Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5945
Research Article(ISSN: 2638-5945) 
Qualitative Survey of Transgender Dual-Energy X-ray Absorptiometry Protocols Volume 5 - Issue 3
Johnathan Dallman1, BS, Quinnlyn Walcott1, BS, Hanna Crow2, DO, Leland Graves2, MD, Courtney Marsh3, MD
- 1 University of Kansas School of Medicine
- 2University of Kansas Department of Endocrinology
- 3University of Kansas Division of Reproductive Endocrinology and Infertility
Received: April 4, 2023 Published: May 04, 2023
Corresponding author: Johnathan Dallman, University of Kansas School of Medicine, Kansas City, Kansas, USA, 2060 W 39th Ave, Kansas City, KS 66103, USA
DOI: 10.32474/OAJOM.2023.05.000213
Abstract
Introduction: The gold standard for determining bone health is by dual energy x-ray absorptiometry (DXA); however, the use of sex-based reference indices has been shown to be confusing when performing the test for individuals who identify as transgender and gender non-conforming (TGNC). In 2019, the International Society of Clinical Densitometry (ISCD) took the first official “positions” regarding how to perform a DXA scan for TGNC patients. However, it is unknown how closely these guidelines have been followed.
Methods: A survey using REDCap® software was created by utilizing and reformatting the 2019 ISCD DXA TGNC position statement into multiple-choice questions. Respondent demographics, state of employment, DXA experience, knowledge of the TGNC community, and how the respondent performs/interprets DXA scans for TGNC patients were collected.
Results: A total of 26 surveys were completed with respondents representing 14 different states, most being from an academic/ university health system. This outcome corresponds with a 0.7% response rate. When comparing the survey responses to the 2019 ISCD official positions for DXA in transgender individuals, 75% of T-scores and 96% of Z-scores would be deemed “incorrect”. 79% of T-scores and 86% of Z-scores were “incorrect” in non-binary individuals.
Conclusions: The ISCD position statement on performing DXA in the TGNC population is the only society who provides guidance on bone health in this population. When clinicians stray from these guidelines, patients may receive incorrect DXA results as well as missed diagnoses of low bone mass. Future prospective studies need to be conducted to evaluate utilization and the long-term effects of the position’s guidance.
Keywords: Bone Health; Transgende; Dual Energy X-Ray Absorptiometry; Survey; Protocol
History
Transgender and gender non-conforming (TGNC) patients face extensive health care disparities [1] especially, when clinical outcomes depend on sex-based guidelines. One example of this disparity can be found in the musculoskeletal care of TGNC patients where determination of bone mineral density via dual energy absorptiometry (DXA) is reliant on a sex-based reference index. Determining an individual’s bone health via DXA scan is possible due to the calculation of T-scores and Z-scores that are dependent upon a reference sex-based population [2] T-scores are a measurement of bone health calculated by one standard deviation from the mean when compared to that of healthy 25 to 35-year-old adults of the patient’s same sex and race. On the other hand, Z-scores reflect the deviation from an age-matched standard that also incorporates an individual’s sex, race, height, and weight. Limited research has been conducted in this field as it relates to the care of TGNC patients to direct clinicians. The research that has been conducted, such as Dobrolińska et al. [3] has demonstrated the importance of properly utilizing the sex-based reference index in this population. They conducted a study in the Netherlands analyzing DXA scans in both transgender females and transgender males utilizing the male and female reference database for each. In doing so, they determined the female T-score and Z-score reference index produced significantly higher scores in the hip than the male T-score and Z-score reference. Furthermore, based on the male reference values in their study, 18% of transwomen had osteoporosis, compared with only 5% when the female reference index was used.
Unfortunately, no large studies have analyzed gender nonbinary individuals. Through analysis of the complexity of this subject, one can quickly understand how clinicians may not be certain what sex-based reference population to compare to for patients that identify TGNC. Fortunately, this issue was addressed in 2019 when the first official positions regarding how to perform a DXA scan for TGNC patients was released by the International Society of Clinical Densitometry (ISCD) [4] Though several years have passed since the publication of these positions, a retrospective analysis performed at the author’s home institution indicated DXA performers and interpreters were incorrectly performing DXA scans in this population based on the 2019 position by the ISCD [5]. Due to the unknown long-term effects of gender affirming hormone therapies and gonadal surgeries on bone health, the authors deemed it imperative to determine how clinicians across the United States are performing DXA scans for this population. Therefore, the purpose of this study was to uncover the nationwide knowledge and/or misconceptions revolving around DXA scans and bone health in the TGNC community.
