Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5752
Review Article(ISSN: 2690-5752) 
Sicher, Sicker, Schicker, Sicca: are we Really Sure (Sind Wir Uns Wirklich Sicher) that Skull Alterations Attributed to Syphilis are Sicker Versions of Caries Sicca or is the Prepared Mind Just Seeing What it is Prepared to See? Volume 5 - Issue 2
Bruce Rothschild*
- IU Health, 2401 W University Ave, Muncie, IN, USA 47303, Carnegie Museum, 4400 Forbes Ave, Pittsburgh, PA, USA-15213
Received:September 20, 2021 Published: October 06, 2021
Corresponding author: Bruce Rothschild, IU Health, 2401 W University Ave, Muncie, IN, USA 47303, Carnegie Museum, 4400 Forbes Ave, Pittsburgh, PA, USA-15213
DOI: 10.32474/JAAS.2021.05.000210
Abstract
Background: Given disparate suggestions as to the origin and geographic distribution of syphilis, it seemed appropriate to examine the premises for the speculations that have been suggested for its recognition. Those premises that were pathognomonic (definitively diagnostic) are identified as such on the basis of precise definitions. It was hypothesized that the more observations differ from the original reports that establish definitive criteria, the greater the likelihood of diagnostic uncertainty. It was hypothesized that Hackett’s attribution of various skull changes to syphilis strayed from Virchow’s original description, was purely speculative in nature and had not been subjected to independent scientific scrutiny.
Methods: New populations with clinically diagnosed syphilis were therefore examined to assess the presence of caries sicca as originally defined and for those which were claimed to be stages of the spectrum of that phenomenon. Museum collections were also examined for presence of the specimens illustrating both varieties.
Results: Caries sicca, as originally defined by Virchow, was identified individuals from populations diagnosed in life with syphilis. Other forms attributed as “stages” of caries sicca were not found in that group. Museum collections with such “stages” lacked examples of caries sicca as originally defined.
Discussion: Epidemiologic co-occurrence of Virchow’s caries sicca and “more advanced cases” was not demonstrated (Fisher exact test, p < 0.00001). It was suggested that clarity, as to the origin and geographic distribution of syphilis through time, would result from extirpation of studies which failed to utilize the above-delineated criteria as originally vetted.
Keywords: Syphilis; Paleopathology; History of Disease; Biological Spectrum
Abbreviations: Venereal Disease Research Laboratory (VDRL), Systemic Lupus Erythematosus (SLE)
Highlights
a) Classic caries sicca, as defined by Virchow and the other skull pathologies attributed to syphilis appeared to represent disparate phenomena.
b) They seemingly are not even found in the same sample.
c) Serial radiographs have not documented progression between stages
d) Perhaps clarity, as to the origin and geographic distribution of syphilis through time, will result from extirpation of studies which fail to use as originally vetted.
Introduction
Premises for diagnosis
In 1995, an evidence-based suggestion was offered that not only allowed recognition of treponemal disease, but actually allowed distinguishing among them [1]. Some anthropologists (e.g., Baker, Cook, Powell, Sanford, Stodder) found this science-based perspective so inconvenient that they banded together to attempt to denigrate that consideration [2]. The validity or lack thereof related to their claims is moot, since they and others have since instead embraced continued use of an approach with which they had been comfortable. The alternative for identification of syphilis would be recognition of pathognomonic (definitively diagnostic) alterations. The two findings pertinent to confident recognition of syphilis were caries sicca and those dental alterations attributed to congenital syphilis. Criteria utilized to identify iterations (i.e., “stages”) suggested for the first of those phenomena, caries sicca, were assessed to identify what had been causally related, what remained speculative and if they were indeed pathognomonic (diagnostically specific for diagnosis of treponemal disease).
