
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Research Article(ISSN: 2641-1725) 
Barriers to the Pap Smear in Women of Fertile Age Volume 2 - Issue 1
Gloria Maricela Guerra Rodríguez1*, Octavio Augusto Olivares Ornelas2, Héctor Manuel Gil Vázquez1, Erika Berenice Rodríguez Martínez3 and Manuel Alejandro Sanchez Bernal4
- 1Professor, Academic Unit Multidisciplinary Matamoros, Autonomous University of Tamaulipas, Mexico
- 2Professor, Obstetrician and Midwife Surgeon, Autonomous University of Tamaulipas, Mexico
- 3Bachelor in Nursing, Autonomous University of Tamaulipas, Mexico
- 4Graduate, Autonomous University of Tamaulipas, Mexico
Received: October 03, 2018; Published: October 11, 2018
*Corresponding author: Gloria Maricela Guerra Rodríguez, Autonomous University of Tamaulipas. Academic Unit Multidisciplinary Matamoros UAT, México
DOI: 10.32474/LOJMS.2018.02.000129
Abstract
In Mexico, it is recommended for the female population in active sexual age to perform the Papanicolau (PAP) smear each year Minister of Health [1] as an strategy for the timely detection of cervical cancer (CC), however, there are multiple reasons that can explain the low adherence to control via PAP smear, some of them, a deficient education, cultural and religious influences, wrong information, access and quality to health services Gajardo and Urrutia [2].
Objective: Identify the barriers for the collection of the PAP smear in a group of women in fertile age.
Material and Methods: The design was descriptive, transversal Polit and Hungler [3] in a population of women in fertile age in the city of Matamoros, Tamaulipas, Mexico; the sampling was by convenience, with a final sample of 150 women, using the CPC-28 Urrutia [4] instrument.
Results: The profile of the women match an average age of 35 years, married, in a stable sexual relationship, with a middle school academic level. Indexes are reported with averages oscillating between 2.48 (SD=1.41) and 2.55 (SD=1.40) where it is mentioned that PAP is not performed due to fear of comments about having cancer, due to shame to being examined in the genitals and due to a lack of time to perform the PAP.
Conclusions: Although the continuous promotion for the timely detection of cancer, we can observe that the same barriers for the collection of PAP remains in multiple studies in Latin America, where the lack of information, beliefs and modesty as the prevails as the main factors of women behavior against prevention.
Keywords: Papanicolau (PAP); Cervical Cancer (CC); Human Papiloma Virus (HPV); Barriers
Abbreviations: PAP: Papanicolau CC: Cervical Cancer; HPV: Human Papilloma Virus
Introduction
The cervical cancer (CC) is one of the main threats against women life; it is estimated that right now in the world, this disease affects over one million women and most of them have neither been diagnosed or have access to a treatment that could save them or extend their life. In 2012, the World Health Organization (WHO) reported that it was diagnosed 528 000 new occurrences, and 266 000 women died of this disease, over 90% of them happened in countries with medium to low income. It is predicted, without immediate attention, the deaths caused by CC could raise by 25% in the next ten years; this same data is reported by the Pan American Health Organization (PAHO) (WHO/PAHO [5] as mortality indexes due to CC.
The CC is closely related with the presence of the Human Papiloma Virus (HPV) mainly those identified as high risk; the two that cause with higher frequency are types 16 and 18, which together, are responsible for an approximate of 70% of CC cases around the world PAHO [6]. In the female population, CC is the main death cause by malignant neoplasm, especially in the range of 25 to 64 years old, this according to the Mexican Official Norm (NOM- 014SSA2-1994).
In Mexico it is recommended that all the female population with active sexual life should perform the Papanicolau (PAP) each year, each three years for those who have had a negative result to infection by HPV in the last two PAP, dysplasias or cancer; women infected by VPH, dysplasia or cancer should be traced by a dysplasia clinic and, when they are released by the hospital, they should begin again with PAP with an annual frequency; those who have positive PAP results due to non-specific inflammatory processes or additional findings should receive medical treatment and continue with annual PAP until there are two straight negative results, according with the Mexican Official Norm NOM-014-SSA2-1998 for prevention, detection, diagnosis, treatment, control and epidemiological surveillance of CC Minister of Health [1]. There is a low prevalence of the usage of this test and the found factors related with its limited use are the modesty, lack of information about the usefulness of the test or lack of approval by the partner Sagarduy [7].
