
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Review Article(ISSN: 2641-1687) 
The TUR Syndrome Re-Incarnating as ARDS after Saline use as Irrigating Fluid in Endoscopic Surgery Volume 3 - Issue 2
Ahmed NM Ghanem*
- Faculty of Medicine, NHS and Mansoura University, Egypt
Received: October 23, 2021; Published: November 09, 2021
Corresponding author: Ahmed NM Ghanem, Faculty of Medicine, NHS and Mansoura University, Egypt
DOI: 10.32474/JUNS.2021.03.000159
Abstract
Objective: To demonstrate the TUR syndrome characterized with hyponatraemia (HN) will no longer be seen after using saline
as irrigating fluid in urology, but it has re-incarnated as the acute respiratory distress syndrome (ARDS) presenting with the same
clinical picture of the multiple organ dysfunction syndrome (MODS).
Material and Methods: A focused objective and relevant narrative review of other eminent authors’ work and mine are used
here.
Results: The TUR syndrome characterized with HN will no longer occur in urology after the use of saline as irrigating fluid
in endoscopic surgery. It has reincarnated as ARDS presenting with the same MODS clinical picture. It is induced by VO caused
by iv fluid infusions. This induces cardiovascular shock (VOS) that cause ARDS. The latter is already common in clinical practice
due to the excessive us of iv fluids in the management of shock, acutely ill patients, and prolonged major surgery as iatrogenic
complication of fluid therapy. The wrong Starling’s law dictates the current faulty rules on fluid management of shock that mislead
physicians into giving too much fluid. The correct replacement is the hydrodynamics of the porous orifice (G) tube which should be
the new scientific basis for fluid therapy in shock management. The currently available hypertonic sodium therapy of 5%NaCl and/
or 8.4%NaCo3 is lifesaving therapy for HN, the TUR syndrome and ARDS.
Conclusion: The TUR syndrome may seem to have been eradicated in urology with the use of saline as irrigating fluid in
endoscopic surgery. However, it has reincarnated as ARDS with the same clinical picture of MODS. It is an iatrogenic complication of
fluid therapy dictated by the wrong Starling’s law for which the hydrodynamic of the G tube is the correct replacement that should
be the new scientific basis for a new policy on fluid management of shock.
Keywords: The TUR syndrome; Endoscopic Surgery; ARDS; Shock; Fluid Therapy; Starling’s law, Capillary-ISF transfer
Introduction
My beginning with the transurethral resection of the prostate (TUR) syndrome started in 1981 after I attended post-mortem (PM) examinations on 3 patients who died after the TURP surgery. I was only an SHO in urology working for the late Mr. KC Perry and JP Ward at DGH in Eastbourne. At the PM examination it was clear and obvious to me that these patients died of internal drowning as result of massive volumetric overload (VO) of fluids used for resuscitation of a cardiovascular shock they suffered, and the fluid was retained in their bodies. When I asked the pathologist why doesn’t he mention that retained VO in his report? He replied: “because it offends treating physicians”? The word offends hit me right hard on my head like a hammer. My next question to myself was if it offends them why do physicians do it? This had led me to immediately replace the term fluid overload with the new and original Volumetric Overload (VO) after adding the cardiovascular hypotension Shock to it to become (VOS) that was introduced to avoid the word offends but it has proved to be a new scientific medical discovery. Another few questions such as: “What is misleading physicians into giving too much fluid during the resuscitation of shock? What shock is it? I communicated with Richard Harrison III (who may be late now) who is the originator of the hyponatraemic shock of the TUR syndrome and the use of 5%NaCl therapy in clinical practice for years during his retirement [1]. I reported later the true pioneer originators of this shock and the hypertonic sodium therapy (HST) were Danowski et al who induced it experimentally in dogs by massive 5%Glucose infusion [2]. Harrison advised me to “put the poison in the honey” that I could not accept. After the PM examination I suspected and incriminated Starling’s law being the scientific basis of fluid therapy in shock that dictates the wrong rules on fluid therapy for shock management documented in articles and books [3-7], for which the hydrodynamics of the porous orifice (G) tube is the correct replacement (Figures 1a&b) [8,9]. I felt so strongly about it that I wrote a letter to the late great professor of physiology Eric Neil and author of Sampson Wright Textbook of Physiology later in 1983 [10,11]. He nicely replied in handwritten letter as he was in retirement asking: Why and how may Starling’s law cause death of patients? The answer is there now after 40 years of hard scientific research and investigations [12].
Figure 1a: shows a diagrammatic representation of the hydrodynamic of G tube based on G tubes and chamber C. This 37-years
old diagrammatic representation of the hydrodynamic of G tube in chamber C is based on several photographs. The G tube
is the plastic tube with narrow inlet and pores in its wall built on a scale to capillary ultra-structure of pre-capillary sphincter
and wide inter cellular cleft pores, and the chamber C around it is another bigger plastic tube to form the G-C apparatus.
The chamber C represents the ISF space. The diagram represents a capillary-ISF unit that should replace Starling’s law in
every future physiology, medical and surgical textbooks, and added to chapters on hydrodynamics in physics textbooks. The
numbers should read as follows:
The inflow pressure pushes fluid through the orifice.
Creating fluid jet in the lumen of the G tube**.
The fluid jet creates negative side pressure gradient causing suction maximal over the proximal part of the G tube near the inlet
that sucks fluid into lumen.
The side pressure gradient turns positive pushing fluid out of lumen over the distal part maximally near the outlet.
Thus, the fluid around G tube inside C moves in magnetic field-like circulation (5) taking an opposite direction to lumen flow
of G tube.
The inflow pressure 1 and orifice 2 induce the negative side pressure creating the dynamic G-C circulation phenomenon that is
rapid, autonomous, and efficient in moving fluid and particles out from the G tube lumen at 4, irrigating C at 5, then sucking
it back again at 3,
Maintaining net negative energy pressure inside chamber C.
**Note the shape of the fluid jet inside the G tube (Cone shaped), having a diameter of the inlet on right hand side and the
diameter of the exit at left hand side (G tube diameter). I lost the photo on which the fluid jet was drawn, using tea leaves of
fine and coarse sizes that run in the centre of G tube leaving the outer zone near the wall of G tube clear. This may explain the
finding in real capillary of the protein-free (and erythrocyte-free) sub-endothelial zone in the Glycocalyx paradigm. It was also
noted that fine tea leaves exit the distal pores in small amount maintaining a higher concentration in the circulatory system
than that in the C chamber- akin to plasma proteins.
