Lupine Publishers Group
Lupine Publishers
Menu
Research Article(ISSN: 2770-5447) 
Myocardial bridge in Resting state does not Induce Myocardial Ischemia Confirmed by Fractional flow Reserve Volume 3 - Issue 5
Fu Qiang1, Zeng Youfa1, Miao Zhilin1, Guan Ruming1, Zhao Linlin1, Su Hao1, Lv He1, Guo Xinjin2 and Hou Aijie1
- 1Department of Cardiology, The People’s Hospital of China Medical University/The People’s Hospital of Liao Ning Province, Shen Yang, Liao Ning, China
- 2Department of Research and Development, Hong Kong Biotechnology and Development Institute, Hong Kong SAR, China
Received:June 3, 2020; Published:June 24, 2021
Corresponding author: Guo Xinjin, Department of Research and Development, Hong Kong Biotechnology and Development Institute, Hong Kong SAR, China
DOI: 10.32474/ACR.2021.03.000171
Abstract
Objective: To investigate whether myocardial bridge (MB) in resting state leads to myocardial ischemia by measuring coronary fractional flow reserve (FFR) and analyze the influence of the most severe stenosis degree(MSSD) and the length of mural coronary artery (MCA) on the decline degree of FFR.
Materials and methods: 39 patients with MB in left anterior descending coronary artery confirmed by coronary computed tomography angioplasty were recruited. Hyperemic proximal FFR (FFRp) and distal FFR(FFRd) of MCA were measured by pressuretemperature sensor guidewire, and then the decline degree of FFR(FFRp-FFRd, FFRp-d) were calculated. QCA software was used to determine MSSD and the length of MCA (MCAL).By comparing FFRp with FFRd, the effect of MB on FFR was analyzed. FFR=0.8(i.e. FFRp-d =0.2 (1-0.8)) was taken as the threshold value of myocardial ischemia to explore the correlation between MB and myocardial ischemia; In addition, we further observed the influence of MCAL and MSSD on FFRp-d.
Results: FFRd is significantly lower than FFRp (P < 0.01).However, FFRp-d was significantly lower than 0.20 (P < 0.01).Another aspect deserves due attention is that there was no correlation between FFRp-d and MCAL(P > 0.05) and MSSD (P > 0.05). Conclusion: Although MB causes a significant decrease in FFR, no ischemia is induced. The degree of FFR decline is independent of both MCAL and MSSD;
Keywords:Myocardial bridge; Mural coronary artery; Fractional flow reserve
Introduction
Coronary arteries can travel segmentally between bundles of myocardial fibers and disappear on the surface of the heart. This section of heart muscle is called myocardial bridge (MB), and the arteries that travel within the heart muscle are called mural coronary arteries(MCA) or bridging vessels[1].MB is a congenital disease and the vast majority of patients may have no symptoms. However, case reports and literature have described that MB is closely related to chest pain after activity, dyspnea after exercise, chest tightness, palpitations, etc [2-5] . Recent studies have found that proximal vessels of MB are associated with atherosclerosis [6-8],Vascular endothelial dysfunction [9-12] and increased myocardial ischemia [13-14] obviously. At present, there are few studies on the correlation between MB and myocardial ischemia. Whether the coronary artery stenosis caused by MB will lead to myocardial ischemia is still inconclusive, and further discussion is needed. In the last 20 years, fractional flow Reserve (FFR) has been widely accepted as a functional evaluation index of coronary artery disease [15]. FFR-guided treatment strategies have been shown to be safe, economical and improve patient outcomes[16]. As an index of invasive functional evaluation, FFR technique is of great significance in determining whether the anatomic stenosis of coronary artery causes physiological ischemia and reasonably guiding the interventional treatment of coronary heart disease[17].
To date, FFR has been used primarily to evaluate fixed critical stenosis (stenosis diameter of 50% ~ 70%)[18], however, the assessment of MB are all empirical small sample reports [19]. Currently, there is a lack of evidence-based medical research support for FFR’s guidance on the evaluation and treatment of MB, and further research is needed. Based on this, this study first time assessed the effect of MB on FFR in resting state, to determine whether MB would induce myocardial ischemia. Quantifying Coronary Angiography (QCA) software was used to determine the length of MCA(MCAL) and the most severe stenosis degree (MSSD) in systolic period and the influence of MSSD and MCAL on the decline degree of FFR was analyzed .
