Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5945
Case Report(ISSN: 2638-5945) 
Exercises Program in Breast Cancer Patient with Chemotherapy Induced Peripheral Neuropathy: A Case Study. Volume 5 - Issue 4
Khulood Alrashid* and Shahd Al Shehri
- Department of cancer, Saudi Arabia
Received: November 28, 2023 Published: December 13, 2023
Corresponding author: Khulood Alrashid, Department of cancer, Saudi Arabia.
DOI: 10.32474/OAJOM.2023.05.000217
Abstract
Background: Breast cancer is one of the most common cancers in women worldwide, accounting for approximately 570,000 deaths in 2015. Over 1.5 million women (25% of all women with cancer) are diagnosed with breast cancer every year throughout the world. One of the most common complications after breast cancer surgery is functional limitation of the upper body. Up to 67% of breast cancer patients experience arm or shoulder impairment, including pain, numbness, loss of strength, and reduced ROM, after surgery. Breast cancer patients are presenting with chemo-induced peripheral neuropathy (CIPN) that is impacting their balance, quality of life, and overall participation, as a side effect of chemotherapy treatment.
Study Design: This case study was used to highlight the role of physical therapy interventions in the management of Breast cancer patient after surgery with chemo-induced peripheral neuropathy.
Case Description: A 55-years-old Saudi female, known case of diabetes mellitus on insulin, hypertension and history of DVT 27 years back on anticoagulant. She came to the combined clinic breast clinic and all workup and investigations were done and showed invasive ductal carcinoma. Referred to physical therapy department by breast and endocrine clinic for left shoulder limited range of motion, impaired mobility and managing the symptoms.
PT management and outcome: The patient received 2 phases of rehabilitations, phase 1 the patient was seen once a week for 4 weeks, phase 2 the patient was seen 3 times per week for 6 weeks. Exercise program of patient education, therapeutic exercise of low- to - moderate intensity resistance exercise for UE and LE. Aerobic Exercise; Cardio bike progressive training for UE and LE and balance exercise. By the end of phase 1 patient’s ROM and pain improved significantly, and by the end of phase 2 of the rehabilitation program, patient’s balance (using BBS), functional ability and QOL using (FACT-B) improved.
Discussion: This case study showed that physical therapy exercise program including therapeutic exercises, low- to moderateintensity resistance exercise, aerobic exercise, balance exercise is an effective program for breast cancer patients as it improves CIPN, minimize dependency and improved QOL.
History
Breast cancer is one of the most common cancers in women worldwide, accounting for approximately 570,000 deaths in 2015. Over 1.5 million women (25% of all women with cancer) are diagnosed with breast cancer every year throughout the world [1,2].
Breast cancer treatment options are based on the type of breast cancer, its stage and grade, size, and whether the cancer cells are sensitive to hormones. Doctors also consider the overall health and patient’s own preferences. Most women undergo surgery for breast cancer and many also receive additional treatment after surgery, such as chemotherapy, hormone therapy or radiation. Chemotherapy might also be used before surgery in certain situations [3].
One of the most common complications after breast cancer surgery is functional limitation of the upper body. Up to 67% of breast cancer patients experience arm or shoulder impairment, including pain, numbness, loss of strength, and reduced ROM, after surgery [4,5].
Breast cancer patients presenting with chemo-induced peripheral neuropathy (CIPN) that is impacting their balance, quality of life, and overall participation, as a side effect of chemotherapy treatment that are amenable to physical rehabilitation should be referred to PT as soon as identified.
Study Design
This case study was used to highlight the role of physical therapy interventions in the management of Breast cancer patient after surgery with chemo-induced peripheral neuropathy.
Case Description
Patient History
A 55-years-old Saudi female, known case of diabetes mellitus on insulin, hypertension and history of DVT 27 years back on anticoagulant. She has a family history of various cancers, her sister with uterine cancer, grandmother with stomach cancer and brother with brain cancer, he passed away at young age. The patient had a left breast lump (around 2.5 cm mass on 2-3 o’clock, hard, no skin changes) for two months, increasing in size. Patient was seen in the Combined Clinic, all workup and investigations were done and showed invasive ductal carcinoma, stage at Presentation cT2N1M0, ER PR positive and Her-2 negative, Ki67-90%.
