Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5945
Research Article(ISSN: 2638-5945) 
Diverticulitis Treatment Strategies in A District General Hospital - A Cross-Sectional Study from United Kingdom Volume 4 - Issue 4
George Bishet, Yahya Salama A Salama*, Mohammed Qayum., Lava Krishna Kannappa
- Department of Surgery, Kettering general hospital, Queen Elizabeth Hospital, Birmingham, Hereford Hospital, United Kingdom
Received:June 26, 2021 Published: July 09, 2021
Corresponding author: Yahya Salama A Salama, Department of Surgery, Kettering general hospital, Queen Elizabeth Hospital, Birmingham, Hereford Hospital, United Kingdom
DOI: 10.32474/OAJOM.2021.04.000195
Introduction
The incidence of diverticulosis among the population in the western world is a common occurrence known amongst the medical fraternity. The spectrum of presentation for diverticulitis varies being asymptomatic to life-threatening sepsis with perforation requiring surgery. The prevalence of diverticulosis increases by age with about 10% I under 40 years of age, over 50 % over 50 years of age and increasing to 70% by 80 years of age [1]. A vast majority of the patients of roughly 75 with diverticulosis are asymptomatic [2]. As per NICE (National institute of clinical excellence) guidelines in the UK (United Kingdom), Watchful watching is advised for patients if they are systemically well, If the patient if the person is systemically unwell but does not meet the criteria for referral with suspected complicated acute diverticulitis. The evidence supports the current practice of treating an acute episode of diverticulitis with intravenous antibiotics in secondary care. Based on the Computer tomography (CT) scan findings, for uncomplicated Diverticulitis on CT scan, the recommendations are to start on oral antibiotics and would not affect the outcome. Watchful waiting can lead to an increase in recurrence rates and antibiotics resistance. Nice recommends patient reassessed in 48 hours for the need for intravenous antibiotics or repeat CT shows evidence of abscess and the total course of antibiotics would be for 5 days which have been debated and questioned [3]. The impact of COVID-19 and the change in the treatment strategies and their impact should be assessed and the objective of this study was to see how the patients were treated during this period and the implication and any findings to reflect and implement. Several risk factors have been associated with diverticulitis. Bolkenstein et al (2017) [4] systematic review and meta-analysis on risk factors for complicated diverticulitis showed the risk factors as people with age more than 70 years [5] and 63.9 years [6] and uncomplicated diverticulitis at 57.1 years [6]. The absolute risk of developing complicated diverticulitis varied from 9-46% in women and 16 to 59% in men respectively. The clinical signs and symptoms included nausea [7], vomiting [8], bloating [6] and constipation [7] for complicated diverticulitis and severe constipation, abdominal pain with increased rectal blood loss for severe complicated diverticulitis [8]. In regards to body temperature, Temperature greater than 37 °C was associated with complicated diverticulitis and less than 37.0 Celsius associated with uncomplicated diverticulitis. The overall mean C- reactive protein (CRP) for patients with uncomplicated diverticulitis was 68 mg/L with a range of 25 to 96 mg/L. This was 186 mg/L with a range of 134 to 224 mg/L among patients with complicated diverticulitis [4]. The objective of our study was to discern the uncomplicated and complicated diverticulitis treated based on Modified Hinchey classification and re-evaluate the management and present our findings.
Diverticulitis Classification
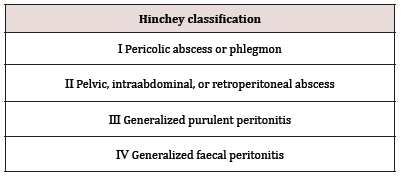
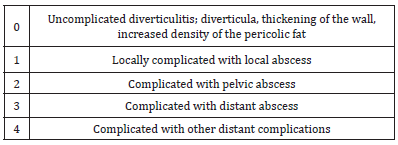
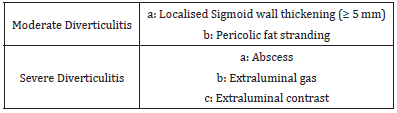
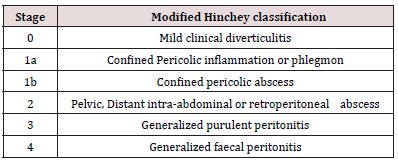
In 1978 Hinchey introduced the first classification of acute diverticulitis [9]. The Hinchey classification has been widely used in the literature for the last 30 years [Table 1]. Since the CT scan has become used widely in every hospital, The classifications have undergone several modifications based on the information from the CT scan findings. Neff et al in 1989 [10] introduced a new classification based on CT findings and included 5 stages as below Table 2. Ambrosetti, et al. in 2002 [11] classified acute diverticulitis based on CT findings as below Table 3. In 2005, Kaiser, et al. [12] modified the Hinchey classification according to specific CT findings and is shown as below Table 4.