Material and Methods
Study patients
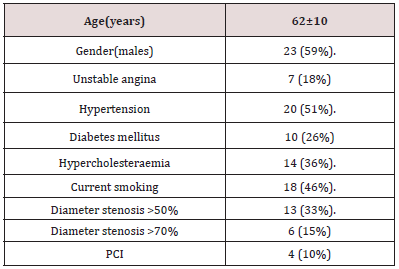
In this study, 39 patients with coronary computed tomography angioplasty (CCTA) confirmed the presence of myocardial bridge in the left anterior descending coronary artery(LAD, Figure 1A). Coronary angiography showed typical milking effect (Figure 1 B and C) on the left anterior descending coronary artery, followed by FFR examination and QCA measurement. All patients signed written informed consent. The research programme complies with the ethical guidelines of the 1975 Helsinki Declaration and has been approved by the local Ethics Committee.
The definition of MB
MB in CCTA cross section shows LAD segments surrounded by myocardium, or transient MCA stenosis was found in at least two positions on coronary angiography, while diastolic vessels returned to normal completely or partially, which is known as the “milking effect”.
QCA measurement
Coronary angiography was performed using standard techniques. Angiographic views were obtained following the administration of intracoronary nitrate (100 or 200 mg).QCA was automatically determined by using the special software Coronary Quantification Package Siemens Medical System, and MCAL and MSSD was measured at the end of contraction (Figure 1D), which were independently confirmed and averaged by two professional technicians.
Figure 1: A. MB confirmed by CCTA; Coronary angiography showed significant “milking effects” during diastole (B) and systolic (C) in patients with a myocardial bridge in the middle portion of the anterior descending left coronary artery (white arrow);D. MCAL and MSSD were measured by QCA software; E:FFRd measurement ; F: FFRP measurement; G:FFRP= 0.99. H:FFRd= 0.88.
FFR Measurement and Threshold Value
All coronary physiologic measurements were performed after diagnostic angiography. A guide catheter (6F) without side holes was used to engage the coronary artery, and a pressuretemperature sensor guidewire (PTGW, Abbott Vascular, St. Paul, Minnesota) was used to measure physiologic indices. After zeroing and equalizing the pressure sensor to the aortic pressure, the pressure sensor was positioned at the distal segment(the distance from distal edge of the MCA is at least 20mm, Figure 1E) of the target vessel. After distal FFR(FFRd) measurement, slowly retracting the guide wire and placing the pressure sensor proximal to MCA for proximal FFR(FFRp) measurement. Intracoronary nitrate (100 or 200 mg) was administered before each physiologic measurement. Hyperemia was induced by intravenous infusion of adenosine (140 mg/kg/min) through a peripheral vein. Hyperemic FFRp (,Figure1F and G) and FFRd (Figure1 H ) were measured during sustained hyperemia after the pressure curve reached a nadir point. The hyperemic period was recognized by a decreased Pd/Pa pattern (Hyperemic proximal aortic pressure (Pa) and distal arterial pressure(Pd)). After measurements were complete, the guidewire was pulled back to the guide catheter, and the presence of a pressure drift was checked. With a drift larger than 3mmHg, re-equalizations and repeated measurements were recommended.
FFR is simply defined as the ratio of the mean distal arterial pressure (Pd) and the mean proximal aortic pressure (Pa) under the state of maximum myocardial congestion, namely FFR=Pd/Pa[20]. The theoretical normal value of FFR is “1”.More than 90% of FFR greater than > 0.80 lesions will not induce myocardial ischemia[21]. In this study, “FFR=0.80”[in other words, FFRp-d=0.2 (1-0.8)] was used as the threshold value of myocardial ischemia[22-24].That is to say, if FFRp-d< 0.2, no myocardial ischemia occurs.
Statistical Analysis
SPSS24.0 software was used for statistical analysis. MCAL, MSSD, FFRp, FFRd, As well as FFRp-d are measurement data, normally distributed data are represented by `X±S, and non-normally distributed data are represented by median (minimum-maximum). The comparison and correlation between FFRp and FFRd were performed by rank sum test and spearman correlation analysis. Pearson correlation analysis and partial correlation analysis were applied to analyze the correlation between FFRp-d and MACL and MSSD. Results were considered statistically significant at p<0.05.