Evidence-based recognition of caries sicca
Caries sicca was a phenomenon which had been suggested as pathognomonic specifically for syphilis [3], although there is admission that it can occur with other forms of treponematosis [4,5]. [3] used the term caries sicca to describe a very specific cranial pathology, a scar with radiating arms in the outer cortex of the external table of the skull, which [6] referred to as a stellate depression. [6] stated that the “lesion starts as a stellate depression in the outer cortex of the external table of the skull. This then increased in circumference and depth. “A shallow funnel shaped pit is formed on the surfaced of the bone. The canals radiating from the starting point are opened up in a similar manner and those lying on the surface are converted into tortuous grooves.” [3] was quite specific as to what is not present or diagnostic of caries sicca:
a. Man könnte dieselbe als Caries sicca oder als entzündliche Atrophie der Knochenrinde Nitchewbezeichnen, denn sie findet sich stets an der Oberfläche und ich sah keinen [3]. This is translated as: It could be called caries sicca or as inflammatory atrophy of the bony cortex, because it is always on the surface and I saw no case of which would have been accompanied by suppuration.
b. Niemals habe ich hier irgend eine Spur von Eiter wahrgenommen, und wenn man den Prozess noch als [3]. This is translated as: I never have here perceived a trace of pus, and when looking at the process afterwards as caries.
Speculation-based recognition of caries sicca
A century after Virchow, [7], suggested a very different pattern, characterizing the initial stage as clustered and confluent pits, suggesting that the pathology subsequently developed focal superficial cavitation, circumvallate cavitation and formation of distinctive radial scars. Review of his work provided insights. He apparently derived his stages from examination of skulls from disparate sources/populations with “authentic diagnoses,” suggesting that some of which have the “sicca sequence.” The term “disparate” was used remind readership that Hackett’s “stages” were not actually found in a single sample, but rather as isolated examples derived from separate groups. Thus, there was no evidence that “stages” were actually related. Hackett that reported few diagnosed skulls available for comparison and noted, with the exception of radial scars, that pyogenic and tuberculosis-derived osteomyelitis manifest findings were indistinguishable from those (stages) he attributed to syphilis. With the exception of what he referred to as “diagnosed skulls,” it seems unclear whether he attributed the findings in the other skulls he examined to syphilis in a pre or post hoc manner. Was attribution to syphilis based on his expectation of their appearance, predicated on his untested hypothesis? That would seem to represent circular reasoning.
Intriguingly, [7] identified caries sicca as the final stage (from earliest to healed) in syphilitic skull lesions. He claimed that pits gave rise to focal, then circumvallate and then serpiginous cavitation, inserting radial scars between the last two, followed by nodular cavitation and finally caries sicca. One wonders what he is describing, when he distinguishes radial scars (the [3] definition of caries sicca) from caries sicca? On page 363, in table 1a, he listed presence of caries sicca in 49 of 281 individuals with syphilis, but zero with radial scars. One wonders where he came up with his step 5, when he had no examples? That table suggests that no individuals in his study actually had the radial scars that [3] used to identify caries sicca! The figures in his article in which he asserts radial scars in his article illustrate nodular confluence, but not the stellate lesion referred to by [3]. [7] claimed that the endocranial periosteal reaction around a linear defect fit Virchow’s classic description. It not only fails to do so but affects the opposite skull surface (endocranial in place of ectocranial) alteration described by Virchow. [7] study was a cross-sectional analysis performed on skulls from individuals at a time when syphilis was extremely prevalent. He seemed to attribute any cranial pathology present to that disease. Any disorder with significant population penetration would find itself co-occurring and its presence even at times correlating with other diseases, despite not actually being related [8,9]. Thus, he not only failed to provide evidence proving that his “stages” were part of the same disease process as that which caused caries sicca, but also failed to disprove potential attribution to other diseases. Hackett’s speculations should be recognized as such. Recognizing that his 1976 speculation on variable skeletal distribution of periosteal reaction among the different treponematoses did not withstand scrutiny [10,1] perhaps one should be circumspect in uncritically applying his other speculations? [7] was not the only individual to suggest alternative cranial findings (e.g., Hackett’s “stages”) as potentially diagnostic for syphilis. [5] reported skulls with several eroded areas, noting inner and outer table affected with irregular circular areas of decreased density, variable in size, having a porous and worm-eaten appearance. “Small lesions may coalesce to produce larger areas and occasionally a larger serpiginous defect may be seen. This picture is distinctly different from that seen in gummatous osteomyelitis, where… there is usually evidence of bone proliferation giving rise to exostoses and periosteal thickening” [5]. The latter was an intriguing statement, as gummatous osteomyelitis was a recognized complication of syphilis [11,12]. While they separated gummatous osteomyelitis from other alterations, [5] assumed that all lesions were related to syphilis and still noted that their findings were indistinguishable from those of non-treponemal osteomyelitis.