Materials and methods
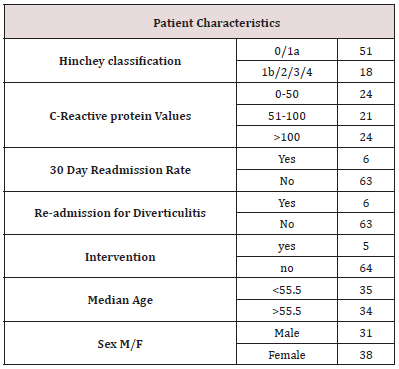
Our study used modified Hinchey classification for stratifying the patients with diverticulitis treated Conservatively. The patient dataset contained patient characteristics information between the period of 1/5/2019 till 31/10/2019 of 6 months and included 69 patients in total along with their CT (Computer tomography) scan findings. The patient characteristics are as shown in Table 5. The uncomplicated group included Hinchey 0/1A classification and the complicated group was Hinchey 1b/2/3/4 classification respectively.
Statistical analysis
The data was collected in a Microsoft Excel spreadsheet and the statistical analysis of Ordinal regression analysis was done by using SPSS 27.0.
Ordinal Regression Analysis
An ordinal linear regression analysis was run to predict Modified Hinchey classification (0/1A vs 1b/2/3/4 = Uncomplicated vs complicated diverticulitis) with CRP, Length of stay, Readmission for diverticulitis or other reasons, interventions included surgery, gender, median age and gender. The regression analysis was statistically significant only for CRP < 50 and length of days the maximum being 5.441 days. The final model statistically significantly predicted the dependent variable for the group (Modified Hinchey classification (0/1A) over and above the intercept-only model, χ2(4) = 29.368, p < .001.The odds ratio of being in the uncomplicated diverticulitis group (Modified Hinchey classification (0/1A) dependent variable for (CRP -0-50) was 0.54, 95% CI [0.004, 0.724], a statistically significant effect, Wald χ2(1) = 4.857, p = .028. The odds of (CRP-50-100) was similar to that of (CRP- >100) to be not associated with uncomplicated diverticulitis group (Modified Hinchey classification (0/1A) dependent variable was (odds ratio of 0.349, 95% CI [0.068, 1.805]), Wald χ2(1) = 1.575, p = .209 which was not statistically significant. An increase in length of stay (expressed in days) was associated with an increase in the odds of being in uncomplicated diverticulitis group (Modified Hinchey classification (0/1A), with an odds ratio of 2.060, 95% CI [1.140, 3.721], Wald χ2(1) = 5.730, p < .017. The length of stay varied from 0-14 days with the mean being 2.91 (IQR -0-14, Sd-2.531). The maximum number of days associated with uncomplicated diverticulitis was 5.441 days.
Discussion
Even though there are several guidelines in regards to the treatment of diverticulitis in respective countries all over the world, there is always a conundrum to stratify patient who can be categorised as complicated and uncomplicated diverticulitis and does not seem to be straightforward and posed enormous challenge during decision-making times. In our study, we came to the conclusion, that a CRP of less than 50 was associated with uncomplicated diverticulitis (Hinchey 0/1A) classification and is amenable for conservative treatment. Three (3/51) patients with uncomplicated diverticulitis went on to have readmission with further antibiotics and one surgical intervention out of 51 patients estimated at 1.96 %. On the other hand, Three out of eighteen patients (4/18) with complicated diverticulitis (Hinchey 1b/2/3/4) went on to have readmission for further treatment with surgery estimated at 22.22 %. This is in accordance with other studies in the literature. Bates, et al. (2018) study to assess whether CT (Computer Tomography) scan findings, Clinical parameters and modified Hinchey classification are predictive of management outcomes in acute diverticulitis showed that, CT findings of the presence of Pericolonic fluid collection, Colonic fistula, Extraluminal air, bowel obstruction and Modified Hinchey score of 1b or higher with low Blood pressure were associated with Operative management [13]. CRP has been identified as a useful biomarker of inflammation and is useful in the prediction of the clinical severity of acute diverticulitis. Several studies have reported different levels with no accuracy. Van der wall et al study of 426 patients which included 364 (85%) with uncomplicated diverticulitis estimated CRP was of sufficient diagnostic value (Area under Curve 0.715). The median CRP in patients with complicated diverticulitis was significantly higher than in patients with the uncomplicated disease (224 mg/l, range 99–284, vs. 87 mg/l, range 48–151, respectively). Patients with a CRP of 25 mg/l had a 15% chance of having complicated diverticulitis. This increased from 23% at a CRP value of 100 mg/l to 47% for 250 mg/l or higher. The optimal threshold was reached at 175 mg/l with