Results
Characteristics of patients
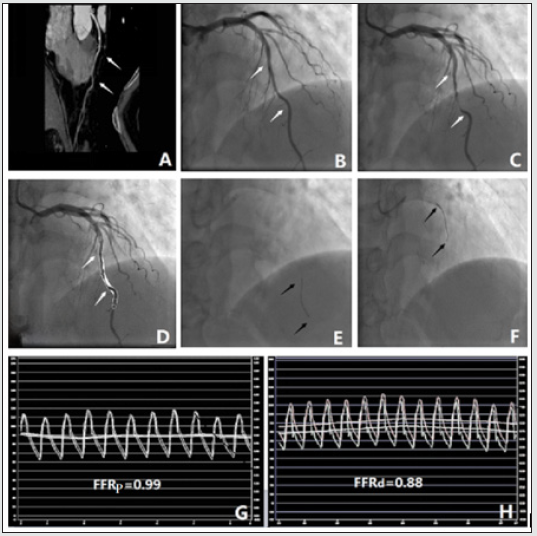
In this study, 39 patients with MB confirmed by CCT and coronary angiography were enrolled. Table 1 shows the clinical characteristics and risk factors of the patients. The mean age was 62±10 years, 23 patients (59%) were male, all patients (7 (18%) were unstable angina pectoris) presented with chest pain, 20 patients (51%) had hypertension, 10 patients (26%) had diabetes, 14 patients (36%) had dyslipidemia, and 18 patients (46%) had smoking history. Of the 39 patients, 13 (33%) had proximal partial stenosis of >50%, and 6 (15%, 4 of whom underwent PCI) had proximal partial stenosis of >70%.
Myocardial bridge causes FFR to decrease but no myocardial ischemia
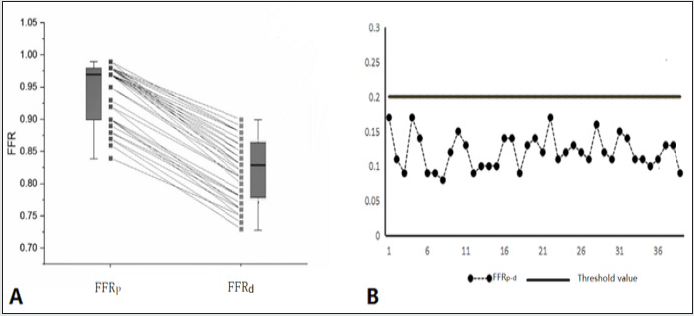
The rank-sum test results indicated FFRd(0.8236±0.0024) Significantly lower than FFRp(0.97,0.84-0.99)(P < 0.01) (Figure 2A and Figure 3A).Spearman correlation (Table 2) analysis results showed that FFRd and FFRp are significantly positively correlated (R=0.827,P < 0.01). In this study, FFRp-d=0.20 was used as the threshold value to judge myocardial ischemia. when FFRp-d < 0.20, the myocardial bridge itself would not cause myocardial ischemia. Data analysis showed that FFRp-d (0.1206±0.0006) was significantly lower than 0.2 (P < 0.001, Figure 2B).Therefore, we hypothesized that the presence of myocardial bridge, leading to a significant decrease in FFR, would not induce myocardial ischemia.
Table 2: Spearman correlation analysis: FFRp and FFRd is significantly positive correlation, P < 0.01.
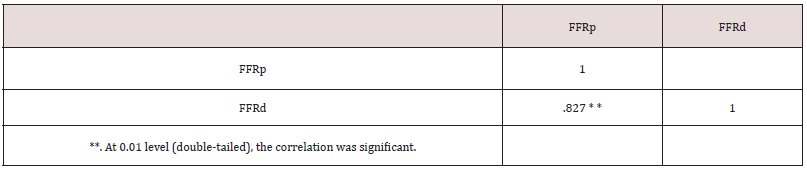
Figure 2: A: multi-group line graph and box diagram: FFRd Significantly lower than FFRp;B: Line graph: FFRp-d Significantly lower than FFR=0.2 (1-0.8).