Testing the “stages” hypothesis
If caries sicca were accepted as a diagnostic finding for treponematosis, what was the actual evidence that any of the attributed “stages” have similar specificity, rather than simply representing pyogenic or granulomatous scalp infection [13,14] which has spread to the ectocranium, or even from processes (e.g., scalping) which expose the cranium to the environment (e.g., denudation)? A major challenge with cross-sectional studies was that one seldom has the opportunity to observe one “stage” to morph into the next. Thus, “stages” represented an artificial speculative construct. This can be overcome by documentation of existence of all or most stages (its spectrum) in a given sample [10]. [7] was not able to provide any such evidence. Observation of only other stages (but not actually presence of exemplary caries sicca, fulfilling Virchow’s specific criteria) in a sample/population raised the possibility that the so-called stages actually might acutally represent a different phenomenon, not attributable to the same process and therefore without the same diagnostic implication/ confidence.
Longitudinal studies would be one approach to provision of evidence that the “stages” were actually related and that [7] sequential hypothesis had merit. Although direct visualization of skulls did not permit that assessment, that changed shortly after 1906 [15]. It was intriguing that there have been no publications subsequent to facile availability of radiology (x-ray techniques) that document transition between [7] “stages.” Recognition of a disease with significant population penetrance (e.g., treponemal) was probably best achieved by assuring [10]:
a. That the pertinent finding(s) represented part of the spectrum, and that the afflicted individual was not just an outlier of another disease, and
b. That other components of the spectrum were also present in the population of interest.
It was suggested that only those findings that adhere to their initial definitions were pathognomonic. The original criteria were iterated, the validity of their application assessed, and new populations examined to determine if skull phenomena (other than that fulfilling the original criteria/definition for/of caries sicca) actually represented part of the spectrum of syphilis or if they were simply outlying examples of another disease.
Methods
The external surface of the frontal, parietal, temporal, occipital and sphenoid bones of individuals with diagnosed (in life) syphilis in the Hamann-Todd (HT) skeletal collection were systematically examined for surface defects. The Hamann-Todd human collection consisted of skeletons acquired between 1914 and 1935 in Cleveland, Ohio [16]. Autopsy and death records were curated for this lower economic status population. The Hamann-Todd human skeletal collection includes 135 individuals diagnosed in life with syphilis. Additionally studied were skulls from both Narrenturm collections [17]. The Narrenturm or Fool’s Tower in Vienna was the first psychiatric hospital worldwide and the source of the original skull collection. It was built in 1784 by Issidore Canevale on commission by Emperor Joseph II [17] adjacent to the old Vienna General Hospital and functioning through the 1790’s. The Pathologisch-anatomisches Bundesmuseu (Wien), founded by Emperor Francis II in 1796 was its successor and the source of skeletal elements exemplifying disease of interest at that time. The collections of the Royal College of Surgeons in London were also surveyed for cranial alterations analogous to those attributed to syphilis. Fisher exact test statistics, selected on the basis of fulfillment of statistical premises not met by the Chi square test [18], were utilized to assess relationship of cases of [3] defined caries sicca and those identified as “more advanced” [7].
Theory/Calculation
It was suggested that only those findings that adhere to their initial definitions were pathognomonic. The original criteria were iterated, the validity of their application assessed, and new populations examined to determine if skull phenomena (other than that fulfilling the original criteria/definition for/of caries sicca) actually represented part of the spectrum of syphilis or if they were simply outlying examples of another disease.