Diagnostic Mammogram and US showed BI-RADS 6: Known biopsy proven malignancy. Nuclear bone scan showed no scintigraphic evidence of osteoblastic bone metastasis. CT Chest, abdomen and pelvis showed no definite distant metastasis.
This case was discussed in the Tumor Board and the decision was to receive neoadjuvant chemotherapy, and the patient received four cycles of Taxotere and Cyclophosphamide. followed by surgery: left wire localization lumpectomy plus sentinel lymph node biopsy. Adjuvant radiation therapy to left breast, axilla and supraclavicular fossa for 15 fractions over 3 weeks and hormonal therapy. She was referred to physical therapy department by breast and endocrine clinic for left shoulder limited range of motion and impaired mobility. During the first session a full assessment of the patient was carried out including setting long and short-term goals.
Long term goals: Were that the patient to maximize left shoulder range of motion and strength. To decrease pain at left upper quadrant, to maximize independence with functional activities and to be independent with home exercise program.
Long term goals to be met within 3 months. As for the shortterm goals: they were to reduce pain by 25-50%, to increase her left shoulder range of motion, to be independent with home exercise program.
Examination
Observation
• Skin: Tight, hard as a result of the surgery and radiation therapy.
• Scars: Lumpectomy scar, healed.
• Wounds: None.
• Edema: Left breast edema, minimal hardness and fibrosed.
Palpation/Skin and scar assessment
• Assessment of skin tissue texture: dry skin.
• Assess scar tissue: None.
Pain
Left shoulder and left upper quadrant tightness and pain.
Graded 10/10 using adult communicative / numeric intensity pain scale.
Pain increased with left arm overhead activities.
General body / joints pain with walking long distance.
Sensation
• Patient reported chemo-induced peripheral neuropathy in her hands and feet.
ROM
Right shoulder movement: Within functional limit.
Left shoulder:
Flexion= 100 degrees
Abduction= 120 degrees
Internal and external rotations= within normal limit.
Functional Status
The patient’s functional abilities were severely affected due to the side effects of the treatments she underwent.
Transfer and walking
Patient is modified independent in transfer using standing pivot technique.
Gait
Patients can walk only for short distances and use wheelchair for long distance.
Functional Assessment of Cancer Therapy – Breast (FACT-B)
Scored= 62.5
Berg balance scale (BBS)
Scored= 49 (Low fall risk)
Findings
Patient presents with limited left shoulder ROM, generalized body / joint pain, impaired mobility. All mentioned problems contributed to her functional dependency.
As consequences of her functional dependency resulted from the cancer treatment side effects, the patient lost her job and became unemployed, which affected her psychologically, socially and financially.
Intervention
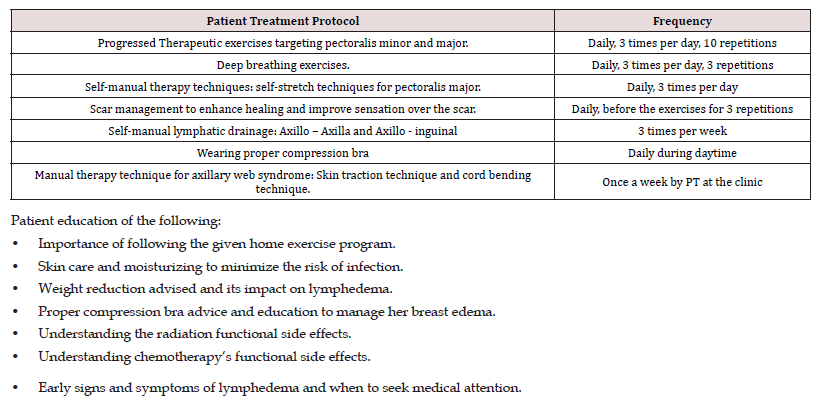
Initially, at phase 1 the patient was seen once a week for 4 weeks at the physical therapy outpatient clinic, focusing on patient education, therapeutic exercise and manual therapy for left shoulder ROM, pain and edema. Patient treatment protocol phase 1 at (Table 1).
