Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4609
Research Article(ISSN: 2637-4609) 
Outcome of Chemical Tattooing in corneal scars in a Tertiary Eye Care Center of Bangladesh Volume 4 - Issue 4
Sujit Kumar Biswas, Soma Rani Roy* and Mahbubul Alam
- Consultant, Department of Cornea, Chittagong Eye Infirmary, Bangladesh
Received:January 3, 2022; Published:March 08, 2022
*Corresponding author:Dr Sujit Kumar Biswas, MBBS, DCO, FCPS, FICO, MRCSEd Consultant, Department of Cornea, Chittagong Eye Infirmary, Chattogram 4202, Bangladesh
DOI: 10.32474/AOICS.2022.04.000221
Abstract
Purpose: To observe the outcome of chemical corneal tattooing suffering from disfiguring corneal scar by using platinum chloride
and hydrazine hydrate.
Methods: Eighteen patients who had no other measures for visual improvement, unable to use cosmetic contact lenses and
unwilling to do enucleation but wanted cosmesis were included. Overlying epithelium of corneal scar were removed, freshly prepared
2% platinum chloride solution applied for 3 to 4 minutes followed by application of freshly prepared 2% hydrazine hydrate
solution for 30 seconds resulting in jet black color. After washing with Ringer’s lactate solution bandage contact lens were applied
and patched for 24 hours [1].
Results: Age range was 17 to 38 years. Twelve (66.66%) were male and 6 (33.33%) were female. Most of the patients (n=13,
72.22%) presented with more or less vascularized cornea. Partial corneal tattooing was done in 7 (38.88%) patients and remaining
11 (61.11%) had full corneal tattooing. Fourteen (77.77%) patients had no complications and other 4 (22.22%) patients had surface
irregularities. Thirteen (72.22%) patients did not show any fading of pigmentation in 2 years follow up. Three (16.5%) showed
fading of color and underwent re-staining 8 months after primary staining [2].
Conclusion: Tattooing of unpleasant corneal scars can provide a good cosmetic outcome.
Keywords: Corneal tattooing; corneal scar; platinum chloride; hydrazine hydrate
Introduction
Tattooing of corneal scars has been known almost for 2000 years.1,2 During the final decade of the 19th and the first decades of the 20th century it was a commonly applied technique.3,4,5 Now a days this ancient treatment is not frequently done due to the tremendous progress in ocular surface reconstructive surgeries. We are going to present some selected cases of chemical corneal tattooing those have given cosmetically better result [3-7].
Patients and Methods
Total 18 patients, of which 12 were male and 6 were female, undergone corneal tattooing at cornea department of Chittagong Eye Infirmary, Bangladesh, from 5th March 2015 to 15th July 2015. The study was approved by the local institutional review board (IRB) and conducted according to the principles of the 2013 revision of the Declaration of Helsinki. Age range was 17 to 38 years and 12 were male, 6 were female. Patients who had no other measures for visual improvement, corneal condition not supporting for cosmetic contact lens but unwilling for enucleation or evisceration were included in the study. Patients with chemical injuries were excluded. Complete ophthalmic examination done and affected eyes vision were 6/60 to no perception of light. The patients were explained that the procedure is only for cosmetic purpose, not for improving the vision and may need repeat surgery. Informed consent was obtained from all patients and legal guardians. Chemical corneal tattooing performed with 2% platinum chloride and 2% Hydrazine Hydrate. Patients were followed up at the first, seventh postoperative day then after a month, at 3rd month 6 month and yearly [8-11].
