Lupine Publishers Group
Lupine Publishers
Menu
Research Article(ISSN: 2770-5447)
Prevalence of Prehypertension and its Relationship to Risk Factors for Cardiovascular Diseases in Algeria: Analysis from a Cross-Sectional Survey Volume 3 - Issue 2
A Mammeri1,2, Guermaz R1,2, Brouri M1,2 and Tebaibia A1,2
- 1Department of Internal Medicine, El Biar Hospital, Algiers, Algeria
- 2Faculty of Medicine, University of Algiers1, Algeria
Received:November 12, 2020; Published: November 23, 2020
Corresponding author: A Mammeri, Department of Internal Medicine, El Biar Hospital, Algiers, Algeria
DOI: 10.32474/ACR.2020.03.000160
Abstract
Background: Many studies have documented an increased risk of the development of hypertension (HT) and subsequent cardiovascular diseases (CVD) in persons with prehypertension (PHT). The aim of this study was to assess the prevalence of PHT in Algiers, and to explore the association between PHT and established cardiovascular risk factors (CVRF). To our knowledge, this is the first report on this subject in our country.
Method: A cross-sectional study was conducted in primary care consultation on a sample of 1086, 18-79 years old, unknown hypertensive. They benefited from screening for PHT (defined by JNCVII as a systolic pressure between 120-139mmhg and a diastolic pressure between 80-89 mmhg) and HT (a systolic pressure ≥140 mmhg and / or a diastolic ≥90 mmhg). After completion of a detailed demographic and medical questionnaire (gender, age, history of diabetes mellitus, dyslipidemia and smoking). All participants were subjected to physical examination, anthropometric, blood lipid profile and blood glucose assessments. Odds ratios for associations of PHT with CVRF were obtained using logistic regression.
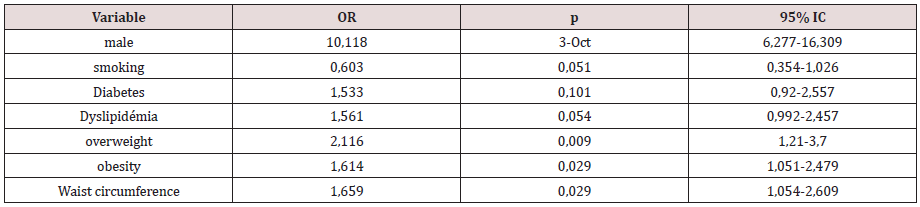
Results: the prevalence of PHT was 36.7%, more common in males (49.5%) than females (31.4%); it was also more important in the ages below 60 years. Prehypertensive patients had a sex ratio of 0.64 and an average age of 42.3 ± 13.9 years. Almost 35.8% of them were overweight, 31.8% were obese, 47.4% had a low physical activity, 17.3% had dyslipidemia, 13% had diabetes mellitus and 19.3% smoked cigarettes. Age and anthropometric values had significantly higher prevalence in the prehypertensive group compared to the normotensive group. Metabolic syndrome involved 25% of patients with PHT according to NCEP/ATPIII 2001 and 36.3% according to the IDF criteria 2009. Concurrent glycoregulation disorders and PHT was prevalent at 29.3% (N=117). Logistic regression analysis identified male (OR = 10,118; 90% CI: 6,277-16,309; p <10-3), overweight (OR = 2,116; IC90 %: 1.21-3.7; p = 0.009), obesity (OR = 1.614; 90% CI: 1.051-2.479; p = 0.029) and waist circumference (OR = 1.659; 90% CI: 1.054-2.609 ; p = 0.029) as the main determinants of PHT in our population.
Conclusion: Our study highlights the need for systematic monitoring of blood pressure in overweight subjects. The benefit of weight loss in the management of PHT seems more important than ever to reduce the cardiovascular risk of these new patients.