This topical has generated multiple controversies by the stretch relationship it has with the different cultures that the human being has; including that, nowadays women have the false believe that if they do not have a background of developing the CaCU disease, they do not have the necessity of performing PAP. Some barriers to not entering a periodical screening is to not know the age in which the test must be performed and with which frequency it should be done, they also mention that they do not come to their control due to fear of being diagnosed with cancer, also as shame to be examined in the genitals, and never had any children. Other beliefs are that they should have an active sexual life, being that CaCU is a serious health problem and it can take them to perform a chemotherapy, a hysterectomy or even death, and because of this, if she has 21 years old, the woman can perform the cytological exam.
The main action that drives women to come and perform an PAP is by the indication of a medical doctor or a nurse, because they heard it on television or radio, and because family members mentioned the topic in relationship with received benefits, being the most important health care Urrutia [8]; however, the majority of women have the belief that they will be hurt in the moment of performing the PAP, or that they will experiment pain during the exploration; this can have a reason in a lack of appropriate information by the medical staff about the realization of the test; they also refer this fear or shame to being male the one who is going to perform the test and that young women who live with their parents have fear of being revealed that they have an active sexual life. Other of the mentioned barriers mentioned by women are that they do not come to perform the test due to the lack of time or the long await to receive the result of the test, or the lack of consent by the couple, which is very common in the Mexican population by the still perceived machismo.
Material and Methods
The design of this study was descriptive, transversal in a population conformed by women in fertile age in the independence health center in the city of H. Matamoros, Tamaulipas, Mexico. The sampling was by convenience, it included all women who manifested the intention and availability to participate in the study, obtaining a final sample of 150 woman. To collect personal identification data, it was used the personal identification card (PIC) which included information related with age, level of education, civil status, type of relationship with the couple and previous results of papanicolau. The variable beliefs about PAP and CC was measured with an instrument developed and validated with Chilean population based in the health beliefs model descripted by Rosenstock [9]. To answer the objective, it was applied an instrument developed and validated based in the health beliefs model descripted by Rosenstock [9] which presents 6 dimensions divided in: 1. Barriers, which contains 9 items. 2. Benefits, which contains 3 items. 3. Severity, which contains 4 items. 4. Susceptibility, which contains 3 items. 5. Signals of action, which contains 6 items and 6. Requirements, which contains 3 items.
For this research, it was only used the dimension of barriers, composed by 9 items and which is subdivided into three dimensions: fear to find having cervical cancer, waiting time to being attended and shame to be observed in the genitals, which an answer range type Likert of 5 points which ranges from completely agree to completely disagree, Items 2,3,4,5,9 are about time and schedules that the patients have to perform the Pap, item 1 is about the lack of knowledge that the patients have with respect to the age where they should begin the monitoring and performing of the Pap, item 6 is about the fear the patients can have by the news of having cervical cancer. Item 7 is about shame that women can have to have somebody inspecting their genitals, since it is a very intimate body part, and item 8 is about the bad treatment that the patients can have by the medical staff working in the health center where the women come. For the capture and data analysis, it was used the statistical package SPSS (Statistical Package for the Social Science) version 20, where a descriptive statistic was used. The results presented are liability of 96 through the Alpha of Cronbach.
Results and Discussion
The socio-demographic profile presented by the women participating in the study corresponds to an average age of 34.7 years (SD=7.01), in relationship with the level of education, 43.3% reported middle school level and a low percentage (10%) reported being currently studying at a university. The bigger proportion reported a marital status of being married with an 57.3% and the 89.3% of the participants reported having a stable sexual partner, and in the PAP results, the PAP class II (normal) with a 96.0 (Table 1) prevailed. These results coincide with multiple studies where the average age is 35 years old and women are in a stable sexual relationship Urrutia [4], Sagarduy [7].
Table 1: Barriers for PAP smear.
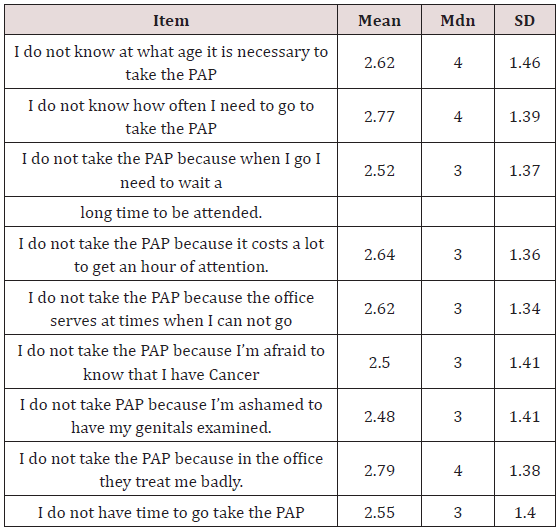
Note: n=150 woman. Beliefs in health. Mdn= Median; SD= Standar Desviation, Measurement range 1-4 (4 = strongly disagree, 3 = disagree, 2 = agree, 1 = strongly agree).