Surgical Technique
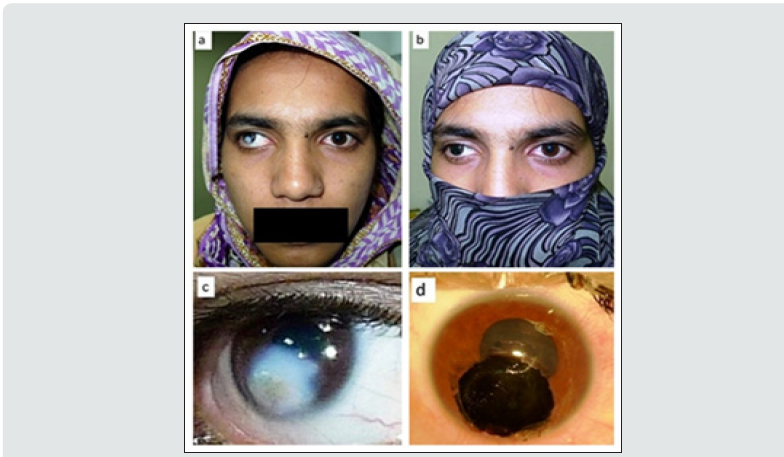
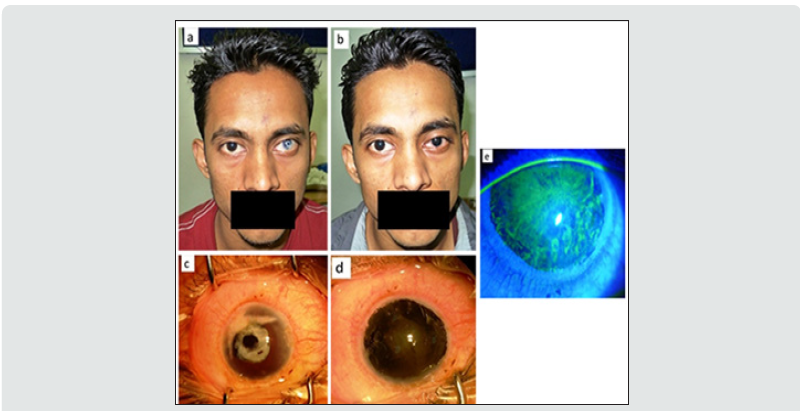
Surgeries were done with aseptic precaution, using operative microscope. Peribulbar anesthesia with mixture of 2% lidocaine and 0.5% bupivacaine with hyaluronidase 50 units was used. The leukoma (corneal dense scar) was marked by trephine and absolute ethyl alcohol was applied over the leukoma for 1 minute. The epithelium over the leukoma scraped with the crescent knife. Freshly prepared solution of 2% platinum chloride was applied with the applicator over the denuded surface for 2 to 3 minutes. Freshly prepared 2% hydrazine hydrate solution was dropped on the surface of the leukoma for about one minute, the leukoma was seen to turn black (Figure 1). Finally, the eye was washed with Ringer’s lactate solution, atropine eye drops 1% and antibiotic eye drop were instilled, and bandage contact lens was applied before bandaging the eye for 24 hours. Postoperative patients were treated with atropine eye drop 1% three times daily for a week, moxifloxacin 0.5% eye drops six times daily for 2 weeks, and dexamethasone eye drops 0.1% six times daily for 2 weeks then tapered over a month. Bandage contact lenses were removed after one week. Three patients associated with calcification were difficult to remove and superficial keratectomy was done with crescent knife before application of platinum chloride and hydrazine hydrate [12).
Results
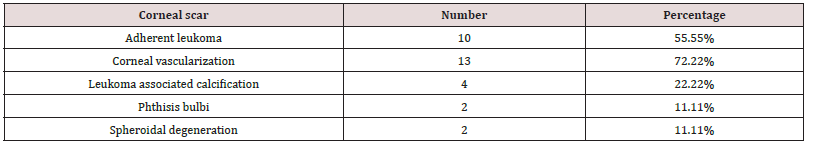
The age range was 17 to 38 and most (n=8, 44.4%) presented between 20-29 years. Male: female was 2:1. Thirteen (72.22%) patients had mild to moderate corneal vascularization. Ten patients (55.55%) had adherent leukoma and 4 (22.22%) had calcification associated with leukoma. Two eyes (11.11%) were phthisical and they were operated to see the effectiveness of tattooing before enucleation. Partial corneal tattooing was done in 7 (38.88%) patients and remaining 11(61.11%) underwent full corneal tattooing. Mild FB sensation, watering, congestion was seen in all patients (Figure 2). FB sensation was more after removal of bandage contact lenses and healing of corneal epithelial defect usually occurred 1 week after surgery. Fourteen (77.77%) patients had no complications and rest 4 (22.22%) patients had surface irregularities. Out of 4 patients, 3 (16.66%) developed epithelial defect after removal of bandage contact lens which was healed with subsequent treatment and 1 (5.55%) developed giant papillae. The color obtained by this method was jet black. Thirteen (72.22%) patients did not show any fading of pigmentation, two (11.11%) had fading of color but still satisfactory and 1 (5.55%) patient experienced nearly total fading with trace pigmentation at periphery as a circle in 6 months follow up. One patient developed corneal melting 3 months after tattooing who had total vascularized scar and underwent evisceration. Only 3(16.5%) patients underwent second surgery 7-8 months after the primary surgery. All patients were followed up for 2 years .