Keywords: Prehypertension; Cardiovascular risk
Background
High blood pressure affects almost a third of the world’s population. It is a major public health problem in industrialized countries, but also in emerging countries such as Algeria. Its prevalence in our country varies from 25 to 45% depending on the region, and the national average was 23.6% in 2018 [1]. Since several years, studies have shown that patients with systolic blood pressures at 120-139 mmHg and / or diastolic blood pressures at 80-89 mmHg had an increased risk of developing hypertension (HT) with all that would imply as cardiovascular morbidity and mortality. This was initially demonstrated in the Framingham study by Vasan and al [2] who assessed the 4 year rate of progression from prehypertension (PHT) to HT at 17.6% for normal BP (systolic pressures at 120-129 mmHg and / or diastolic pressures at 80-84 mmHg) and 37.3% for high normal blood pressure (BP) (systolic pressures at 130-139 mmHg and / or diastolic pressures at 85-89 mmHg) in subjects aged less than 65 years. In Europe, Zhang et al [3] shown in the Flemish study that the 4-year rate of progression from PHT to HT, in subjects aged less than 50 years, were 17.9% for normal BP and 24.5% for high normal BP. These figures increased to 26.3% and 54% respectively from the age of 50. The concept of PHT was first introduced in official recommendations in 2003, in the Seventh Report of the Joint National Committee (JNC7) on Prevention, Detection, Evaluation and Treatment of High Blood pressure [4], while in Europe, experts continue to consider PHT in two distinct categories, namely normal BP and high normal BP [5]. By identifying this new blood pressure category, it was pointed out that a pressure within the upper limits of the norm is associated with an increased cardiovascular risk, and that it is already necessary at this stage to implement preventive measures. based on changes in lifestyle. If the increased prevalence of PHT is observed and well documented in many countries, it is still not in Algeria. To our knowledge, this is the first publication which estimates the prevalence of PHT in Algiers and evaluates its relationship with other cardiovascular risk factors (CVRF).
Method Study Population
The present investigation adopted a cross-sectional design protocol. The population studied was recruited at the general practice consultation over one year (2015/2016). We excluded known hypertensive patients, treated or not, those undergoing treatment that could modify their blood pressure figures and pregnant women. The final sample consisted of 1086 subjects who answered a demographic and a detailed medical questionnaire.
Physical Examination
All subjects benefited from height, weight, and waist circumference measurements. Body mass index (BMI) was calculated as weight (in kilograms) divided by height (in meters) squared. A BMI of 20-24.9 kg/m2 was considered normal, a BMI of 25-29.9 kg/m2 as overweight and a BMI ≥ 30 kg/m2 as obese. Android obesity was defined according to the International Diabetes Federation (IDF) [6] (waist circumference ≥ 80 cm for women and ≥ 94 cm for men) and the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATPIII) [7]. (waist circumference ≥ 88 cm for women and ≥ 102 cm for men). Based on European recommendations [5], blood pressure was taken after a rest of at least 5 minutes. Two BP measurements were taken (OMRON M3, Japan), 2min apart and a third one if the first two were quite different. The average of the last two measurements was used in the analysis. In the end, we classified the blood pressure figures according to the JNC 7.
Serum assessments
Prehypertensive and hypertensives’ blood samples were collected in the morning after an overnight fast to assess lipid abnormalities. Those not known to be diabetic benefited from an oral glucose tolerance test (OGTT). Fasting levels between 6.1 and 7.0 mmol/L (1.10 and 1.25 g/L) defined the impaired fasting glycaemia (IFG), and fasting levels at or above 7.0 mmol/L (1.26 g/L) defined diabetes. For a 2 hour GTT with 75 g glucose intake, a glucose level below 7.8 mmol/L (1.40 g/L) was normal, whereas higher levels, between 7.8 mmol/L (1.40 g/L) and 11.1 mmol/L (2g/L) indicated impaired glucose tolerance (IGT), and levels above 200 mg/dL at 2 hours confirm a diagnosis of diabetes [8, 9]. Metabolic syndrome was defined according to the IDF [6] and ATPIII criteria [7] . Coronary heart disease (CHD) risk at 10 years in percent was calculated with the Framingham Risk Score. At 10% the risk was low, at 20% it was moderate and at 30% it was high [10].