Methods
This descriptive study was conducted using a cross-sectional design with individual survey administration. IRB approval was obtained from the authors home institution before a unique survey instrument created for this project (see Appendix 1) was assembled utilizing and reformatting the 2019 ISCD DXA TGNC positions4 into multiple-choice questions. Study data were collected and managed using REDCap® (Research Electronic Data Capture) electronic data capture tools hosted at the University of Kansas Medical Center [6,7]. REDCap® is a secure web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources [6,7]. Additional information inquired consisted of demographics, state of employment, DXA experience, and knowledge of the TGNC community. DXA scan performers and interpreters were recruited via institutional email addresses that were obtained from public hospital department websites. The method of gathering email addresses of interest consisted of searching medical institutions in all 50 states for radiology, endocrinology, and transgender health departments. Available emails were added to the REDCap distribution server. Survey participation invitations were sent to 3,502 individual email addresses, 6 consecutive times, over a period of 4 months. Researchers relied-on email recipients forwarding the survey to potential respondents to obtain additional responses. Total responses yielded 26 completed surveys, corresponding to a 0.7% response rate. Due to the small sample size, classic statistical analyses were unable to be performed. Instead, the data was evaluated qualitatively by calculating the “correct” versus “incorrect” responses when compared to the ISCD guidelines. The 2019 ISCD official positions for T- and Z-scores in DXA scans for TGNC individuals can be found in Appendix 2. If respondents applied ISCD 2019 position when performing and analyzing DXA scans, their response was deemed “correct” whereas if the respondents were not applying the 2019 ISCD guidance, their responses were deemed “incorrect.”
Results
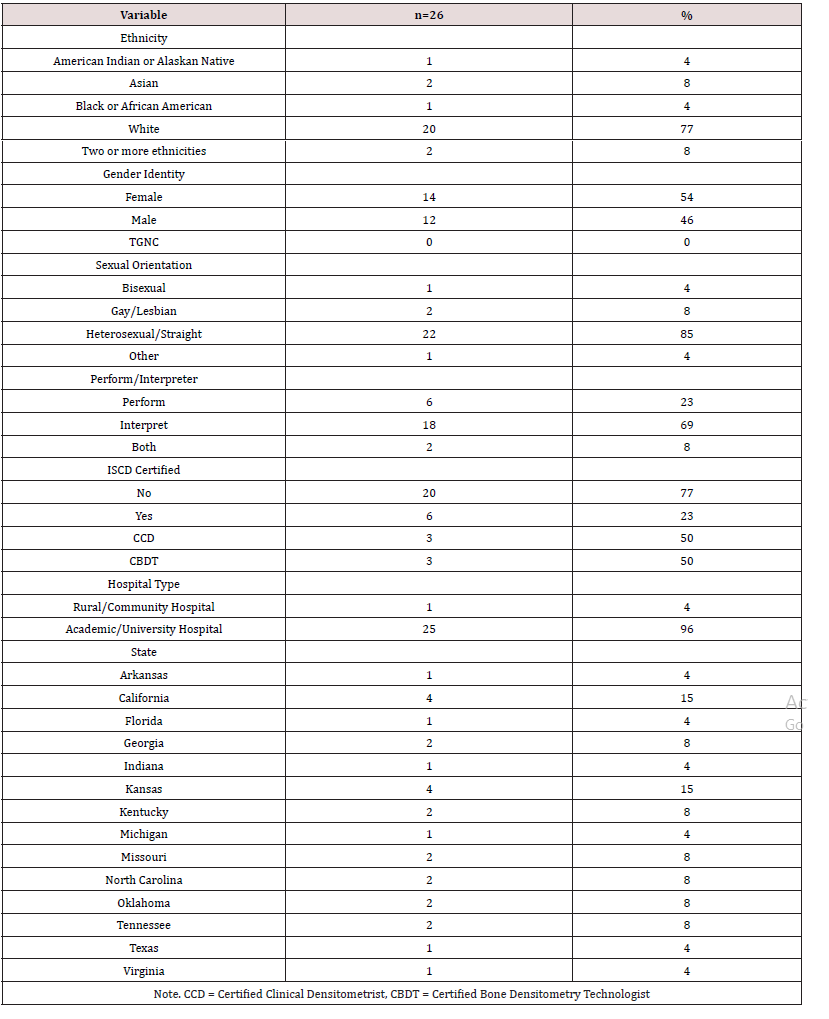
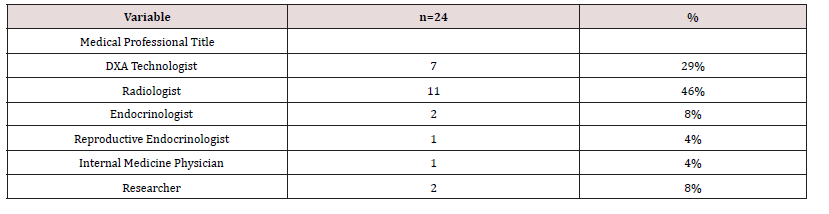
Due to the widespread distribution of the survey, a diverse survey respondent demographic was contacted and offered the opportunity for survey participation. Appendix 3, Table 1 shows the evenly distributed gender of survey takers, varying ethnicity, and sexual orientation, as well as a variety of DXA performers and interpreters. Furthermore, two individual respondents had experience in both performing and interpreting DXA scans, with the majority of responses originating from academic/university affiliated health systems. Additionally, 14 different states were represented. Finally, for survey taker demographic information, Radiologists and DXA Technologists comprised the majority of the survey takers though Endocrinologists, Reproductive Endocrinologists, Internal Medicine Physicians, and Researchers also were represented (Appendix 3, Table 2).