FFRp-d has no correlation with MCAL and MSSD
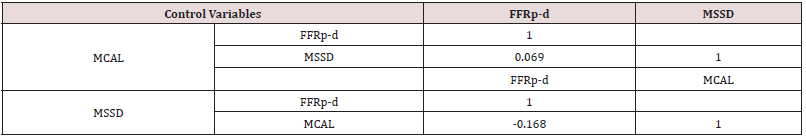
Pearson correlation analysis showed that FFRp-d had no correlation with MCAL (table 3, P > 0.05, figure 3C) and MSSD (table 3, P > 0.05, figure 3D).Partial correlation analysis results: When MSSD was the control variable, FFRp-d had no correlation with MCAL (table 4, P > 0.05);when MCAL was the control variable, FFRp-d had no correlation with MSSD (table 4, P > 0.05).
MSSD and MCAL significant positive correlation
Pearson correlation analysis results were MSSD and MCAL significant positive correlation (Table 3, P < 0.01,Figure 3B).
Figure 3: Scatter plot: A:FFRp and FFRd: significantly positive correlation; B: MCAL and MSSD: significantly positive correlation; C: MCAL and FFRp-d : No correlation; D: MSSD and FFRp-d:no correlation.
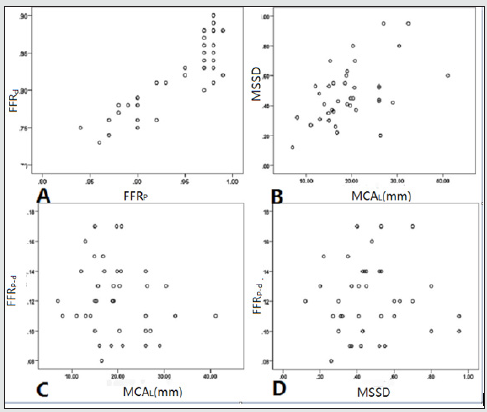
Table 3: Pearson correlation analysis: No correlation between FFRp-d and MSSD and MCAL(P > 0.05). Significantly positive correlation between MCAL and MSSD, P < 0.01.
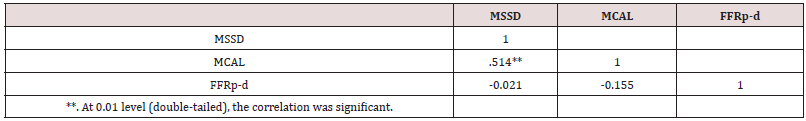
Table 4: Partial correlation:when the control variable is MCAL,There is no correlation between FFRp-d and MSSD;when the control variable is MSSD,There is no correlation between FFRp-d and MCAL.
Discussion
In this study, FFR was the first time used to investigate whether MB can induce myocardial ischemia in resting state and explore the correlation between FFR decline caused by MB and MSSD and MCAL. The research results are discussed as follows:
MB will cause FFR to drop significantly.
Research data confirms that the presence of MB will cause FFR to drop significantly. MB leads to a decrease in coronary blood flow, which is speculated to be caused by the following reasons: 1.MB compresses the coronary artery which occurs during systolic and mid-to-late diastolic periods, leading to a decrease in coronary artery blood flow; 2.Mechanical stress changes caused by narrowing of blood vessels in MB systolic phase can lead to local vasospasm[9]. Possible mechanisms include: increased calciumion concentration in the arterial wall [10]And increased reactivity of vasoconstrictor [11] and so on;3. Hemodynamic and structural changes in the proximal portion of MCA; 4. The depth-type MB is more likely to compress and distort blood vessels, which can last until the diastolic period; In addition, the concentrations of vasoactive agents (endothelial nitric oxide synthase, endothelin-1, and angiotensin-converting enzyme) were lower in the MAC and higher in the proximal and distal portions of MB [8],which may also contribute to the decrease in coronary artery blood flow.