Results are presented in relationship with the study variables where it can be observer that women do not know in which age is necessary to perform the PAP and with which frequency it is necessary to come to perform the test with averages ranging from 2.62 (SD=1.64) to 2.77 (SD=1.39); results that differ from the study performed by Huamani [10] where it was reported that participants from its study presented a high knowledge, where 64.8% knew about how it is performed the PAP and 65.2% knew the optimal frequency to perform the PAP, highlighting that in a 38.5% the level of studies was university, where we can observe that a lower education level and an inadequate history of PAP are associated with poor knowledge and a negative attitude towards the performance of Papanicolau Huamani [10]. In relationship with the barriers to the practice of the papanicolaou, women agree that they do not take the PAP because when they attend, it takes a large amount of time to be attended by medical staff and they do not have that time, results with averages ranging from 2.52 (SD=1.37) and 2.55 (SD=1.40) (Table 1). Similar results are reported by Polo-Peña [11] where in its study, it was mentioned that the time availability was a main cultural factor, which constructs barriers to the realization of cytology in the 95% of its participants.
Another important factor are those related with fatalists thoughts and machismo that might be present as barriers to perform this test in a periodical manner, in the present study, the women that do not take PAP due to fear to a cancer diagnostic and being ashamed to have their genitals being examined are averages ranging from 2.50 (SD=1.41) to 2.48 (SD=1.41) (Table 1); these results match with previously analyzed literature where multiple authors report that shame, fear and lack of time are barriers against the perform of Papanicolau, as it is also the lack of information about age to take the exam Urrutia [4] Sagarduy [7] Mosavel [12- 14].
Conclusion
In relationship with the obtained results, it can be concluded that there still exists false beliefs about PAP and CC, where the most relevant ones are that the population does not know in which age it is necessary to take PAP [13] it also does not know the frequency in which it should be taken, they do not take the PAP due to a long time to being attended in the medical center and do not have that time to take the test, fear of knowing to have cancer and shame to be examined in the genitals. It is very important data to consider by the professionals in the preventive health field, where providing brief information is not enough to achieve woman empowerment and adhere to perform the Papanicolau test.
References
- Secretary of Health (2013) National Health Program 2001-2006. Mexico DF. Health Secretary.
- Gajardo M, Urrutia M T (2017) Beliefs about cervical cancer and Papanicolaou and its relationship with adherence to screening. Chilean Journal of Obstetrics and Gynecology 82(6): 706-712.
- Polit DF, Hungler BP (2000) Sampling designs. scientific research in health sciences 6th (Edn); Mexico: McGraw-Hill Interamericana pp. 285- 289.
- Urrutia MT, Hall R (2013) Beliefs about cervical cancer and Pap test: a new Chilean questionnaire. Journal of Nursing Scholarship 45(2): 126- 131.
- WHO / PAHO, World Health Organization / Pan American Health Organization (2016).
- Pan American Health Organization [PAHO] (2013) Comprehensive prevention and control of cervical cancer: a healthier future for girls and women, Retrieved on September 23.
- Sagarduy JLY, Salinas BEP, Reyes D R (2012) Conocimiento y creencias sobre la prueba de Papanicolaou en estudiantes universitarios. Psicología y Salud 22(2): 185-194.
- Urrutia MT (2012) Creencias sobre Papanicolaou y cáncer cérvicouterino en un grupo de mujeres chilenas. Revista chilena de obstetricia y ginecología 77(1): 3-10.
- Rosenstock I M (1974) Historical origins of the health belief model. Health education monographs 2(4): 328-335.
- Huamaní C, Hurtado-Ortega A, Guardia-Ricra M, Roca-Mendoza J (2008) Conocimientos y actitudes sobre la toma de papanicolaou en mujeres de Lima, Perú 2007. Revista Peruana de Medicina Experimental y Salud Pública 25(1): 44-50.
- Polo-Peña EY, Torres-Pérez SP, Ochoa-Acosta R, Villarreal-Amarís G (2014) Factores personales relacionados con la realización de citología vaginal sincelejo 2013 - 2014. RevisaludUnisucre 2(1): 31-41.
- Mosavel M (2011) Health promotion and cervical cancer in South Africa: why adolescent daughters can teach their mothers about early detection. Health promotion international 27(2): 157-166.
- Urrutia MT (2009) Development and testing of a questionnaire: beliefs about cervical cancer and Pap test in Chilean women. Tesis doctoral presentada a la Universidad de Miami (USA) como uno de los requisitos para obtener el grado de PhD.
- Comprehensive control of cervical cancer. Guide essential practices. 2nd (Edn); Washington DC: OPS.1-204.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...