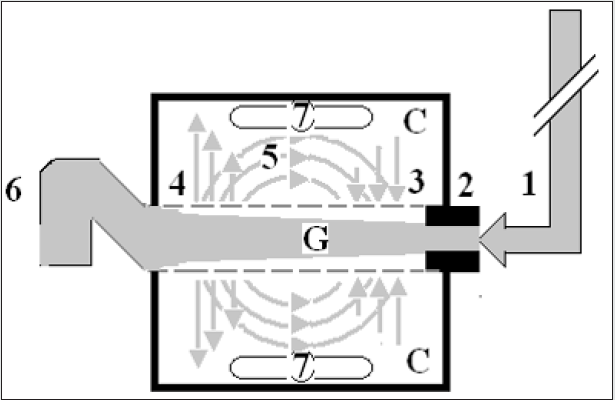
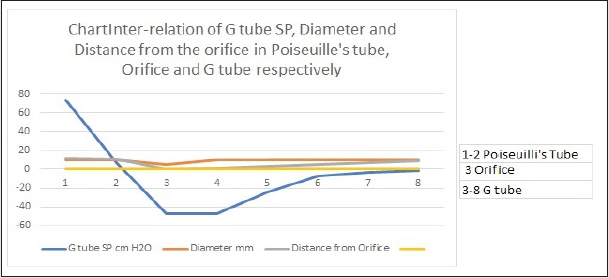
Figure 1b: shows the relationship between SP to the Diameter and length of the G tube which demonstrate a negative SP starting at the orifice (Point 2) (akin to precapillary sphincter) and extends as high negative pressure gradient over the proximal part of the G tube (Point 2-6) to cross 0 line at point 8 and then turn positive of 7 cm water at Point 9. This SP gradient from orifice at Point 2 to G tube lumen (Points 2-6) is negative to become positive DP at point 9 of 7 cm H20 water along the G tube. The wide section diameter of G tube is 7 mm all along the entire tube. The orifice is 5 mm while the distance from orifice to exit represent the tube’ length in which the Fluid jet diameter change with increasing gradient (Figure 1a). Neither Poiseuille’s law nor Bernoulli’s equation can predict SP neither at orifice of Venturi’s effect nor at the G tube proximal part know as Bernoulli’s effect. Thus, the RBCs speed or CBS depend on the dynamic fluid jet diameter not the G tube diameter. Hence the equation in Figure 2g (Figure 2) and graph are wrong giving low RBCs speed or CBS over the capillary length but is correct only at point of the G tube where the jet diameter equals the tube diameter.
What is the TUR Syndrome? And what is causing the
“Understanding Gap”?
Our prospective cohort study on the TUR syndrome was
conducted in 1987-8, a letter to the editor of BJU was reported in
1988 [13], MD Thesis was accepted November 1988 [14], and the
article reported in 1990 [15]. The TURP syndrome is a condition
induced by gaining large volume of sodium-free fluid overloading
the cardiovascular system and spelling over into the interstitial
fluid (ISF) space of vital organs and subcutaneous. The fluid of
1.5%Glycine used as irrigating fluid gets absorbed, or rather
infused through peri-prostatic veins, during the TURP surgery
as well as all endoscopic surgeries performed under sodium-free
fluid irrigation of any type such as Mannitol, Sorbitol, Glucose and
Cytal. Also, intravenous (iv) infusion of 5% Glucose considerably
and significantly contributes to it- as well as saline. What is more,
excessive infusion of saline or any sodium-based fluid such as
Saline, Hartman, Ringer, plasma, and plasma substitutes, and blood
worsens it transferring the shock being treated from VOS 1 into VOS
2 [16] and causing ARDS 1 and 2 [17,18] with apparent correction
of HN, and has high morbidity and mortality later.
The TUR syndrome has a characteristic severe drop of serum
sodium level causing acute dilutional hyponatraemia (HN) induced
by VO 1 (Figures 2 & 3) with severe clinical symptoms affecting
all vital organs causing the multiple organ dysfunction syndromes
(MODS) (Table 1) or ARDS [17,18] with recognizable clinical picture
but one system may predominate such as acute kidney injury (AKI).
The HN of <120 mmol/l has 2 paradoxes and 2 nadirs that have
eluded authorities and physicians on HN, and that has made the
TUR syndrome most elusive and invisible making it though obvious
it has remained invisible even to authorities on HN. Professors
and consultant urologists who are such swift good resection
experts have testified that the TUR syndrome does not exist as no
fluid absorption occurs, with a negative prospective study of 100
patients [19]. Off course no such hyponatraemia occurs when the
irrigating fluid is saline whatever the volume absorbed and infused.
Another important reason that prevents massive 1.5% glycine
absorption and the TUR syndrome is for the Urologist not to breach
the prostate capsule and not to open the venous sinuses where
the irrigating fluid is directly injected intravenously (iv) into the
periprostatic veins. There was also another good swift urologist
who reported >1000 consecutive TURP surgeries without seeing
the TUR syndrome. The risk of VO during endoscopic surgery
will continue to occur as long as there are registrars in training
and even with the experienced consultants who occasionally and
inadvertently breach the prostatic capsule and open the venous
sinuses. However, the TUR syndrome due to 1.5% Glycine VO
with its characteristic HN has an undoubted reality [13-15] and
[20-22]. Our study reported 10% incidence of the TUR syndrome
with one near death case that was saved [14] and a similar study
done a year earlier in the same department reported 7% incidence
of morbidity with 1% mortality [22]. Before the TUR syndrome
disappears into oblivion and is totally replaced by ARDS a most
comprehensive literature review on the subject was reported in
2018 after the wide use of saline as irrigating fluid in the TURP
surgery [23]. Here a distinction between a physiological VO of <2 L infused in less than one hour that is extensively studied by Hahn
in volunteers and patients is known as Volume Kinetic (VK) (20)
and the pathological VO of 3.5-5 L gained in < 1 h that causes the
TUR syndrome [15] is highlighted. This has been a cause of serious
misunderstanding gap in the pathogenesis of the TUR syndrome.
The physiological response of VK is remarkably different from
the pathological response of VO which is paradoxical: VK elevates
blood pressure and induces diuresis while VO causes hypotension
with bradycardia and causes acute renal failure.
Figure 2: It shows the means and standard deviations of volumetric overload in 10 symptomatic patients presenting with shock and hyponatraemia among 100 consecutive patients during a prospective study on transurethral resection of the prostate. The fluids were of Glycine absorbed (Gly abs), intravenously infused 5% Dextrose (IVI Dext) Total IVI fluids, Total Sodium-free fluid gained (Na Free Gain) and total fluid gain in litres.
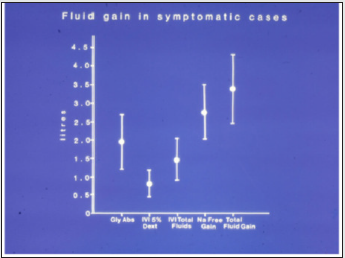
Table 1: Shows the manifestations of VOS 1 of the TURP syndrome for comparison with ARDS manifestations induced by VOS2. The manifestations are the same but one vital organ-system may predominate.