The majority of participants stated they found information regarding a patient’s sex and gender identity in the patient’s chart or electronic medical record, rather than asking at the time of the test. Participants also were given multiple-choice questions asking, “what reference database should be used for transgender individuals” for both T-scores and Z-scores, and “what reference database should be used for gender-nonbinary individuals” for both T-scores and Z-scores. Regarding responses for which reference database was applied for T-scores for transgender individuals, 41% of DXA scan performers and interpreters answered, “sex assigned at birth” or “unknown”. Among responses for gender-nonbinary individuals, 48% answered, “sex assigned at birth” or “unknown”.
Responses for T-score data for transgender and gendernonbinary individuals were widely incorrect. Specifically, T-scores for transgender individuals reported to be calculated incorrectly 15/20 (75%) by interpreters and 6/8 (75%) by performers, while gender-nonbinary individuals received incorrect calculations 16/20 (80%) by interpreters and 6/8 (75%) by performers. When asked for responses regarding which reference database was applied for Z-scores for transgender individuals, 56% of DXA scan performers and interpreters answered, “sex assigned at birth” or “unknown”. Among responses for gender-nonbinary individuals, 44% answered, “sex assigned at birth” or “unknown”. Furthermore, responses for calculations of Z-score data for transgender and gender-nonbinary individuals were also mostly reported incorrectly. Z-scores for transgender individuals was surveyed to be calculated incorrect 19/20 (95%) by interpreters with the most common answer “Race Adjusted, Aged Matched Database for the Individual’s Gender Identity” followed by “Unknown.” Additionally, Z-scores for transgender patients were calculated incorrectly by performers 8/8 (100%). For gender-nonbinary patients, Z-scores were calculated incorrectly 17/20 (85%) by interpreters and 7/8 (87%) by performers. Overall, comparing the survey responses to the 2019 ISCD official positions for DXA in transgender individuals, 75% of T-scores and 96% of Z-scores were deemed “incorrect”, with 79% of T-scores and 86% of Z-scores deemed “incorrect” in nonbinary individuals. Lastly, 11% of respondents indicated that their institution had a protocol for DXA scans in TGNC individuals, where the other 89% claimed they did not or did not know if there was a protocol.
Discussion
The TGNC population is an underrepresented population not only in society and healthcare, but in the realm of research. The research discrepancy largely is due to human subject data being categorized into only two sexes for demographics, sometimes even reported without dividing the sexes. Alarmingly, as recent as 2016, an article made the argument that studies should report sex and gender outcomes separately in order to facilitate future research and meta-analyses [8]. One such reason, described by Franconi et al. [9], is because effects of an intervention in one sex might be greater than in the other. Similarly, an intervention may affect an individual who has been receiving long-term gender affirming hormone therapies and/or gonadal surgeries differently. Ultimately, additional research regarding TGNC healthcare and genderaffirming hormone therapy is needed to understand bone health, fracture risk and healing, outcome disparities and care access across multiple subspecialties, and establishment of perioperative management guidelines [9].