MB itself does not induce myocardial ischemia
Traditionally, MB is considered as a congenital benign developmental anomaly, which was once considered to have no hemodynamic significance. However, studies have shown that MB is clinically correlated with myocardial ischemic events [25]. However, there are few studies on the correlation between MB and myocardial ischemia. In this study, the data showd that the existence of MB leads to a significant decrease of FFR. Based on this, We further analyzed the effect of FFR decline, which caused by myocardial bridge, on myocardial blood supply. In this Research, datas results confirmed that FFRp-d significantly less than 0.2.The presence of MB does not lead to myocardial ischemia, although it leads to a significant decrease in FFR. The speculated reasons are as follows:
1. The stenosis caused by MB occurs in the systolic and midto- late diastolic periods, while the coronary artery blood supply is mainly in the diastolic period, which has limited influence on the coronary blood flow;
2. The degree of stenosis in different parts of MCA caused by myocardial bridge is different, so MSSD can not represent the stenosis degree of the whole MCA;
3. The degree of MCA stenosis caused by MB compression are changed throughout the cardiac cycle, so the duration of MCA stenosis is very short and the duration of MSSD and MCAL is even shorter;
4. The coronary artery structure change caused by MB compression is a complex process, and the actual decrease degree of lumen area does not match MSSD .
In other words, the reduction in the area of the coronary lumen is not as serious as it appears.
FFR decline due to MB is not enough to induce myocardial ischemia, which may explain why the vast majority of MB cases do not have ischaemic symptoms. However, when combined with coronary artery stenosis or other factors that lead to FFR decline, MB may cause further decrease in coronary blood flow, leading to myocardial ischemia and a series of clinical symptoms (Four patients in this study had concurrent coronary artery stenosis and received stent intervention).
FFR decline is independent of MCAL and MSSD
MB causes FFR to drop significantly and FFRd is significantly positively correlated with FFRp. In other words, the higher the FFRp is, The higher the FFRd is. Therefore, we speculated that this may indicate that the decline of FRR has little correlation with the morphological structure of MCA itself. Based on the above inference, we further discussed the correlation between FFRp-d and MCAL and MSSD. Data analysis shows there is no correlation between FFRp-d and MCAL and MSSD.MB-induced FFR decline is independent of MCAL and MSSD. The reasons are as above we discussed why MB itself does not induce myocardial ischemia. MB leads to a significant decrease in FFR, but FFRp-d has no correlation with MCA’s own morphological structure (MCAL and MSSD).
The longer the MCAL is,the more severe MSSD is
In addition, MSSD positively correlated with MCAL. The longer the MCAL is, the more severe the MSSD is. This conclusion is likely consistent with the MB typing (superficial type and depth type) proposed by Ferreira[26].The deeper the MCA walks in the cardiac muscle fibers, the longer the MCA is and the heavier the extrusion is. Depth MB is more likely to compress and distort blood vessels.
Conclusion
The presence of MB can lead to a significant decrease in FFR, but no myocardial ischemia. MB-induced FFR decline is not affected by MCAL and MSSD. However, the presence of MB may cause further decrease of FFR, when combined with coronary artery stenosis or other factors that lead to FFR decline, thereby inducing myocardial ischemia and causing a series of clinical symptoms. So we can get a conclusion that no treatment is necessary for MB itself.
References
- Lee MS, Chen CH (2015) Bridging: an up-to-date review J 27(11): 521-528
- Sunnassee A,Shaohua Z,Liang R (2011) Unexpected death of a young woman: is myocardial bridging significant? A Case Report and Review of Literature [J]. Forensic Sci Med Pathol 5: 42-46.
- Lin S, Tremmel JA, Yamada R (2013) A novel stress echocardiography pattern for myocardial bridge with invasive structural and hemodynamic correlation. J Am Heart Assoc 2(2) : E000097.
- Lee BK, Lim HS, Fearon WF, et al. (2015) Uplift evaluation of patients with Angina in the absence of a patient [J]. Circulation 131: 1054-1060.
- Sharma J, Hellen brand W, Kleinman C (2011) Symptomatic Myo-Cardial Bridges in Children: A Case Report with Review of Literature. Cardiol Young 21: 490-494
- Rozenberg VD, Nepomnyashchikh LM (2004) Pathomorphology and path-ogenic role of myocardial Bridges in sudden cardiac death. J Bull Exp Biol Med 138 (1) : 87-92.
- Hostiuc S, Curca GC, Dermangiu D (2011) Shape changes associated with hemodynamically significant extensions of the heart in sudden cardiac death. J Thorac Cardiovasc Surg 59(7): 393-398.
- Ge J. Jeremias A, Rupp A, et al (1999) New Signs characteristic of Myo-Cardial Fit by Intracoronary ultrasound and Doppler . Eur Heart J 20(23) : 1707-1716.