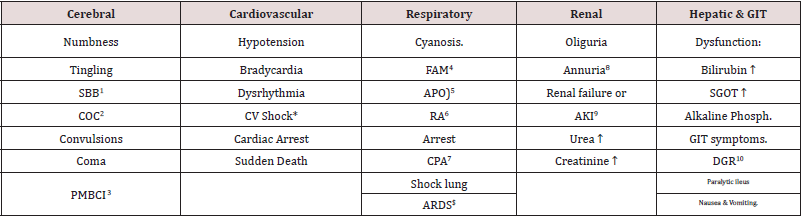
Table Abbreviation
SBB1: Sudden Bilateral Blindness
COC2: Clouding of Consciousness
MBCI3: Paralysis mimicking bizarre cerebral infarctions, but is recoverable on instant use of HST of 5%NaCl and/or NaCO3, and so
is coma and AKI
FAM4: Frothing Around the Mouth
APO5: Acute Pulmonary Oedema.
RA6: Respiratory Arrest.
CPA7: Cardiopulmonary Arrest; ARDS$: Occurs on ICU later.
Annuria8: That is unresponsive to diuretics but responds to HST of 5%Ncl and/or 8.4%NaCO3; AKI8: Acute Kidney Injury. Also
occurs the excessive bleeding at
AKI9: Acute Kidney Injury
DGR10: Delayed Gut Recovery; CV Shock*:
Excessive bleeding may occur at the surgical site and leucocytosis occurred in the absence of sepsis and septic shock.
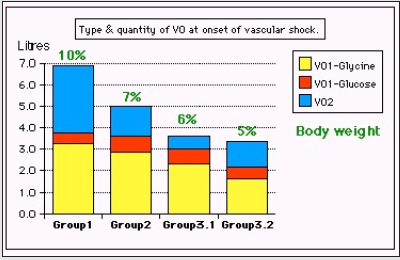
Figure 3: Shows volumetric overload (VO) quantity (in liters and as percent of body weight) and types of fluids. Group 1 was the 3 patients who died in the case series as they were misdiagnosed as one of the previously known shocks and treated with further volume expansion. Group 2 were 10 patients from the series who were correctly diagnosed as volumetric overload shock and treated with hypertonic sodium therapy (HST). Group 3 were 10 patients who were seen in the prospective study and subdivided into 2 groups; Group 3.1 of 5 patients treated with HST and Group 3.2 of 5 patients who were treated with guarded volume.
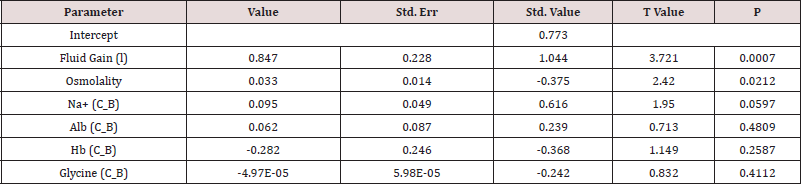
The TURP syndrome starts by presenting with cardiovascular hypotension shock to anaesthetists and surgeons in theatre [24,25] and at times by cardiac or cardiopulmonary arrest [26] and sudden death. By next morning the surviving patients present with coma, convulsion and bizarre paralysis to physicians, neurologists, and ICU specialists [15]. It has the characteristic serum hypo-osmolality. BUT other solute contents dilutions seem to be apparently spontaneously improving due to water shift into cells [Table 2, Figures 1 and 2]. The HN of <120 mmol/l causes cardiovascular hypotension shock. Volumetric overload (VO) is the most highly significant factor causing its patho-aetiology with a (p=0.0007). Osmolality was also significantly low (p=0.02) while all other serum solute changes including the most remarkable drop in serum sodium and huge elevation in serum glycine did not reach statistical significance in the multiple regression analysis, yet it did alone when pre- and post-operative levels are compared!? [Table 2 and 3]. This cardiovascular shock of VOS is easily confused with and mistaken for haemorrhagic or septicaemia shock and is wrongly treated with further massive volume expansion that usually kills the patient as happened in the 3 patients mentioned above!?
Table 2: Shows the mean summary of data, therapy and outcome comparing the 3 groups of 23 case series patients who’s (whose) VO is shown in Figure 3. Groip-1 was the 3 patients who died and had post-mortem examination, Group-2 were a series of severe TURP syndrome cases successful ly treated with hypertonic sodium therapy (HST), and Group-3 were 10 patients encountered in the prospective study who were randomized between HST (3.1) and conservative treatment (CT) (3.2). The significant changes of serum solute contents are shown in bald font with the corresponding p- value. Most of the patients showed manifestation of ARDS of which the cerebral manifestation predominated, being on initial presentation (Regional Anaesthesia) and representation of VOS 1 (General Anaesthesia). However, most patients were given large volume of saline that elevated serum sodium to near normal while clinical picture became worse. They suffered VOS2 that caused ARDS. The VO of patients to whom these data belong is shown.
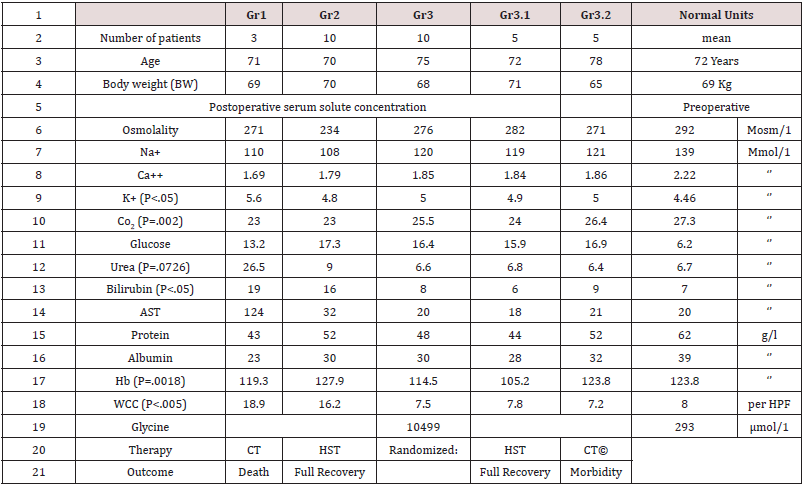
Table 3: Shows the multiple regression analysis of total per-operative fluid gain, drop in measured serum osmolality (OsmM), sodium, albumin, Hb and increase in serum glycine occurring immediately post-operatively in relation to signs of the TURP syndrome. Volumetric gain and hypo-osmolality are the only significant factors.