Figure 2: (a, c) Before corneal tattooing, (b, d) After corneal tattooing, e) Negative fluorescein stain after one week of tattooing.
Footnote: some patient had more than one variable.
Footnote: some patient had more than one variable.
Discussion
Tattooing of cosmetically disfiguring corneal scars may be a
valuable therapeutic alternative in a distinct group of patients.
This group comprises patients in whom reconstructive surgical
procedures will not result in functional improvement, difficulty
in wearing a cosmetic contact lens and the reluctant attitude of
the patient for enucleation [2]. Corneal tattooing has been used
not only as a cosmetic treatment for corneal opacities but for
optical reasons as well for centuries. Various methods have been
introduced and modified over the years.6 Now a day two methods
are used predominantly for tattooing the cornea.
a) Chemical method: This involves using metallic salts
which react with each other chemically to produce a brownblack
precipitate that is taken up by the keratocytes and stain the
cornea. The chemicals used are gold chloride, platinum chloride,
silver nitrate which are reduced by hydrazine hydrate and a black
precipitate result. The reacting chemicals are applied over the
stroma directly after peeling the corneal epithelium [2,6,7].
b) Coloring method: This technique involves the direct
introduction or impregnation of colored pigments into the corneal
stroma. To obtain a uniform color, the dyeing agent is injected
through multiple micro-punctures by a needle inserted into the
corneal stroma. Various colored dyes and inks such as Indian
ink, organic colors, animal uveal pigment, Chinese ink, soot have
been used. A surgical difficulty inherent to this technique is the
risk of accidental corneal perforation [2]. The new advances in
technology include using excimer laser to prepare the corneal bed
for tattooing 8; lamellar keratectomy offers excellent results in
terms of a homogeneous application of colour 9 but for many scars,
this is not possible because of irregularity, thinning, staphyloma
or calcification of cornea. Penetrating keratoplasty (PK) has
the risks of infection and graft rejection and its use for cosmetic
purposes is ethically unacceptable in many parts of the world
due to the worldwide shortage of corneal donors. Mechanized
keratopigmentation is another costly option.10 Alternative
methods to improve the aesthetic appearance of disfigured eyes are
cosmetic contact lenses, wearing ocular prosthesis with or without
an enucleation or evisceration 11 With contact lenses, intolerance
frequently develops after prolonged use [12] while wearing an
ocular prosthesis over a scarred cornea often causes inflammation,
infection and corneal erosion. Hence tattooing of corneal opacities
still has a role for the cosmetic improvement of unsightly corneal
scars [13].