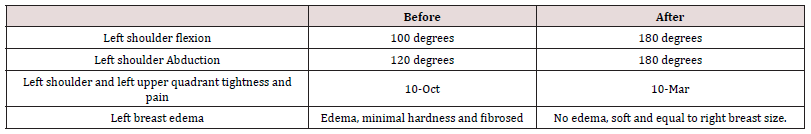
Outcomes after 4 weeks / 4 sessions end of phase 1: Outcomes at (Table 2).
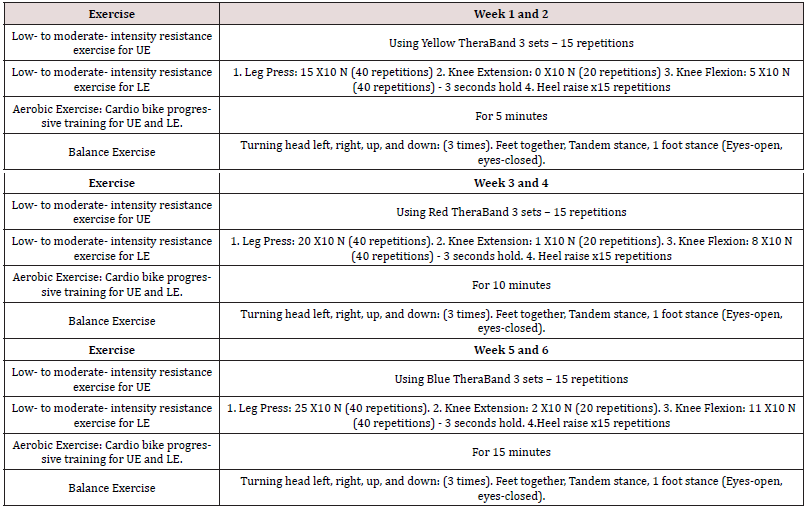
Phase 2 of the intervention, the patient was seen at the gym for low- to moderate- intensity resistance exercise for UE and LE. Aerobic Exercise; Cardio bike progressive training for UE and LE and balance exercise [6,7,8,9,10]. 3 times per week for 6 weeks, exercise program at (Table 3).
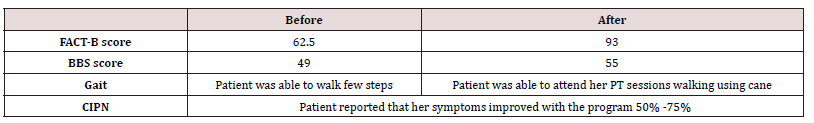
Outcomes after 6 weeks / 18 sessions end of phase 2: Outcomes at (Table 4).
At the last session
The patient reported that she is very satisfied with the physical therapy program provided to her
Follow up after 6 months.
Patient reported that she is compliant with exercises, being physically active and she reported that she is now employed working at school which affected her socially and financially status positively.
Discussion
Breast cancer is one of the most common types of cancer in women worldwide [1]. Breast cancer patients face an array of problems and have specific needs which must be addressed to prevent long term functional limitations and disability. Upper limb dysfunction and decreased quality of life are frequently reported sequelae of early-stage breast cancer treatment.
Based on the result, we supported the physical therapy exercise program including patient education, therapeutic exercise, manual therapy, edema management, low- to moderate- intensity resistance exercise for UE and LE, Aerobic exercise, Cardio bike progressive training for UE and LE and balance exercise in the treatment of breast cancer patient post breast surgery limitations, radiation and chemotherapy functional side effects.
That goes with Ian R. Kleckner (2017) who proved that exercise reduces CIPN symptoms in patients receiving taxane-, platinum-, or vinca alkaloid-based chemotherapy [6]. Shaoning Guo (2022) showed that combined exercise could be an effective option for improving quality of life, physical function (balance control and muscle strength), and neuropathic pain in cancer patients with chemotherapy-induced peripheral neuropathy [9].