The toxic theory of the TUR syndrome and septic theory of ARDS.
Sepsis and septic shock in the pathogenesis of ARDS is as innocent as the wolf in Josef story [18], so is glycine in the aetiology of the TUR syndrome [15], particularly as correctly mentioned that the TUR syndrome occurs with Mannitol, Sorbitol, and Glucose. Professor Alan Arieff has clearly reported the morbidity and mortality of hyponatraemia (HN) of the TUR syndrome induced by 1.5%Glycine as well as the excessive 5%Glucose infused intravenously during prolonged surgery in healthy women [27]. That does not mean that I deny the toxicity of glycine and the seriousness of sepsis. I am just saying they are misleading like a mirage to someone thirsty and lost in the desert. While thinking about it please, try to attend the PM examination of some patients who died from the TUR syndrome and ARDS. Every anaesthetist should examine own practice when he embarks on Bolus Fluid Therapy (BFT) during anaesthetic induction and watch out how much fluid is given during prolonged major surgery. Review the scientific basis of fluid therapy in the management of septic and all other types of shock on which bases the current practice is implemented.
Fluid therapy Regimen and Iatrogenic complications
The TUR syndrome occurs because of combination of fluid absorption and direct iv infusion of the irrigating fluid when the prostatic capsule is breached, and venous sinuses are open. In clinical practice all ARDS cases occur as result of iv infusion of fluids. In our study 7 cases of capsule breaching occurred among the 10 TUR syndrome cases as observed by the surgeon. The iv infusion occurs with both the liberal regimen of Early Goal-Directed Therapy (EGDT) and Bolus fluid therapy (BFT) of the conservative regimen. Hahn is a professor and consultant of anaesthesia and intensive care. He is also a leader and world authority on fluid therapy and the editor of a book on the same subject. I would and have recommended him as the head of a committee to write the new guidelines on fluid therapy in shock management. He has my new book that will help him for >8 months now, please read it if you’ve not done so already. Like all anaesthetists, Intensive care therapists, surgeons, and physicians of the whole world who remain to practice the liberal fluid therapy regimen also well known as EGDT in the management of shock, don’t you? Go to any ICU near you and observe the swollen-up ARDS patients mostly with trunk oedema comparing their body weight on hospital admission with their current weight while suffering from ARDS. Try to attend the PM examination of the TURP patients and ARDS patients. Allow me to reproduce this section from my article later that is most recommended reading to all physicians interested in the subject of fluid therapy, the TUR syndrome, HN, VOS and ARDS [18].
The role of Starling’s law
Starling’s law [28,29] dictates the current faulty rules on fluid therapy in the management of shock. It thus misleads physicians into giving too much fluid during shock resuscitation [30]. More than 21 reasons were reported to show that Starling’s law is wrong [31], none of it can be denied or refuted. The correct replacement is the hydrodynamic of the porous orifice (G) tube [8,9] (Figure 1 a & b) that was built on capillary ultrastructure anatomy of having precapillary sphincter [32] and a porous wall [33] that allow the passage of plasma proteins-hence nullify the oncotic pressure. It follows that the extended Starling Principle is wrong and a misnomer [34,35] and all the equations are also wrong.
Two types of VO inducing VOS and causing ARDS of type 1 and 2
There are two types of VO: Type 1 induced by sodium-free fluid and Type 2 induced by sodium-based fluid. These in turn induce VOS 1 and VOS 2 which cause ARDS 1 and ARDS 2, respectively. The clinical picture is the same for both types (Table 1). Type 1 is characterized with HN of the TUR syndrome with which the cerebral neurological manifestations of coma, convulsions, and bizarre paralysis predominate while type 2 may have moderate hypoproteinemia if induced by crystalloids and none when plasma, plasma substitutes and blood are used. Type 2 may complicate Type 1 or may occur do novo. Manifestations of the multiple organ dysfunction syndrome (MODS) are the same and appear in every case, but one system may predominate. When Hahn sent me his article on Revised Starling Principle calling for revalidation [34] I immediately responded with an article: Revised Starling’s Principle (RSP): a misnomer as Starling’s law is proved wrong. I considered research on validating RSP is a total waste of money, time, and efforts.
Proof by eminent authors on the VO role in the aetiology of the TUR syndrome and ARDS
Professor Robert Hahn from Sweden has done lots of research infusing various types of fluid used in clinical practice to normal adult volunteers and patients, as well as animal research and clinical studies and reported >340 articles on the TURP syndrome alone (PubMed 2017) and 532 articles in total (PubMed search 2021): Here is what Robert Hahn said: in the abstract of an article reported in 2017 [36]:
Abstract [36]:
“Adverse effects of crystalloid fluids are related to their
preferential distribution to the interstitium of the subcutis, the gut,
and the lungs. The gastrointestinal recovery time is prolonged by 2
days when more than 2 liters is administered. Infusion of 6-7 liters
during open abdominal surgery results in poor wound healing,
pulmonary oedema, and pneumonia. There is also a risk of fatal
postoperative pulmonary oedema that might develop several days
after the surgery. Even larger amounts cause organ dysfunction by
breaking up the interstitial matrix and allowing the formation of
lacunae of fluid in the skin and central organs, such as the heart.”
Thank you, Professor Hahn for a most impressive work indeed.
New guidelines based on currently available evidence on fluid
therapy for resuscitation of sepsis, septic shock, trauma patients,
critically ill patients, ARDS and patients undergoing prolonged
major surgery are badly needed. Professor Hahn is the expert
witness on fluid therapy.
Why does not Hahn believe his own results? Why doesn’t he
make the most obvious conclusion based on what he said in the
abstract above? What and how much more evidence and years
that he needs to believe that the pathological VO of massive fluid
infusions induces cardiovascular shock that is VOS of both types
and causes ARDS? If my articles referenced here and the books [3-
7] particularly the one Hahn has now for 8 months and being held
in the press awaiting his introduction, then allow me most sincerely
and humbly to give you a helping hand to lift you up to where I
stand and clearly see the picture on the real issues discussed here.
Hahn does not need to do any more research studies. Just report a
re-analysis of data from previously reported articles he has done
and reported before, based on his previous published articles on
the TUR syndrome and saline-based fluid infusions. Please, reexamine
and re-analyse your own research work in a manner and
method identical to your article reported here [20]. Please, Hahn
don’t bother with equations that are hard to understand and are
meaningless and perhaps misleading or even wrong. Do not use
fancy sophisticated graphs that does not impress me. I would love,
most sincerely and humbly, to give you a hand to get you out of the
huge maze you have been lost inside it for >3 decades. All you need
to do my friend now is to liberate yourself from the illusive and
misleading concepts of the toxic/septic hypotheses of glycine and
sepsis!? One must unlearn old bad habits to be able to receive and
acquire the new correct ones.