Statistical Analysis
Primary data processing involved entering all the questionnaires in a clean file while secondary data processing aimed to produce data analysis files and create the tables required for analysis, according to the aims of our study. Categorical variables were presented as frequencies. Associations between categorical variables were tested by the use of contingency tables and the chisquare test. Logistic regression was used to assess the association of CVRF to blood pressure by estimating the odds ratio with 95% confidence interval (CI). Variables were considered significant at a p-value less than 0,05. These measurements were performed using R software.
Results
Characteristics of the study population
The 1086 participants included in the analyse were distributed in 772 (71%) men and 314 (29%) women. The mean age was 41,6±14,39 years, higher in women than in men (42,2±14,01 ans vs 40,3±15,22 years ; p =0,0017). The prevalence of PHT was 36.7%, higher in men than in women (49.7% vs 31.47%, p<10-3). The prevalence rates of normotensive and unrecognized hypertensive were respectively 15.83% and 47.42% Table 1. The average age of prehypertensive people was 42.3 ± 13.9 years, higher in women than in men (45.3 ± 13.4 years vs 37.6 ± 13.4 years; p = 0.017. Twenty-four percent of the subjects were under 30 years old, 9.3% over 60 years old while 66.7% were between 30 and 59 years old. We noticed that the mean values for age and anthropometric indices were significantly higher (p < 0.001) among the prehypertensive and hypertensive groups compared to those with normal BP. Table 2 shows the characteristics of patients according to BP categories. Among prehypertensive group, we identified 199 subjects with a high normal BP (18.32%). They were older than those with normal BP (N=200) (p = 0.005) and had higher anthropometric indices. For other risk factors, there was no significant difference between the two groups.
Table 1:Prevalence of blood pressure categories according to JNC 7.
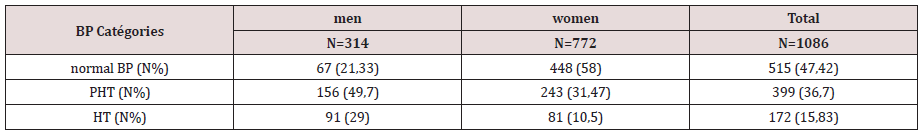
p<10-3
BP :blood pressure, PHT :prehypertension, HT :hypertension
Table 2:Clinical characteristics of patients according to blood pressure levels (JNC7).
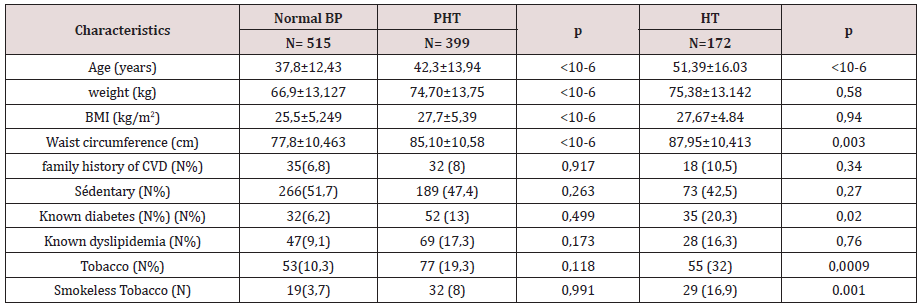
BP :blood pressure, PHT :prehypertension, HT :hypertension , BMI : Body Masse Index
Analytical Study of The Prevalence of Prehypertension
Univariate analysis showed a significant relationship between PHT and male gender (OR = 2.15; 95% CI,1.63 - 2.84, p <10- 6), also found for overweight (OR = 1.52; 95% CI,1.12 - 2.07; p = 0.005), obesity (OR = 1.88; 95% CI,1 , 36 - 2.59, p <10-3), waist circumference (OR= 1.48; 95% CI,1.15 - 1.92, p = 0.002) and dyslipidemia (OR = 1.71 ; 95% CI,1.18 - 2.47, p = 0.003). The results of the multivariate logistic regression analysis ( Table 3, 4) reveal that male gender was the most powerful predictor of PHT (OR= 10,118 ; 95% CI, 6,277-16,309, p < 0.001), followed by overweight (OR=2.11; 95% CI,1,21-3,7,p = 0.009), obesity (OR=1,614 ; 95% CI, 1,051-2,479, p= 0,029) and waist circumference (OR = 1,659; 95% CI, 1,054-2,609, p =0.029).