Results
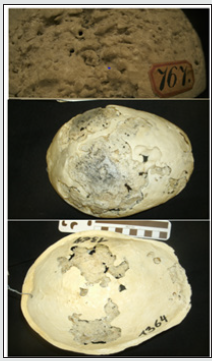
The Hamann-Todd human skeletal collection included 135 individuals diagnosed in life with syphilis. Radial scars of caries sicca were observed on the crania of 36 individuals, 28 of whom also have peripheral skeletal periosteal reaction. Five were diagnosed with paralysis of the insane, three with neurosyphilis and two with cardiovascular syphilis. There were no examples of clustered or confluent pits, focal superficial or circumvallate cavitation. Epidemiologic co-occurrence of Virchow’s caries sicca and “more advanced cases” was not demonstrated (Fisher exact test, p < 0.00001.). There was no evidence of stages of caries sicca that did not fulfill Virchow’s 1858 criteria in the 200-skull component of the Narrenturm collection derived from the psychiatric hospital. Examination of the separate Pathologisch-anatomisches Bundesmuseu anatomical pathology collection revealed no examples of caries sicca (as defined by Virchow) but did include eight crania with extensive destructive pathology attributed to syphilis and yaws. There were two forms, nodular and lytic (Figure 1). The nodular form seemed indistinguishable from that in a skull with Paget’s disease of bone and one with leontiasis (and massive osteochondromas) located in the Royal College of Surgeons in London. Massive defects in the Narrenturm skulls afflicted with the lytic variety had thinned, beveled lesion edges with prominent necrotic centers. Endocranial surfaces were equally affected as ectocranial. There were no examples of Virchow-defined caries sicca. The psychiatric hospital and anatomical pathology collection samples were highly disparate (Fisher exact test, p < 0.00001).
Discussion
Hypothesis testing
The speculation (that skull findings that did not fulfill the exemplary criteria for caries sicca actually represent a “stage” and therefore that they had similar diagnostic significance) should be testable. There seem to be three major ways that speculation can be tested:
a. Epidemiologically- diseases such as syphilis do not occur in isolation [19,20,10]. They and their manifestations present as a spectrum [21,22,10]. Some mild, some severe and of lessor or greater extent. Said spectrum should be represented in a single sample.
b. Documentation in clinically diagnosed individuals- Were diagnoses even valid in cases suggested as “stages” of syphilis? c. Given the significant population prevalence of syphilis, it is likely that was not the only disease with which individuals were afflicted.
d. Resolution of disease by medical intervention to which other disorders were not responsive.
Epidemiology
Documentation of co-occurrence of caries sicca and “stages” as a spectrum in the same sample
Examination of the skulls of individuals diagnosed in life with syphilis was anticipated to illustrate the spectrum of alterations that might be attributed to the disease [10]. One of the clinical manifestations in the most advanced cases of syphilis was “paralysis of the insane.” This, in past times, resulted in their incarceration in insane institutions and appears to have been the major source of the Narrenturm clientele [17]. However, there is no evidence of the so-called syphilitic stages in skulls from that hospital. Presence of both caries sicca as defined by [3] and the multiple “stages” stages defined by [7] has yet to be confirmed in the same single population/sample.
Was there actual evidence to attribute cranial lesions to syphilis?
[6] described eight calvaria from John Hunter’s 1768-1793 collection at the Royal College of Surgeons of England that he attributed to syphilis. None had caries sicca. The most severely affected skull (HS50a1) had a 102 mm defect with ragged edges and ectocranial thinning. Ragged edges suggested taphonomic damage or a different pathophysiology, rather than syphilis. An additional images skull (S50a.2) had multiple ectocranial defects, without obvious reactive bone or sicca-type changes. [1] further stated that “the question … is whether the process is purely syphilitic or whether there was a superimposed purulent osteomyelitis, causing further destruction of bone. The full aetiology of the cranial condition is open to some doubt.” This is analogous to Ortner’s reminder that dogs can have both ticks and fleas. Given the inverse relationship between presence of Virchow’s caries sicca and these lesions, an actual role for syphilis was not actually established here. The uncertainties of diagnosis in that time period and the unusual character of the lesions precluded their confident attribution as a direct manifestation of syphilis. The question of diagnosis validity was illustrated in Figure 1 from the Pathologisch-anatomisches Bundesmuseu. The image on the right is of the endocranium, not the ectocranium. The former is not known to be primarily affected in syphilis. [23] specifically noted that “the destructive changes…
have never been considered as manifestation of… syphilis… but “lack resemblance to any known disease (except tuberculosis).” Thus, there was no unequivocal diagnostic evidence for the Royal College of Surgeons’ cases. So, [7] hypothesis was not validated. Exemplary of the challenge was the report by [24] of an individual in the University of Coimbra medical collection whose lytic lesions they attributed to syphilis [25]. They note that hypertrophic cirrhosis, not syphilis was listed as cause of death. While they suggested syphilitic hepatitis, hypertrophic cirrhosis listed as cause of death was more likely related to hemochromatosis or sarcoidosis [not included in their consideration of diagnostic alternatives (differential diagnosis), both diseases notoriously overlooked [26,27] and lytic lesions are highly characteristic of sarcoidosis [28,29,25].
