenter analysis of the clinical microbiology and antimicrobial usage in hospitalized patients in the US with or without COVID-19. BMC Infect Dis 21(1): 227-235.
- C Heneghan, A Pluddemann, K R Mahtani (2020) Differentiating viral from bacterial pneumonia. April 8, 2020. The Centre for Evidence-Based Medicine. Evidence Service to support the COVID-19 response, University of Oxford, USA.
- Lipman M, Chambers RC, Singer M, Jeremy Stuart Brown (2020) SARS-CoV-2 pandemic: clinical picture of COVID-19 and implications for research. Thorax 75(8): 614-616.
- Pulia M, Wolf I, Schwei R, Chen D, Lepak A, et al (2021) Antibiotic prescribing patterns for coronavirus disease 2019 (COVID-19) in two emergency departments with rapid procalcitonin. Infection Control & Hospital Epidemiology 42(3): 359-361.
- Montes Andujar L, Tinoco E, Baez Pravia O, Carlos Martin Saborido, Pablo Blanco Schweizer, et al (2021) Empiric antibiotics for community-acquired pneumonia in adult patients: a systematic review and a network meta-analysis. Thorax 76(10): 1020-1031.
- Alejandro David Bendala Estrada, Jorge Calderón Calderón Parra, Eduardo Fernández Carracedo, Antonio Muiño Míguez,Antonio Ramos Martínez, et al (2021) Inadequate Use of Antibiotics in the Covid-19 Era: Effectiveness of Antibiotic Therapy. Research Square p. 1-46.
- (2014) Revised WHO classification and treatment of childhood pneumonia at health facilities. World Health Organization, Geneva.
- A S Ginsburg, T Mvalo, E Nkwopara, Eric D McCollum,Melda Phiri, et al (2020) Amoxicillin for 3 or 5 Days for Chest-Indrawing Pneumonia in Malawian Children. N Engl J Med 383: 13-23.
- A B Chang, K Grimwood (2020) Antibiotics for Childhood Pneumonia — Do We Really Know How Long to Treat?. N Engl J Med 383: 77-79.
- https://en.wikipedia.org/wiki/Azithromycin
- Gyselinck I, Janssens W, Verhamme P, Robin Vos (2021) Rationale for azithromycin in COVID-19: an overview of existing evidence. BMJ Open Respiratory Research 8(1): e000806-e000810.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...