Evidence for the VO Theory causing VOS and ARDS
“The prevalence of “liberal fluid infusion” in resuscitation of all
types of shocks not only septic shock in clinical practice all over the
world is attributed to an impactful article by Rivers et al, reported at
The N Engl J Med 2001 [37]. Dr Rivers’ investigation reported EGDT
in the treatment of severe sepsis and septic shock. In this singlecenter
study published more than 20 years ago involving patients
presenting to the emergency department with severe sepsis and
septic shock, the conclusion was: “mortality was markedly lower
among those who were treated according to a 6-hour protocol of
EGDT, in which intravenous fluids, vasopressors, inotropes, and
blood transfusions were adjusted to reach central hemodynamic
targets, than among those receiving usual care” Usual care means
conservative fluid regime. There is something grossly wrong with
this conclusion, but I cannot tell what is it? Not yet. Let us see what
other author investigators have said first. The EGDT of liberal fluid
infusion has been termed “aggressive” by some authors. However,
it has been adopted all over the world not only for the therapy of
septic shock but also whenever fluid therapy is required for the
management of all types of shocks.
“In another article by Dr Rivers 11 years later in 2012 [38] he
compared the liberal to the conservative approach concluding in
his last statement: “In contrast to what is true in politics, in fluid
management of acute lung injury, it is OK to be both liberal and
conservative.” So, Dr Rivers says it is OK to have it both ways: “one
for the ebb and one for the flow”! Sorry, sir, I disagree. It is not OK.
It is not politics either. No, you cannot have it both ways. The right way is only one. The issue here is how much fluid should be infused
during the ebb phase of shock and does it have a maximum limit?
Replace the loss but do not overdo it. Since the cardiovascular
system (CVS)’ maximum capacity of an adult is 7 L and the normal
blood volume is 5 L, the maximum infused volume of fluid should
be limited by the maximum capacitance of the CVS. What do you
expect when you try to fit 10-15 L of fluid into a 7 L capacity
container? Simple physics and common sense indicate that it must
spell over if it is open system or burst if closed! The cardiovascular
system is no exception. Dr Rivers should re-examine his own data
and tell us where and why he went so grossly wrong.” The EGDT has
spread like fire in a haystack, and it remains operative in current
clinical practice all over the world that is why ARDS is so common
yet remains under recognized and underestimated affecting
and killing hundreds of thousands of patients per year.” Other
authors have confirmed the significant role of VO of crystalloids
in causing the morbidity and mortality of ARDS both in adult and
children of trauma patients [39,40]. All authors have stopped
short of recognizing VOS as Cause of ARDS or MODS morbidity and
mortality. Quoting also from this article [18] I mention here the
remarkable multicenter study by Rowan et al. [41] Like Hahn they
reported results that demonstrate the massive VO retained in the
body of surviving ARDS patients. After sending 3 emails to Rowan
commending the authors on their results and asking about the dead
patients retained fluid VO, none of the 40+ authors replied.
“The PRISM Investigators reported its Trial by Rowan et al at
NEJM 2017 [41] concluded: “In this meta-analysis of individual
patient data, EGDT did not result in better outcomes than usual
care and was associated with higher hospitalization costs across a
broad range of patient and hospital characteristics.” Thank you, Dr
Rowan and colleagues for the excellent research and report. This is
good evidence-based medicine, but more is needed, from you, and
you have the data to provide it. Based on this conclusion that agrees
with other multicenter trials I wonder is time to say goodbye Dr
Rivers? The aggressive and deleterious liberal approach of EGDT is
no longer wanted. It should be abandoned immediately. Even when
the nasty liberal approach goes away, hopefully soon, it remains bad
enough with the conservative regime as it is now that must be sorted
out! I wonder what Dr Rivers has to say about this, particularly
as authors of 3 other huge prospective multicenter trials of The
ProCESS/ARISE/ProMISe reported similar conclusion by Huang et
al. [42]. So, Rowan gave the results of: The cumulative VO was -136
ml in the conservative-strategy group, as compared with 6992 ml
in the liberal-strategy group (P<0.001). For patients who were in
shock at baseline, the cumulative seven-day VO was 2904 ml in the
conservative-strategy group and 10,138 ml in the liberal strategy
group (P<0.001). For patients who were not in shock at baseline,
the cumulative VO was −1576 ml in the conservative-strategy
group and 5287 ml in the liberal-strategy group (P<0.001)”. “First,
the negative sign (-) indicating negative fluid balance has appeared
in the data above and is very important. It characterizes the nonsymptomatic
patients among the conservative-strategy group.
These patients should be used as the controls for the statistical
analysis of the data. I have been waiting for 40 years to see these VO
results. I am still waiting to see VO data with statistical significance
in mortality patients. I plead with and urge the respected authors
of major randomized Trials of FACCT, PRISM, ProCESS, ARISE, and
ProMISe to come forward with these data, please,
Clinical picture of (VOS, The TUR syndrome, ARDS and MODS)
The clinical picture of ARDS is that of the multiple organ dysfunction syndrome (MODS) (Table 1) reported previously by Khadarow and Marshal in 2002 [43]. Another remarkable article was reported by Schrier in 2010 [44]. Demonstrating the link of the TUR syndrome with ARDS by having identical clinical picture with minor variations was reported by Ghanem as complications of VO covering the cardiovascular/hematological that appear first under general Anaesthesia with bradycardia [45], the cerebral/ neurological with coma appear first under spinal/epidural Anaesthesia and convulsions and bizarre paralysis predominate in the TUR syndrome, not in ARDS [46], the respiratory of ARDS and hepatic/gastrointestinal manifestations [47] and AKI predominate later were documented recently in individual specific reports. Excessive bleeding and leukocytosis in the absence of sepsis also occur.