Were diagnoses even valid in cases suggested as “stages” of syphilis?
Syphilis was known as the great imitator, similar to tuberculosis and systemic lupus erythematosus (SLE) today [30,31], with the result that diagnoses were speculative, rather than definitive. The availability of laboratory tests in 1906 [15] provided a potential mechanism for potential confirmation of clinical diagnoses. However, it was belatedly recognized that those tests lacked diagnostic specificity [32]. The laboratory tests for syphilis were divided into treponemal (specific) and non-treponemal, the former only more recently available and the latter, representing the screening test available at the time of anatomical specimen acquisition. The Wassermann or venereal disease research laboratory (VDRL) test was predicated upon reaction of patient blood to the diphosphatidylglycerol referred to as cardiolipin [33]. Unfortunately, that test was non-specific, had many false positives, related to diseases that clinically mimic syphilis. These included SLE, viral infections, vaccination, tuberculosis, leprosy, brucellosis, tropical ulcer, endocarditis, cancer, vitamin deficiencies (e.g., pellagra and beri-beri) and even diabetes [33- 36,15]. Many represent entities which were known to directly or indirectly produce the same damage as that in Hackett’s “stages” [37]. Additionally, laboratory tests do not conclusively refute the diagnosis. [38] reported osteitis in an individual in whom the Wasserman test for syphilis, noting that the test was negative in 12% of individuals with what was perceived as osseous syphilis. The prevalence of false positive and false negatives precludes its use as an epidemiologic tool. A further consideration was whether the diagnoses in the individuals with the “stage” phenomenon were clinically diagnoses in life or whether the diagnoses was made retrospectively on the basis of skull alterations. Such would represent circular reasoning.
Was presence of syphilis in an individual from a highly infected population even pertinent?
Even if syphilis serology had validly identified affliction with syphilis, the extensive population penetrance of the disease precludes attribution of cranial damage, rather than simple cooccurrence. Again, it seems appropriate to invoke Ortner’s reminder that dogs can have both ticks and fleas.
Response to treatment
[39] and [19] attributed acute gummatous osteomyelitis to transfusion syphilis, noting that osteolytic skull lesions healed completely under anti-syphilitic therapy. [5] assumed that lesions were related to syphilis, but noted that their findings were indistinguishable from non-treponemal osteomyelitis. A large apparently lytic occipital area in one individual filled in with normal appearing bone within 6 months of penicillin treatment. The response of radiologically detected osteolytic lesions to therapy raises the possibility that the offending microbiologic organism was not Treponema pallidum and that the lesions, rather than superinfection, might have been unrelated to syphilis. After all, both bismuth and arsenic compounds have broad-spectrum efficacy against a wide variety of bacteria [40-42].