Table 3:Clinical characteristics of patients according to the two categories of PHT according to ESC classification.
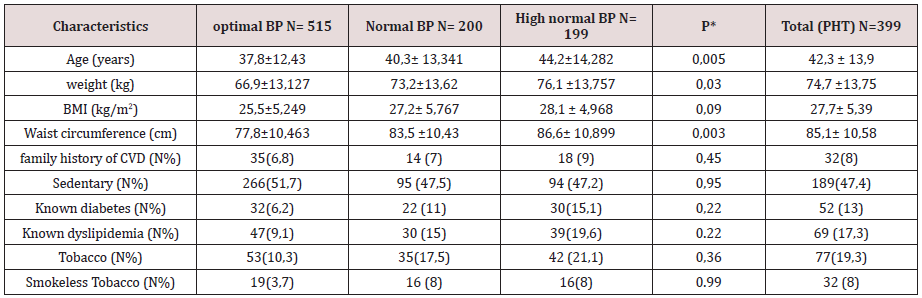
BP :blood pressure, PHT :prehypertension, HT :hypertension , BMI : Body Masse Index
P*: compare results between normal BP and high normal BP
PHT and cardiovascular risk factors
The metabolic assessment was only performed in 280 prehypertensive patients (70,67%). Almost a third (31%) had hypercholesterolemia, 19.6% had high triglyceride level and 42.1% had a low HDL c level. The OGTT, practiced in 230 prehypertensive patients (not known diabetics), identified 13 new diabetics (5.7%) and 52 pre-diabetics (22.6%). Sixteen patients – (16/230) had an impaired glucose tolerance (IGT) (7%) and 36 patients (36/230) had an impaired fasting glycaemia (IFG) (15.7%). So, nearly a third of prehypertensive people had a carbohydrate metabolism abnormality. On average, the Framingham score was estimated at 6.08 ± 5.54 without significant difference regarding to the gender. The coronary risk was low in 83.6% of the cases, intermediate in 11.8% and high in 4.6% . A quarter of prehypertensive patients had metabolic syndrome according to NCEP/ATPIII and this proportion increased to 36.3% when the definition of IDF was applied Table 5.
Table 5:Metabolic data in prehypertensive patients.
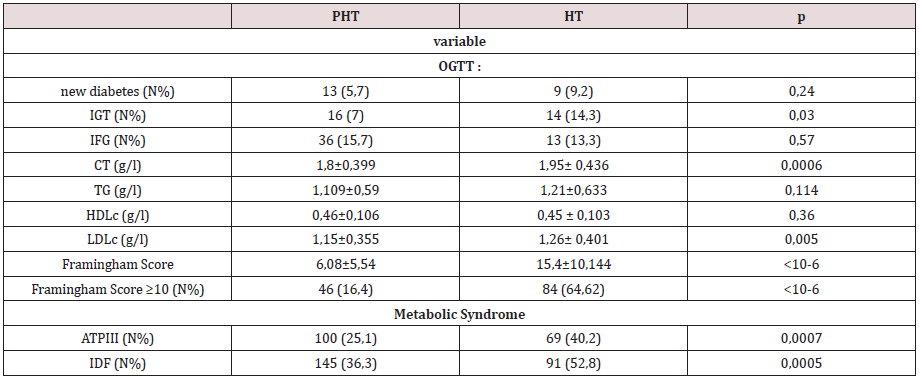
OGTT: Oral glucose tolerance test, IGT :Impaired glucose tolerance, IFG:Impaired fasting glycaemia, CT :cholesterol, TG : triglyceride, HDLc:High Density Lipoprotein cholestrol, LDLc : Low Density Lipoprotein cholesterol
ATPIII :Adult Treatment Panel III, IDF :International Diabetes Federation.