Therapy of VOS, the TUR syndrome and ARDS [17] Prevention
Based on the above discussion, ARDS is an iatrogenic complication of fluid therapy in hospital, never in community, that is overlooked and underestimated. Being iatrogenic; means it is preventable. In order to prevent VOS and ARDS a limit to the maximum amount of fluid used during shock resuscitation or major surgery must be agreed upon. Professor Hahn [36] found that infusing 2 L of saline to human volunteers produces symptoms. Infusing >3 L is pathological. More than 5 L is associated with deleterious morbidity [38,39]. So, the maximum volume of fluids that can be infused safely to an adult patient is 3 L which is the daily fluid requirement, and no more fluid of any kind is given for 24 hours except replacing the actual loss that does not include urine loss. The patient should be put on a weighing scale every day from hospital admission till discharge or death. Any retained volume of fluid above his body weight on admission is pathological. On using CVP for monitoring fluid therapy, please refrain from persisting to elevate CVP to levels above 12 and up to 18-22 cm saline [48]. This is a major cause for inducing VO and VOS and ARDS during shock resuscitation, particularly septic shock [37]. Look up any physiology textbook to find out that the normal CVP is 0 and it swings between -7 and +7 cm saline which is the level that should be aimed at in monitoring fluid replacement in shock of sepsis, trauma, and bleeding, acutely ill and during major surgery. Elevating CVP is not synonymous with elevating arterial pressure. If hypotension develops later during ICU stay, inotropic drugs, hydrocortisone 200 mg and HST should be used. The latter restores the pre-capillary sphincter tone (peripheral resistance) so that the capillary works as normal G tube again [9], but no isotonic crystalloids or colloids infusions of above the daily fluid requirement should be given. If persistence with the current liberal regimen of Early Goal-Directed Therapy (EGDT) and conservative Bolus Fluid Therapy regime continues, then more reports on ARDS will continue. Future authors will be hopefully taking into consideration the mentioned above data concerning VO/Time, or the retained fluid VO at the time of inducing ARDS or death on reporting new trials or case reports.
Treatment of ARDS [6]
Hypertonic sodium therapy (HST) of 5%NaCl and/or 8.4%NaCo3 has truly proved lifesaving therapy for the TUR syndrome and acute dilution HN [17,18] as well as Secondary VOS 2 that complicates fluid therapy of VOS 1 causing ARDS. It works by inducing massive diuresis; being a potent suppressor of antidiuretic hormone. My experience in using it for treating established ARDS with sepsis and primary VOS 2 that causes ARDS is limited. However, evidence on HST suggests it will prove successful if given early, promptly, and adequately to ARDS patients while refraining from any further isotonic crystalloid or colloid fluid infusions using saline, Hydroxyethyle starch and/or plasma therapy- just give the normal daily fluid requirement and no more. After giving HST over one hour using the CVP catheter already inserted, the patient recovers from AKI and produces through a urinary catheter massive amount of urine of 4-5 L as you watch. This urine output should not be replaced. Just observe the patient recovering from his AKI, coma and ARDS and asks for a drink. This is done in addition to the cardiovascular, respiratory, and renal support on ICU. Patients with AKI on dialysis, the treating nephrologist should aim at and set the machine for inducing negative fluid balance. The HST of 5%NaCl and/or 8.4%NaCo3 is given in 200 ml doses over 10 minutes and repeated. I did not have to use more than 1000 ml during the successful treatment of 16 patients. Any other hypertonic sodium concentration is not recommended- I know Hahn tried 1.8%NaCl and it does not work. A dose of intravenous diuretic may be given but it does not work in a double or triple the normal dose. A dose of 200 mg of hydrocortisone is most useful. Antibiotic prophylactic therapy is given in appropriate and adequate doses to prevent sepsis and septic shock. No further fluid infusions of any kind of crystalloids, colloids and blood is given. The urinary loss should not be replaced as this represent a surplus in the body and must be discarded otherwise defeats the objective of treatment.
Addendum: Relevant articles on the history of the TUR syndrome and ARDS
This addendum is dedicated to important landmark articles on the history of the TUR syndrome and ARDS that could not be fitted directly on the above focused narrative review on how the TUR syndrome has been reincarnated into ARDS. It is optional reading for the interested reader, but it completes this review. The first part is dedicated to eminent authors on the TUR syndrome and ARDS whether directly or indirectly. The second part is a section on selfreferences by the author that report important issues that highlight aspects of the presentation.
A. Other Eminent Authors
Creevy was the first author to report the TUR syndrome as acute water Intoxication [49]. Ashbaugh et al were the first to report ARDS in the Lancet in 1967 [50]. Lessels et al. reported in a letter to the editor as the only article on death during prostatectomy [51]. Hendry was first to report that the osmotic pressure of various body fluid is the same as plasma [52]. Guyton and Coleman reported the negative pressure of the subcutaneous space of -7 cm water, a fact that cannot be explained by Starling’s law [53]. Calnan et al reported the negative pressure in lymphatic vessels [54]. Renkin was the first to call for reconsideration of Starling’s law [55]. The Coshran injuries Group, Finfer, Vincent and futier et al demonstrated that oncotic pressure does not work and the argument on albumin versus saline is obsolete [56-59].
B. Self-references
Articles 60 and 61 have educational and entertainment value. Articles 62 and 63 shows the relevance of my work on ARDS to Covid-19 pandemic ARDS. Article 64- 66 corrects other received misconceptions on capillary physiology to augment the discovery of the G tube hydrodynamics and its impact on the capillary- ISF transfer. Articles 67 and 68 report the two clinical studies on which the above article is based. Article 68 corrects some errors and misconceptions on fluid therapy. Article 70 is on preventing renal failure in the critically ill patients. Article 71 reports my Experience with cystoprostadenectomy with “prostatic capsule sparing” for orthotopic bladder replacement. Article 72 is on Features and Complications of Nephroptosis Causing the Loin Pain and Haematuria Syndrome. Article 73 reports “New Discoveries in Medicine and Physiology Originated in Urology”. Article 74 is on an Update on Ghanem’s new scientific discoveries in physics, Physiology, and Medicine, Article 75 is on Goodbye Starling’s law, hello G tube.
Conclusion
The TUR syndrome as defined and characterized with acute dilutional hyponatraemia will no longer be seen in urology after the use of saline as irrigating solution in endoscopic surgery. However, the ARDS will replace it with identical clinical picture of MODS that continue to occur with high morbidity and mortality that is underrecognized and underestimated. The ARDS is common in clinical practice and is induced by excessive sodium-based fluid infusion and is likely to occur in urology due to the added risk of irrigating fluid absorption and infusion through periprostatic veins. Neither the toxic theory nor the septic theory plays the significant assumed rule in the pathogenesis of the TUR syndrome and ARDS. Both are iatrogenic complications of fluid therapy, induced by VO of > 3 L in <1 h time and is severe at 7-10 L of retained fluid VO in surviving ARDS patients wile mortality occur with 12 L, and both have preventative and curative therapy of HST of 5%NaCl and/or 8.4%NaCo3.
Conflict of Interest
Conflict of Interest: None
Funds received
Funds received: None
References
- Harrison III RH, Boren JS, Robinson JR (1956) Dilutional hyponatraemic shock: another concept of the transurethral prostatic reaction. The Journal of Urology 75(1): 95-110.
- Danowski TS, Winkler AW, Elkington JR (1946) The treatment of shock due to salt depression; comparison of isotonic, of hypertonic saline and of isotonic glucose solutions. J Clin Invest 25: 130-138.