Differential diagnostic considerations for the cranial lesions Hackett referred to as stages
Differential diagnosis included pyogenic and granulomatous (e.g., tubercular) osteomyelitis, eosinophilic granuloma and sarcoidosis. Osteomyelitis produced multiple osteolytic foci typically with ill-defined margins in the absence of abscess formation, saucerization, and periosteal reaction and osteocartilaginous necrosis (43-44, 26,10). It was often a complication of traumatic head trauma producing scalp avulsion or hematoma [26]. [26] reported that “Primary tuberculous osteomyelitis is a common cause of cranial osteomyelitis in many regions of the world,” as did [45]. The histology of tubercular erosions was characterized by caseating granulomas, circumscribed lytic, diffuse lytic and circumscribed sclerotic lesions [46-51]. There was a Burkholderia pseudomallei-derived entity referred to as melioidosis, which mimiced the radiologic findings of tuberculosis as delineated above [52] and therefore would be in the differential. Sarcoidosis was characterized by non-caseating granulomas [28]. The osseous lesions were indistinguishable [53-55] from what has been claimed for syphilis. First described by Kreibich in 1904, sarcoidosis involved bone in 3-13% of affected individuals. The prevalence of skull involvement [56-62, 29] was similar to the prevalence of the exaggerated lesions attributed to syphilis, but indistinguishable [63]. Tierstein et al. (1961) reported 2 cm frontal swellings with well demarcated ovoid areas of bone destruction, but with ragged margins in sarcoidosis. Eosinophilic granuloma (a form of Langerhans histiocytosis) produced well-defined, eccentrically shaped lytic bone defects [64-66,44]. The coalescence of multiple lesions created the classic ‘‘geographic’’ appearance) [64,66-71]. An apparently unique feature was effaced trabeculae, associated with wrinkled bases [66].
Conclusion
Classic caries sicca, as defined by [3], and the other skull pathologies attributed to syphilis [7] appeared to represent disparate phenomena. Epidemiologic co-occurrence of Virchow’s caries sicca and “more advanced cases” was not demonstrated (Fisher exact test, p<0.00001). Were those cases indicative of syphilis? If such cases, which at best could be considered outliers, are the only ones identified, epidemiologically, the diagnosis is not confirmed. There is often an unconscious adjustment of findings to that for which one is searching (e.g., syphilis). Attribution to syphilis of findings at variance with [3] definition of caries sicca may be valid. But, isn’t it interesting that they seemingly are not found in the same sample? Isn’t it interesting that sequential radiographs documented resolution of skull lesions but that there were none documenting progression between stages? Perhaps clarity, as to the origin and geographic distribution of syphilis through time, will result from extirpation of studies which fail to use as originally vetted.
Acknowledgements
a) Appreciation is expressed to Eduard Winter, Anatole Patzalc, Lyman Jellema and the Royal College of Surgeons for collection access and insights shared.
b) This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of interest:
None.
References
- M Fiedler, V Nikiforov (2010) Spectral radius and Hamiltonicity of graphs. Linear Algebra and its Applications 432(9): 2170-2173.
- Bo Zhou (2010) Signless Laplacian spectral radius and Hamiltonicity. Linear Algebra and its Applications 432(2-3): 566-570.
- Mei Lu, Huiqing Liu, Feng Tian (2012) Spectral Radius and Hamiltonion graphs. Linear Algebra and its Applications 437(7): 1670-1674.
- Guidong Yu, Yizheng Fan (2013) Spectral conditions for a graph to be Hamilton-connected. Applied Mechanics and Materials 336-338: 2329-2334.
- Guidong Yu, Miaolin Ye, Gaixiang Cai, Jinde Cao (2014) Signless Laplacian Spectral Conditions for Hamiltonicity of Graphs. Journal of Applied Mathematics 2014(15): 1-6.
- Ruifang Liu, Wai Chee Shiu, Jie Xue (2015) Sufficient spectral conditions on Hamiltonian and trace- able graphs. Linear Algebra and its Applications 467: 254-266.
- Rao Li (2014) Laplacian spectral radius and some Hamiltonian properties of graphs. Applied Math- ematics E-Notes 14(2014): 216-220.
- Bo Ning, Binlong Li (2015) Spectral radius and traceability of connected claw-free graphs. Mathe- matics 2015(2): 1-8.
- Binlong Li, Bo Ning (2015) Spectral conditions for Hamiltonicity of claw-free graphs. arXiv 1504: 4195.
- Guidong Yu, Rao Li, Baohua Xing (2015) Spectral Invariants and Some Stable Properties of a Graph. Ars Combinatoria 121: 33-46.
- Lihua Feng, Weijun Liu, Minmin Liu, Pengli Zhang (2017) Spectral conditions for graphs to be k- Hamiltonian or k-path-coverable. Discussiones Mathematicae Graph Theory 40(1): 1-15.