In general, balance training is known to induce neuronal adaptations and improve muscular output leading to enhanced postural control [11,12]. It is well known that patients with a proprioceptive deficit such as peripheral neuropathy suffer from postural instability [13], as do patients with CIPN [14,15].
This case study provides a good learning opportunity for the physical therapist to be able to design a complete plan of treatment for breast cancer patients suffering from the mentioned symptoms and treatment’s side effects. Further exploration of appropriate exercise prescriptions is needed.
Conclusion
The physical therapy exercise program including therapeutic exercises, low- to moderate- intensity resistance exercise, aerobic exercise, balance exercise is an effective program for breast cancer patients as it improves CIPN, minimize dependency and improved QOL.
Acknowledgement
None.
Conflicts of Interest
No conflicts of interest.
References
- McGuire S (2016) World Cancer Report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press, 2015. Advances in Nutrition 7(2): 418–419.
- World Health Organization (2023). Breast cancer. [online] www.who.int.
- Mayo Clinic (2022) Breast cancer - Diagnosis and treatment - Mayo Clinic. [online] Mayoclinic.org.
- Verbelen H, Tjalma W, Meirte J and Gebruers N (2019) Long‐term morbidity after a negative sentinel node in breast cancer patients. European Journal of Cancer Care 28(5).
- Lee TS, Kilbreath SL, Refshauge KM, Herbert RD and Beith JM (2007) Prognosis of the upper limb following surgery and radiation for breast cancer. Breast Cancer Research and Treatment 110(1): 19-37.
- Kleckner IR, Kamen C, Gewandter JS, Mohile NA, Heckler CE, et al. (2017) Effects of exercise during chemotherapy on chemotherapy-induced peripheral neuropathy: a multicenter, randomized controlled trial. Supportive Care in Cancer 26(4): 1019-1028.
- Kneis S, Wehrle A, Muller J, Maurer C, Ihorst G, et al. (2019) It’s never too late - balance and endurance training improves functional performance, quality of life, and alleviates neuropathic symptoms in cancer survivors suffering from chemotherapy-induced peripheral neuropathy: results of a randomized controlled trial. BMC Cancer 19(1): 414.
- Zimmer P, Trebing S, Timmers-Trebing U, Schenk A, Paust R, Bloch W, et al. (2018) Eight-week, multimodal exercise counteracts a progress of chemotherapy-induced peripheral neuropathy and improves balance and strength in metastasized colorectal cancer patients: a randomized controlled trial. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer [online] 26(2): 615–624.
- Guo S, Han W, Wang P, Wang X, Fang X (2022) Effects of exercise on chemotherapy-induced peripheral neuropathy in cancer patients: a systematic review and meta-analysis. Journal of Cancer Survivorship 17(2): 318-331.
- com. (n.d.). Strength and Conditioning: Biological Principles and Practical Applications | Wiley. [online].
- Taube W, Gruber M, Gollhofer A (2008) Spinal and supraspinal adaptations associated with balance training and their functional relevance. Acta Physiol (Oxf) 193(2):101-116.
- Zech A, Hubscher M, Vogt L, Banzer W, Hansel F, et al. Balance training for neuromuscular control and performance enhancement: a systematic review. J Athl Train 45(4): 392-403.
- Van Schie CHM (2008) Neuropathy: mobility and quality of life. Diabetes Metab Res Rev 24(Suppl1): 45-51.
- Wampler MA, Topp KS, Miaskowski C, Byl NN, Rugo HS, et al. (2007) Quantitative and clinical description of postural instability in women with breast Cancer treated with Taxane chemotherapy. Arch Phys Med Rehabil 88(8): 1002-1008.
- Monfort SM, Pan X, Patrick R, Ramaswamy B, Wesolowski R, et al. (2017) Gait, balance, and patient-reported outcomes during taxane-based chemotherapy in early-stage breast cancer patients. Breast Cancer Res Treat 164(1): 69–77.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...