With this said, an elevation of importance is demonstrated for gender identity specific dashboards and organ inventories in hospital electronic medical records [10], as this is where most healthcare professionals will go to gather information about the patient. Furthermore, without proper gender identity documentation, the patient is at risk of failing to be identified by the preferred name and pronoun in the medical setting which has been shown to have a profound impact on TGNC patients mental health and quality of care [11]. Additionally, bone health evaluation, incorrect treatment recommendations such as sex-based medication dosages, as well as increase the patient risk if laboratory tests are incorrectly paired with a different assumed hormonal history [12]. Altogether, it is advised that data on gender identity be recorded in electronic health records and that this goal be included into the important objectives [13].
Assuming a bone mineral density is addressed, and correct gender is identified, clinicians utilizing the literature to order or interpret a DXA scan will recognize the large amount of protocol variations and recommendations that exist. Numerous existing studies compare TGNC DXA scans to both male and female reference indices [3,16], while sex assigned at birth was also the reference index utilized by some previous studies. The overriding consensus from our survey was sex assigned at birth. While the ISCD TGNC DXA positions made their debut in 2019 [4], it should be noted all calculated T-scores for patients in all ethnic groups and genders should have been assigned to a uniform Caucasian (non-race adjusted) female reference database since 2013 [20], which contradicted most of the prementioned studies and survey responders. As discussed, this topic has been a subject of immense debate and confusion over the past decade, and the patient population in question would benefit from a well-studied, standardized DXA reference index.
Finally, comparing survey responses to the current positions put forth by the ISCD revealed an enormous health care discrepancy that needs to be addressed.Clinicians should work to improve models of individualized care by continuing to learn about social determinants which continue to hinder equitable care efforts [21]. 21 Considering the only current TGNC DXA positions were published by ISCD in 2019 [4], it is imperative that practicing DXA technicians and interpreters have knowledge about and access to these positions for the TGNC populations. Lastly, knowing clinical guidelines play an important role in optimizing the quality of patient care on the basis of evidence-based medicine [22], it is important to acknowledge that a dismal portion of surveyed institutions reported having guidelines for providing and/or interpreting DXA scans in the TGNC population. As knowledge in this area continues to expand, institutional protocols will help the healthcare team provide quality care to patients by identifying the correct service to provide as well as the best way to provide that service [23] and can inspire research, in particular regarding common diseases and/or illnesses as well as diagnostic uncertainty [25] such as bone health in the TGNC community.
significant limitation of this study was the small sample size due to a low response rate. As stated in Baruch et al. [25], there are 2 primary reasons for receiving low response rates from surveys which include failure to deliver the questionnaires to the correct population and the reluctance of survey response. In the present study, researchers saw both reasons. From the 3,502 email addresses collected, many emails were deemed “undeliverable” due to hospital firewall protections systems, with many other automatic replies that the individual was out of the office. Additionally, researchers experienced the reluctance of people to respond, judged by the number of negative email responses sent back to investigators without a concurrent survey response from the individual. Possible reasons for this hostility can stem from stressful work environments, politics, transphobia, or an overall lack of awareness for the TGNC population among survey recipients. Although the low response rate affects the power of the study, based on a meta-analysis, Cook et al. [26] argued response rate in survey research was less important than response representativeness. We had survey participants from 14 states, which was representative of all official regions in the United States. Other limitations included the use of multiple-choice questions in the survey because the participants were forced to pick an already formulated answer choice and were not given a free text space. The authors believed these limitations did not affect the validity of the study.
In conclusion, the bone health of individuals who identify as TGNC is in jeopardy due to the lack of knowledge and understanding of proper protocols surrounding the gold standard for the measurement of bone mineral density via DXA scan. The ISCD positions were published as a product of the only known large-scale clinical trials measuring the bone mineral density of persons who identify as TGNC. Until further prospective trials are conducted with a patient population that mimics the United States, the ISCD positions should be followed to assess accurately bone health in the TGNC population, and most importantly, to avoid missed osteoporosis diagnoses which can lead to significant patient morbidity, mortality and healthcare burden for these patients.
Acknowledgments
We thank Sharon Fitzgerald for assisting the research team in the evaluation of the statistics for this project.