- Guidong Yu, Tao Yu, Xiangwei Xia, Huan Xu (2021) Spectral Sufficient Conditions on Pancyclic Graphs. Complexity 2021: 1-8.
- Binlong Li, Bo Ning (2016) Spectral analogues of Erd˝os’ and Moon-Moser’s theorems on Hamilton cycles. Linear and Multilinear Algebra 64(11): 1-18.
- V Nikiforov (2016) Spectral radius and Hamiltonicity of graphs with large minimum degree. Czechoslovak Mathematical Journal 66(3): 925-940.
- Jun Ge, Bo Ning (2016) Spectral radius and Hamiltonicity of graphs with large minimum degree, arXiv: 1606. 08530.
- Yawen Li, Yao Liu, Xing Peng (2018) Signless Laplacian spectral radius and Hamiltonicity of graphs with large minimum degree. Linear and Multilinear Algebra 66(10): 2011-2023.
- Mingzhu Chen, Xiaodong Zhang (2018) The number of edges, spectral radius and Hamilton- connectedness of graphs. Journal of Combinatorial Optimization 35(4): 1104-1127.
- Qiannan Zhou, Ligong Wang, Yong Lu (2020) Signless Laplacian spectral conditions for Hamilton- connected graphs with large minimum degree. Linear Algebra and its Applications 592: 48-64.
- Binlong Li, Bo Ning (2017) Spectral analogues of Moon-Mosers theorem on Hamilton paths in bi- partite graphs. Linear Algebra Appl 515: 180-195.
- Guisheng Jiang, Lifang Ren, Guidong Yu (2019) Sufficient Conditions for Hamiltonicity of Graphs with Respect to Wiener Index, Hyper-Wiener Index, and Harary Index. Journal of Chemistry 2019: 1-9.
- Guidong Yu, Yi Fang, Yizheng Fan, Gaixiang Cai (2019) Spectral radius and Hamiltonicity of graphs. Discussiones Mathematicae Graph Theory 39(2019): 951-974.
- Lihua Feng, Pengli Zhang, Henry Liu, Weijun Liu, Minmin Liu, Yuqin Hu, et al (2017) Spectral conditions for some graphical properties. Linear Algebra and its Applications 524(1): 182-198.
- Guidong Yu, Yi Xu, Guisheng Jiang (2019) Energy and the Zagreb index conditions for nearly balanced bipartite graphs to be traceable. Journal of combinatorial Mathematics and Combi-natorial Computing 110: 109-123.
- Rao Li (2012) Egienvalues, Laplacian eigenvalues and some Hamiltonian properties of graphs, Utilitas Mathematica 88: 247-257.
- Rao Li (2014) Spectral conditions for some stable properties of graphs, Journal of Combinatorial Mathematics and Combinatorial Computing 88: 199-205.
- Qiannan Zhou, Ligong Wang (2016) Distance signless Laplacian spectral radius and Hamiltonian properties of graphs. Linear Multilinear Algebra 65(11): 2316-2323.
- Rao Li (2009) Energy and Some Hamiltonian Properties of Graphs, Applied Mathematical Sciences 3(56): 2775-2780.
- Guidong Yu, Gaixiang Cai, Mioalin Ye, Jinde Cao (2014) Energy conditions for Hamiltonicity of graphs. Discrete Dynamics in Nature and Society 2014: 1-6.
- M Krivelevich, B. Sudakov (2003) Sparse pseudo-random graphs are Hamiltonian. Journal of Graph Theory 42(2003): 17-33.
- S Butler, F Chung (2010) Small spectral gap in the combinatorial Laplacian implies Hamiltonian. Annals of Combinatorics 13: 403-412.
- Yizheng Fan, Guidong Yu (2012) Spectral condition for a graph to be Hamiltonian with respect to Normalized Laplacian.
- Weijun Liu, Minmin Liu, Lihua Feng (2017) Spectral conditions for graphs to β-deficient involving minimum degree. Linear Multilinear Algebra 66(4): 1-11.
- Guidong Yu, Yi Fang, Yi Xu (2017) Spectral condition of complement for some graphical properties. Journal of combinatorial Mathematics and Combinatorial Computing 108 (2019): 65C74.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...