- Masuda T, Ishikawa Y, Akasaka Y (2001) The effect of myocardial bridging of The coronary artery on vasoactive agents and atheroscle - rosis localization [J] J Pathol 193(3): 408-414.
- Aparci M, Yalcin M, Isilak Z (2016) Proximal proximal MAO was able to proximal proximal MAO and its proximal proximal MAO was able to affect the vascular dynamics of coronary artery [J]. Cardiol 202:782-783.
- Cerit L, Duygu H (2017) Acute bridging and sudden death [J]. Int J Cardiol 229: 11.
- Hostiuc S, Curca GC, Dermangiu D (2011) Shape changes associated with hemodynamically significant extensions of the heart in sudden cardiac death J Thorac Cardiovasc Surg 59(7): 393-398.
- Corban MT, Hung OY, Eshtehardi P (2014) Gren's bridgings: Contemporary Understanding of Pathophysiology with implications for diagnostic and therapeutic strategies [J].J Am Coll Cardiol 63(22): 2346-2355.
- Yu M, Zhang Y, Li Y, Yuehua Li 1, Minghua Li, et al. (2017) Assessment of myocardial bridge by cardiac CT: intracoronary transluminal attenuation gradient derived from diastolic phase predicts systolic compression will J. Journal of Korean J Ra – diol 18(4): 655-663.
- Hu P, Tang MY Song, WC, et al. Xin-Yang Hu, Jian-An Wang (2015) The Fractional Flow Reserve Guided Percutaneous Coronary Intervention little Clinical Outcome witll Reduced Cost I in Clinical Practice J. Chin MedJ (Ensl) 128(15) :2000-2005.
- ls NH, van Schaardenburgh P, Manoharan G. et al. Percutaneous nonsignificant stenosis: 5 years follow-up -- upof the DEFER Study. J Jam Coil Cardiol (2007) 49(21): 2105-2111.
- Toth GG, Hamilos M, Pyxaras S, et al. Guy R Heyndrickx , Jozef Bartunek (2014) The Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J 35(40): 2831-2838.
- Windecker S, Kolh P, Alfonso F, Giulio G Stefanini, David Paul Taggart, et al. (2014) ESC/EACTS guidelines on myocardial Revascularization: The task force on revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-thoracic Surgery (EACTS) developed with the Special Contribution of The European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 35(37): 2541-2619.
- Kurisu Satoshi, Iwasaki Toshitaka, Ishibashi Ken, Mitsuba Naoya, Dohi Yoshihiro, et al. (2012) Measurement of fractional flow reserve in a patient with combined myocardial bridging and Fixed stenosis. J Journal of cardiology cases 6(6): e113-e165.
- Pijls NH, De Bruyne B, Peels K, H J Bonnier, J J Bartunek J Koolen, et al. (1996) Measurement of fractional flow Reserve to assess the functional severity of -- vein Stenoscs J Iv Estimation of fractional flow Reserve J. N Ensl J Med 334(26): 1703 -1708.
- Davies JE, Sen S, Dehbi HM, Manesh R Patel , Patrick Serruyset al. (2017) Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N Engl J Med 376(19): 1824-1834.
- Tonino PA, De Bruyne B, Pijls NH (2009) The Fractional flow reserve Venus angiography for behind percutaneous coronary intervention .N Engl J Med 360(3): 213-224.
- De Bruyne B, Pijls NH Kalesan B, Ole Frobert, Nick Curzen, et al. (2012) The Fractional flow reserve - guided PCI versus medical therapy in stable coronary diseases . N Engl J Med 367(11): 991-1001.
- De Bruyne B, Fearon WF, Pijls NH, Nick Curzen, Jane B Johnson, et al. (2014) Fractional flow reserve-directional PCI for stabl ecoronary disease. N Engl J Med 371(13): 1208-1217.
- Verhagen SN, Rutten A, Meijs MF, Ivana Isgum, Maarten J Cramer, et al. (2013) Relationship between myocardial bridges and reduced coronary atherosclerosis in patients with angina pectoris. Int J Car- diol 167(3): 883-888.
- Ferreira AG, Trotter SE, Knig B, et al. (1991) Beckham's Bridges: shape and functional aspects [J] British Heart Journal 66(5): 364-367.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...