References
- Safer JD, Tangpricha V (2019) Care of the Transgender Patient. Ann Intern Med 71(1): Itc1-itc16.
- Petak S, Barbu CG, Yu EW, et al. (2013) The Official Positions of the International Society for Clinical Densitometry: body composition analysis reporting. J Clin Densitom 16(4): 508-519.
- Dobrolińska M, van der Tuuk K, Vink P, et al. (2019) Bone Mineral Density in Transgender Individuals After Gonadectomy and Long-Term Gender-Affirming Hormonal Treatment. J Sex Med 16(9): 1469-1477.
- Rosen HN, Hamnvik OR, Jaisamrarn U, et al. (2019) Bone Densitometry in Transgender and Gender Non-Conforming (TGNC) Individuals: 2019 ISCD Official Position. J Clin Densitom 22(4): 544-553.
- Walcott Q, Dallman J, Crow H, Graves L, Marsh C (2022) DXA Scan Variants in Transgender Patients. J Clin Densitom 25(4):615-621.
- Harris PA, Taylor R, Minor BL, et al. (2019) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95: 103208.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2): 377-381.
- Clayton JA, Tannenbaum C (2016) Reporting Sex, Gender, or Both in Clinical Research? JAMA 316(18): 1863-1864.
- Ramsey DC, Lawson MM, Stuart A, Sodders E (2021) Working ZM. Orthopaedic Care of the Transgender Patient. J Bone Joint Surg Am 103(3):274-8.
- Deutsch MB, Green J, Keatley J, Mayer G, Hastings J, et al. (2013) Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J Am Med Inform Assoc 20(4): 700-703.
- Mizock L, Lewis TK (2008) Trauma in Transgender Populations: Risk, Resilience, and Clinical Care. Journal of Emotional Abuse 8(3): 335-354.
- Burgess C, Kauth MR, Klemt C, Shanawani H, Shipherd JC (2019) Evolving Sex and Gender in Electronic Health Records. Fed Pract 36(6): 271-277.
- Institute of Medicine (US) Committee on Lesbian G, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington (DC): National Academies Press (US) 2011.
- Broulik PD, Urbánek V, Libanský P (2018) Eighteen-Year Effect of Androgen Therapy on Bone Mineral Density in Trans(gender) Men. Horm Metab Res 50(2): 133-137.
- Haraldsen IR, Haug E, Falch J, Egeland T, Opjordsmoen S (2007) Cross-sex pattern of bone mineral density in early onset gender identity disorder. Horm Behav 52(3): 334-343.
- Fighera TM, da Silva E, Lindenau JD, Spritzer PM (2018) Impact of cross-sex hormone therapy on bone mineral density and body composition in transwomen. Clin Endocrinol (Oxf) 88(6): 856-862.
- Van Caenegem E, Wierckx K, Taes Y, et al. (2012) Bone mass, bone geometry, and body composition in female-to-male transsexual persons after long-term cross-sex hormonal therapy. J Clin Endocrinol Metab 97(7): 2503-2511.
- Wierckx K, Mueller S, Weyers S, et al. (2012) Long-term evaluation of cross-sex hormone treatment in transsexual persons. J Sex Med 9(10): 2641-2651.
- Wiepjes CM, de Jongh RT, de Blok CJ, et al. (2019) Bone Safety During the First Ten Years of Gender-Affirming Hormonal Treatment in Transwomen and Transmen. J Bone Miner Res 34(3): 447-454.
- Watts NB, Leslie WD, Foldes AJ, Miller PD (2013) International Society for Clinical Densitometry Position Development Conference: Task Force on Normative Databases. J Clin Densitom 16(4): 472-481.
- Nesbitt S, Palomarez RE (2016) Review: Increasing Awareness and Education on Health Disparities for Health Care Providers. Ethn Dis 26(2): 181-190.
- Bottrighi A, Molino G, Montani S, Terenziani P, Torchio M (2013) Supporting a distributed execution of clinical guidelines. Comput Methods Programs Biomed 112(1): 200-210.
- Heymann T (1994) Clinical protocols are key to quality health care delivery. Int J Health Care Qual Assur 7(7): 14-17.
- Fink W, Kamenski G, Konitzer M (2018) Diagnostic protocols-A consultation tool still to be discovered. J Eval Clin Pract 24(1): 293-300.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...