Discussion
The prevalence of PHT in our study (36.74%) does not differ from that estimated in the NHANES III report (31%) [11], and those found by most authors around the world, (30- 40%): Japan 32.7% [12] , Jamaica 30% [13], Greece 39% [14], Iran 33.7% [15], Korea 31.6% [16], Taiwan 34% [17], China 32.3% [18] and Bangladesh 31.9% [19]. These data indicate the weak influence of the geographic distribution of populations on the prevalence of PHT. In most studies, carried out in various countries, the prevalence of PHT is consistently higher in men than in women: Japan [12], Jamaica [13], Iran [15], Korea [16], Taiwan [17], India [20], Brazil [21], USA [22] and Tunisia [23]. The male gender is also pointed out by many authors as determining factor of PHT (15, 23, 24, 25). In our population, PHT is more common in men up to the age of 50 years and the male gender multiplies by 10,118 (6,277- 16,309, p <10-3) the risk of having PHT. BMI was the strongest determining factor in this new blood pressure category as has been suggested by several authors [15,24, 25-28]. The link between overweight and BP has already been established in literature [13, 17,21, 23,29, 30] and the American survey. NAHANES III 1999-2000 had reported that prehypertensive patients were more likely to be overweight than normotensive patients [31].
Conclusion
PHT is common in Algiers. It is strongly determined by other CVRF, including male gender and overweight. PHT does not yet require antihypertensive treatment in most cases but we should call about “hypertension alert” which would require in our country an urgent implementation of preventive measures focused on the management of overweight and obesity. Taking into account a national prevalence of hypertension of 25%, this approach is crucial in reducing blood pressure for more than half of the general population
References
- Enquête nationale sur la mesure du poids des facteurs de risque des Maladies Non Transmissibles selon l’approche STEPwise de l’OMS. Principaux ré
- Vasan RS, Larson MG, Leip EP (2001) Impact of high normal blood pressure on the risk of cardiovascular disease. N Engl J Med 345 : 1291-1297.
- Zhang H, Thijs L, Kuznetsova T (2006) Progression to hypertension in the non-hypertensive participants in the Flemish Study on Environment, Genes and Health Outcomes. J Hypertens 24 (9): 1719-1727.
- Chobanian AV, Bakris GL, Black HR, Suzanne Oparil, Jackson T Wright Jr, et al. (2003) The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 289: 2560-2572.
- Guidelines Committee (2003) European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 21: 1011-1053.
- The IDF consensus worldwide definition of the metabolic syndrome.
- Zimmet P, Alberti G, Shaw J (2005) Nouvelle définition du syndrome mé Diabete voice 50(3).
- Institute for Quality and Efficiency in Health Care (2013) Glucose tolerance test: how does it work exactly ? Informed Health Online. Institute for Quality and Efficiency in Health Care.
- American Diabetes Association (2013) Standards of medical care in diabetes--2013. Diabetes Care. 11-66.
- D’agostino RB, Grundy S, Sullivan LM (2001) Validation of Framingham coronary heart disease prediction score : results of a multiple ethnic groups investigation. JAMA 286(2): 180-187.
- WangY and Wang QJ (2004) The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch intern med 164(19): 2126-2134.
- Ishikawa Y, Ishikawa J, Ishikawa S, Eiji Kajii, Thomas G Pickering (2008) Prevalence and determinants of prehypertension in a Japanese general population: the Jichi Medical School Cohort Study. Hypertens Res. 31(7): 1323-1330.
- Ferguson TS, Younger N OM, Tulloch-Reid M K Elizabeth M Ward, Deanna E Ashley, et al. (2008) Prevalence of prehypertension and its relationship to risk factors for cardiovascular disease in Jamaica: Analysis from a cross- sectional. BMC Cardiovascular Disorders 8: 20.