- Ghanem AN (2018) Volumetric overload shocks or volume kinetic shocks in clinical practice. Resolving the puzzles of the transurethral resection of the prostate (TURP) syndrome, acute dilution hyponatraemia (HN) and the acute respiratory distress syndrome (ARDS) Book USA.
- Ghanem AN (2021) Scientific Discoveries of the 21st century. 2021 1st edition, Book Scholars Press, USA.
- Ghanem AN (2021) The scientific basis of fluid therapy in shock: Based on new scientific discoveries in physics, physiology, and medicine. Book Eliva Press 2021.
- Ghanem AN (2021) Acute respiratory distress syndrome (ARDS): Is it relevant to Covid-19 pandemic ARDS? The puzzle is resolved being recognized as an iatrogenic complication of fluid therapy that induce volumetric overload shocks (VOS) and cause ARDS.
- Ghanem AN (2021) New Scientific Basis Of Fluid Therapy In Shock Management: The complications. The Complete Evidence Based on New Scientific Discoveries in Physics, Physiology, and Medicine. Austin Macauley Publishers Ltd®, London, New York, Cambridge, Sharjah. February/March 2021 (In the press). Comes in 35 Chapters and 516 pages (In the Press).
- Ghanem AN (2001) Magnetic field-like fluid circulation of a porous orifice tube and relevance to the capillary-interstitial fluid circulation: Ghanem Preliminary report. Medical Hypotheses 56(3): 325-334.
- Ghanem AN (2021) Final Affirmative Proof Starling’s Law Wrong and G Tube Hydrodynamic is the Correct Replacement: New Results and Critical Analytical Criticisms of Impactful Landmark Articles. Biomed J Sci & Tech Res 33(5).
- Folkow B, Neil E (1971) Circulation. Oxford University Press, London p: 1-125.
- Keele CA, Neil E (1982) Sampson Wright Applied Physiology. 13th edition. Oxford University Press Oxford, USA.
- Ghanem (2021) Why and how Starling’s law is killing patients in clinical practice in hundreds of thousands per year? Journal of Anatomy and Physiology 2: 41-44.
- Ghanem AN, Ward JP (1988) Fluid absorption during urological surgery. Br J Uro 61: 168-169.
- Ghanem AN (1988) The Transurethral Prostatectomy (TURP) Syndrome: An Investigation of the Osmotic and Metabolic sequelae of Volumetric Overload (VO). MD Thesis. Institute of Urology & Nephrology, Mansoura University, Egypt.
- Ghanem AN, Ward JP (1990) Osmotic and metabolic sequelae of volumetric overload in relation to the TURP syndrome. British Journal of Urology 66(1): 71-78.
- Ghanem AN (2020) Volume Kinetic (VK) Shock or Volumetric Overload Shocks (VOS) In Surgical Patients. J Biomed Sci Res 2(3): 128.
- Ghanem AN (2020) Volumetric Overload Shocks Cause the acute respiratory distress syndrome: The Plenary Evidence on Patho-Aetiology and Therapy. Op Acc J Bio Sci & Res 1(4).
- Ghanem AN (2020) Volumetric Overload Shocks Cause the acute respiratory distress syndrome: Building the Bridge Between Physics, Physiology, Biochemistry, and Medicine. Biomed J Sci & Tech Res 29(1).
- Goel CM, Badenoch DF, Fowler CG, Blandy JP, Tiptaft RC (1992) Transurethral resection syndrome. A prospective study. Eur Urol 21(1): 15-17.
- Hahn RG (2021) Isotonic saline causes greater volume overload than electrolyte-free irrigating fluids. Journal of Basic and Clinical Physiology and Pharmacology (JBCPP).
- HAHN RG (1990) Fluid and Electrolyte Dynamics during Development of the TURP Syndrome. Br J Urol 66(1): 79-84.
- Rhymer JC, Bell TJ, Perry KC, Ward JP (1985) Hyponatraemia following transurethral resection of the prostate. Br J Uro 57(4): 450-452.
- Ghanem AN, Salma A Ghanem, Khalid A Ghanem, Nisha Pindoria (2018) The transurethral resection of the Prostate (TURP) syndrome and acute dilutional hyponatraemia (HN): A comprehensive literature review from first incidence in 1947 to disappearance in 2018. Global Journal of Urology and Nephrology 1: 7.
- Ghanem AN, Ghanem SA (2016) Volumetric Overload Shocks: Why Is Starling’s Law for Capillary Interstitial Fluid Transfer Wrong? The Hydrodynamics of a Porous Orifice Tube as Alternative. Surgical Science 7(6): 245-249.
- Ghanem AN (2021) Cardiovascular and Hematological Manifestations of the acute respiratory distress syndrome (ARDS) Caused by the Newly Discovered Volumetric Overload Shocks (VOS). Is it Relevant to Covid-19 Pandemic ARDS? EC Emergency Medicine and Critical Care 5(3): 1-10.
- Ghanem AN (2019) Cardiac arrest and volumetric overload shocks (VOS) complicating fluid therapy. EC Clinical and Medical Case Reports.
- Arieff AI (1986) Hyponatraemia, convulsion, respiratory arrest and permanent brain damage after elective surgery in healthy women. New England Journal of Medicine 314(24): 1529-1534.
- Starling EH (1886) Factors involved in the causation of dropsy. Lancet 2 1266-1270, 1330-1334 and 1406-1410.
- Starling EH (1896) On the absorption of fluids from connective tissue spaces. J Physiol 19(4): 312-326.
- Ghanem AN (2020) What is Misleading Physicians into giving too much Fluid During Resuscitation of Shock and Surgery that Induces ARDS and/or AKI? Asploro Journal of Biomedical and Clinical Case Reports 3(1): 90-98.
- Ghanem AN (2020) Twenty-one reasons affirming Starling’s law on the capillary-interstitial fluid (ISF) transfer wrong and the correct replacement is the hydrodynamic of the porous orifice (G) tube. Biomedical and Case Reports Open Access Open Journal. I (1): 8-11.
- Rhodin JA (1967) The ultra-structure of mammalian arterioles and pre-capillary sphincters. Journal of Ultrastructure Research 18 (1967): 181-222.
- Karnovesky MJ (1967) The ultra-structural basis of capillary permeability studied with peroxidase as a tracer. Journal of Cell Biology 35(1): 213-236.
- Hahn RG, Dull RO, Zdolsek J (2020) The Extended Starling principle needs clinical validation. Acta Anaesthesiol Scand 64(7): 884-887.
- Ghanem AN, Ghanem KA (2020) Revised Starling’s Principle (RSP): a misnomer as Starling’s law is proved wrong. Med Res Chronicles.
- Hahn RG (2017) Adverse effects of crystalloid and colloid fluids. Anaesthesiology Intensive Therapy 49(4): 303-308.