Here we used only chemical method with 2% platinum chloride and 2% hydrazine hydrate. The color obtained by this method was jet black which was more comparable to our iris color. We used corneal trephine according to the size of the scar to mark the area precisely to prevent the irregular margin of tattooed area. Absolute alcohol is used to remove the epithelium with the aim of not to damage the Bowman’s membrane. It has been thought that the multiple lacerations of Bowman’s layer might promote recurrent corneal erosions [9]. Four patients associated with calcification difficult to remove the calcific plaque. We used crescent knife to do a superficial keratectomy and tried to make the surface as smooth as possible. Among surface irregularity of 4 patients, 3 showed subsequent epithelial defect and 1 showed giant papillae. Two patients with spheroidal degeneration showed neither subsequent epithelial defect nor fading of color. They are benefited after scrapping the CDK (climatic droplet keratopathy) material (Figure 3). Here patient with vascularized scar did not show any significant fading of color. Two phthisical eyes were done tattooing with the aim to see the effectiveness before enucleation. We will avoid enucleation of those patient if the long-term result will be good. This study showed 2 central and one peripheral fading of color, 6 months after primary tattooing and after re-staining they are doing well. In a series of seven cases by Recep et al. [13] reported that re-staining was performed in one patient. Another study showed, re-staining was performed in five cases out of seven patients [14]. In the current study, we want to show that chemical tattooing is able to improve of ocular cosmetic appearance, easy and safe procedure of tattooing, its efficacy and as an alternative to costly invasive reconstructive surgery for cosmetic improvement within this follow up period. A long term follow up will be needed to confirm further.
Figure 3: (a, c) Before tattooing. Corneal scar is associated with vascularization and calcification. (b, d) After corneal tattooing.

Conclusion
Chemical tattooing of unpleasant corneal scar is an efficient and a simple technique. Its surgical procedure is relatively safe and can avoid invasive reconstructive surgery. Chemical corneal tattooing by this technique gives a satisfactory cosmetic result.
References
- Galen CD (1965) e compositione medicamentorum secundum locos In Kühn CG, ed. Claudii Galeni opera omnia. Hildesheim: Olms 12: 696–803.
- Pitz S, Jahn R, Duis A, Frisch L, Pfeiffer N (2002) Corneal tattooing: an alternative treatment for disfiguring corneal scars. British Journal of Ophthalmolgy 86(4): 397–399.
- Knapp P (1925) Eine neue Methode der Hornhauttätowierung. Klin Monatsbl Augenheilkd 75: 693–700.
- Holth S (1926) Die Technik der Hornhauttätowierung, speziell der mehrfarbigen. Klin Monatsbl Augenheilkd 77: 289–302.
- Gifford SR, Steinberg A (1927) Gold and silver impregnation of cornea for cosmetic purposes. Am J Ophthalmol 10: 240–247.
- Irfan S, Rashid F (2014) To Assess the Efficacy of Chemical Corneal Tattooing for UnsightlyCorneal Scars.Pak J Ophthalmol 30(3).
- Khan, Arif O, Meyer D (2005) Corneal tattooing for the treatment of debilitating glare in a child with traumatic iris loss. Am J of Ophthalmlogy pp. 920-921.
- Anastas CN, McGhee CNJ, Webber SK (1995) Corneal tattooing revisited: excimer laser in the treatment of unsightly leucomata. Aust NZ J Ophthalmol 23: 227–230.
- Panda A, Mohan M, Chawdhary S (1984) Corneal tattooing-experiences with -lamellar pocket procedure. Ind J Ophthalmol 32: 408–11.
- Alio JL, Sirerol B, Walewska-Szafran A, Miranda M (2010) Corneal tattooing (keratopigmentation) with new mineral micronised pigments to restore cosmetic appearance in severely impaired eyes.Br J Ophthalmol 94: 245-249.
- Custer PL, Kennedy RH, Woog JJ (2003) Orbital implants in enucleation surgery. A report by the American Academy of Ophthalmology. Ophthalmol 110: 2054-2061.
- SnejinaV, Hristakieva E (2007) Medical Applications of Tattooing." Clinics in Dermatology 25: 367-374.
- Recep ÖF, Caǧıl N, Hasıripi H (2008) Tattooing for the treatment of corneal opacities Tükiye Klinikleri J Ophthalmol 17: 156–160.
- Kim C, Kim KH, Han YK, Wee WR, Lee JH, et al. (2011) Five-year results of corneal tattooing for cosmetic repair in disfigured eyes Cornea 30: 1135–1139.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...