- Chrysohoou C, Pitsavos C, Panagiotakos DB, (2004) Association between prehypertension status and inflammatory markers related to atherosclerotic disease: the ATTICA Study. American Journal of Hypertension 17(7): 568-573.
- Rahmanian K, Shojaie M (2012) The prevalence of pre-hypertension and its association to established cardiovascular risk factors in south of Iran. BMC Research Notes 5: 386.
- Choi KM, Park HS, Han JH, Kyung Hwan Yoon, Dokyong, et al. (2006) Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. Journal of hypertension 24(8): 1515-1521.
- Tsai PS, Ke TL, Huang CJ, Jen-Chen Tsai, Ping-Ling Chen, et al. (2005) Prevalence and determinants of prehypertension status in the Taiwanese general population. J Hypertens. 23(7): 1355-1360.
- Hu L, Huang X, You C (2017) Prehypertension and hypertension in south china. Plos ONE 12(1) :e0170238.
- Khanam M, Lindeboom W, Razzaque A (2015) Prévalence and determinants of prehypertension and hypertension among the adults in rural Bangladesh: findings from a community-based study BMC Public Health 15: 203.
- Singh RB, Fedacko J, Pella D, Radzhesh Agarwalo, Veerappan V Muthusamy, et al. (2011) Prevalence and risk factors for prehypertension and hypertension in five Indian cities. Acta Cardiol 66(1): 29-37.
- Nary FC, Santos RD, Laurinavicius AG, Raquel Dilguerian de Oliveira Conceição, José Antonio Maluf de Carvalho (2013) Relevance of préhypertension as a diagnostic category in asymptomatic adults. Einstein 11(3): 303-309.
- Hales CM, Caroll MD, Simon PA (2017) hypertension prevalence , awareness, treatment and control among adults aged ≥18years, Los Angeles county ?1999-2006 and 2007-2014.Weekly Rep 66 (32): 846-849.
- Allal elasmi M, Feki M, Zayani Y (2012) Prehypertension among adults in Great Tunis region (Tunisia): A population-based study. Pathologie Biologie 60(3): 174-179.
- Erem C, Hacihasanoglu A, Kocak M (2008) Prevalence of préhypertension and hypertension and associated risk factors among Turkish adults: Trabzon Hypertension Study Journal of Public Health 31(1): 47-58.
- Hariharan S, Chen D, Merritt-Charles L, R Reeves, S Singh, et al. (2006) Prevalence of Préhypertension in Adult Outpatients in Trinidad. West Indian Med J 55(5): 362.
- Sun Z, Zheng L, Wei Y, Dayi Hu, Yingxian Sun, et al. (2007) Prevalence and Risk Factors of the Rural Adult People Prehypertension Status in Liaoning Province of China. Circ J 71(4): 550-553.
- Koura MR, Al-Dabal BK, Rasheed P (2012) Prehypertension among young adult females in Dammam, Saudi Arabia. Eastern Mediterranean Health Journal EMHJ 18(7): 728-734.
- Al asmary S, al shebri A, Fayssal M Farahat, Moataz M Abdel-Fattah, Muraya M, et al. (2008) Community based screening of prehypertension among military active duty personnel. Saoudi Med J 29(12) : 1779-1784.
- Gupta R, Deedwania PC, Achari V Tulika G Mahanta, Arthur J Asirvatham, et al. (2013) Normotension, Prehypertension, and Hypertension in Urban Middle-Class Subjects in India: Prevalence, Awareness, Treatment, and Control. American Journal of Hypertension 26(1): 83-94.
- Hadaegh F, Hasheminia M, Abdi H, Davood Khalili, Mohammadreza Bozorgmanesh, et al. (2015) Prehypertension Tsunami: A Decade Follow-Up of an Iranian Adult Population. PLoS One10(10): e0139412.
- Greenland KJ, Croft JB, Mensah GA (2004) Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999–2000. Archives of Internal Medicine 164(19): 2113-2118.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...