a positive predictive value of 36%, negative predictive value of 92%, sensitivity of 61%, and specificity of 82%6. Markela et al study Comparing CRP levels in 350 patients with first presentation predicted a cut off level of 149.5 mg/l as a discriminatory level for acute uncomplicated diverticulitis and a level of more than 150 mg/l for complicated diverticulitis. The mean CRP value was significantly higher in the patients who died (mean CRP of 207 mg/l) than in those who survived (mean CRP of 139 mg/l) and concluded the CRP value higher than 150 mg/l have increased risk for complicated diverticulitis and warrants a CT examination. Kechagias et al study of Ninety-nine patients showed eighty-eight patients with Hinchey 1a/1b and Hinchey > 1b had mean CRP od 80 mg/l and 236 mg/l respectively. The study also showed index CRP was the only independent predictor for Hinchey > 1b and a CRP level of > 173 mg/l obtained at initial evaluation at the emergency department will have complications and require urgent percutaneous drainage or surgical management [14]. The 2020 update of the world society of emergency surgery concluded that CRP values might have not raised to the levels at presentation as there is a delay of 6-8 hours from the onset of the disease reaching the peak at 48 hours so exercise caution using CRP as a marker to rule out acute diverticulitis [15]. Our study findings included Hinchey 0/1a is significantly associated with uncomplicated diverticulitis with CRP < 50. The Study has a small dataset of 69 patients treated and a larger cohort will be needed for the study in the future. The number of patients treated conservatively for Hinchey 0/1a (uncomplicated diverticulitis) vs Hinchey 1b/2/3/4 (Complicated diverticulitis) having surgery was at 1.96% and 22.22% respectively.
Conclusion
The study presents a cohort of 69 patients treated conservatively in a district general hospital in the United Kingdom. The study findings showed the Hinchey 0/1a grade is strongly associated with uncomplicated diverticulitis and a CRP < 50 ideal for Conservative management with surgical intervention rate of 1.96% for uncomplicated diverticulitis (Hinchey 0/1A) classification grade and 22.22 % for complicated diverticulitis (Hinchey 1b/2/3/4).
References
- Convener’s handbook - commissioning-guide-colonic-diverticular-disease-RCS-2014.
- Diverticular disease: Diagnosis and management.
- Org.
- Bolkenstein HE, van de Wall BJM, Consten ECJ, Broeders IAMJ, Draaisma WA (2017) Risk factors for complicated diverticulitis: Systematic review and meta-analysis. Int J Colorectal Dis 32(10): 1375-1383.
- Makela JT, Klintrup K, Takala H, Rautio T (2015) The role of C-reactive protein in prediction of the severity of acute diverticulitis in an emergency unit. Scand J Gastroenterol 50(5): 536-541.
- van de Wall BJ, Draaisma WA, van der Kaaij RT, Consten EC, Wiezer MJ, et al. (2013) The value of inflammation markers and body temperature in acute diverticulitis. Colorectal Dis 15(5):621-626.
- Longstreth GF, Iyer RL, Chu LH, et al. (2012) Acute diverticulitis: Demographic, clinical and laboratory features associated with computed tomography findings in 741 patients. Aliment Pharmacol Ther. 36(9):886-894.
- Tursi A, Brandimarte G, Giorgetti G, Elisei W, Maiorano M, et al. (2008) The clinical picture of uncomplicated versus complicated diverticulitis of the colon. Dig Dis Sci 53(9): 2474-2479.
- Hinchey EJ, Schaal PG, Richards GK (1978) Treatment of perforated diverticular disease of the colon. Adv Surg 12: 85-109.
- Neff CC, vanSonnenberg E (1989) CT of diverticulitis. diagnosis and treatment. Radiol Clin North Am 27(4): 743-752.
- Ambrosetti P, Becker C, Terrier F (2002) Colonic diverticulitis: Impact of imaging on surgical management -- a prospective study of 542 patients. Eur Radiol 12(5): 1145-1149.
- Kaiser AM, Jiang JK, Lake JP, Glenn Ault, Avo Artinyan, et al. (2005) The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005;100(4):910-917.
- Bates DDB, Fernandez MB, Ponchiardi C, et al. (2018) Surgical management in acute diverticulitis and its association with multi-detector CT, modified hinchey classification, and clinical parameters. Abdom Radiol (NY) 43(8): 2060-2065.
- Kechagias A, Sofianidis A, Zografos G, Leandros E, Alexakis N, et al. (2018) Index C-reactive protein predicts increased severity in acute sigmoid diverticulitis. Ther Clin Risk Manag 14: 1847-1853.
- Sartelli M, Weber DG, Kluger Y (2020) 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg 15(1):32-020-00313-4.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...