- Rivers E, Nguyen B, Havstad S (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345(19): 1368-1377.
- Rivers EP, Katranji M, Jaehne KA (2012) Early interventions in severe sepsis and septic shock: a review of the evidence one decade later. Minerva Anestesiol 78(6): 712-724.
- Jones DG (2018) Crystalloid resuscitation in trauma patients: deleterious effect of 5L or more in the first 24h. BMC Surgery 18(1): 93.
- Coons BE, Tam S, Rubsam J, Stylianos S, Duron V (2018) High volume crystalloid resuscitation adversely affects paediatric trauma patients. J Pediatr Surg 53(11): 2202-2208.
- Rowan KM (2017) PRISM Investigators Early, Goal-Directed Therapy for Septic Shock - A Patient-Level Meta-Analysis. New England Journal of Medicine 376(23): 2223-2234.
- Huang DT (2013) Harmonizing international trials of early goal-directed resuscitation for severe sepsis and septic shock: methodology of ProCESS, ARISE, and ProMISe. Intensive Care Medicine 39(10): 1760-1775.
- Khadaroo Rachel G, John C Marshall (2002) ARDS and the multiple organ dysfunction syndrome: common mechanisms of a common systemic process. Critical Care Clinics 18(1): 127-141.
- Schrier RW (2010) Fluid administration in critically ill patients with acute kidney injury. Clinical Journal of the American Society of Nephrology 5(4): 733-739.
- Ghanem (2021) Cardiovascular and Hematological Manifestations of the acute respiratory distress syndrome (ARDS) Caused by the Newly Discovered Volumetric Overload Shocks (VOS). Is it Relevant to Covid-19 Pandemic ARDS? EC Emergency Medicine and Critical Care 5(3): 1-10.
- Ghanem AN (2021) Cerebral-neurological Manifestations of the Acute Respiratory Distress Syndrome (ARDS). Acta Scientific Neurology 4(2): 1-3.
- Ghanem AN (2020) Hepatic and Gastro-Intestinal Manifestations of Volumetric Overload Shocks (VOS) Causing ARDS. Acta Scientific Gastrointestinal Disorders 3(5) (2020): 1-5.
- Ghanem AN (2019) Does Raising the Central Venous Pressure (CVP) in Treating Shock with Fluids Induce Volumetric Overload Shocks (VOS)? Advance in Cardiac Research 1(5): 000120.
- Creevey CD (1947) Hemolytic reaction during transurethral prostatic resection. J Urol 58: 125-131.
- Ashbaugh DG (1967) Acute respiratory distress in adults. Lancet 2(7511): 319-323.
- Lessels AM, Honan RP, Haboubi, NY (1982) Ali HH and Green MJ. Death during Prostatectomy. J Clin Path 35: 117.
- Hendry EB (1962) The osmotic pressure and chemical composition of human body fluids. Clinical Chemistry 8(3): 246-265.
- Guyton AC, Coleman TG (1968) Regulation of interstitial fluid volume and pressure. Annals New York Academy of Sciences 150(3): 537-547.
- Calnan JS (1972) Lymphatic surgery. Proceedings of the Royal Society of Medicine 65(1972): 715-719.
- Renkin EM (1986) Some consequences of capillary permeability to macromolecules: Starling’s hypothesis reconsidered. American Journal of Physiology - Heart and Circulatory Physiology 250: H706-H710.
- Cochrane Injuries Group (1998) Human albumin administration in the critically ill patients: systemic review of randomized controlled trials: Why albumin may not work. British Medical Journal 317(7153): 235-240.
- Finfer S (2006) Effect of baseline serum albumin concentration on outcome of resuscitation with albumin or saline in patients in intensive care units: analysis of data from the saline versus albumin fluid evaluation (SAFE) study. British Medical Journal 333(7577): 1044-1046.
- Vincent JL (2006) Resuscitation using albumin in critically ill patients: Research in patients at high risk of complications is now needed. British Medical Journal 333(7577): 10291030.
- Futier E (2020) Effect of Hydroxyethyl Starch vs Saline for Volume Replacement Therapy on Death or Postoperative Complications Among High-Risk Patients Undergoing Major Abdominal Surgery: The FLASH Randomized Clinical Trial. Journal of the American Medical Association 323(3): 225-236.
- Ghanem AN (2021) Authors and Conference Speakers Beware: Scam Master Artist Fraudsters (SMAF) are Invading Your Privacy Extorting Your Money. EC Emergency Medicine and Critical Care 5(7): 125-131.
- Ghanem AN (2021) Stupidity and Utter Stupidity: A Problem without Solution and Malady without Cure!? Perspective. EC Emergency Medicine and Critical Care 5(3): 11-16.
- Ghanem AN (2021) The War on Covid-19 Pandemic ARDS Should and Must End the Lockdown Triumphantly Soon: Only Utter Stupidity May Prevent or Prolong that. EC Emergency Medicine and Critical Care 5(4): 112-120.
- Ghanem AN (2021) Impact of COVID-19 on Surgery and Anaesthesia: Fighting Another Unique War on ARDS Relevant to Covid-19 Pandemic. EC Emergency Medicine and Critical Care 5(2): 40-52.
- Ghanem (2021) Capillary ultrastructure cardiovascular physiology: what is known, what is unknown or missing, what is wrong, and what is new? Journal of Anatomy and Physiology 2: 45-57.
- Ghanem AN (2021) The Tree Branching Law: Correcting Misconceptions on Capillary Cross-Section Areas and Blood Speed. International Journal of Science and Research (IJSR) 10 (1): 1409-1418.
- Ghanem AN (2021) Hydrodynamics of the G Tube with Physiological Relevance and Clinical Significance. J Blood Transfusions Dis 4(1): 183-188.
- Ghanem KA, Ghanem AN (2017) Volumetric overload shocks in the patho-etiology of the transurethral resection prostatectomy syndrome and acute dilution hyponatraemia: The clinical evidence based on 23 case series. Basic Research Journal of Medicine and Clinical Sciences 6(4): 35-43.
- Ghanem SA (2017) Volumetric Overload Shocks in the Patho Etiology of the Transurethral Resection of the Prostate (TURP) Syndrome and Acute Dilution Hyponatraemia: The Clinical Evidence Based on Prospective Clinical Study of 100 Consecutive TURP Patients. Surgical Medicine Open Access Journal 1(1): 1-7.
- Ghanem AN (2018) The Adult Respiratory Distress Syndrome: Volumetric Overload Shocks in Patho-Aetiology, Correcting Errors and Misconceptions on Fluid Therapy, Vascular and Capillary Physiology. Surg Med Open Acc J 2(2).
- Ghanem AN (2019) Preventing Renal Failure in the Critically Ill Patient: Identifying the Problems and Finding the Solutions. EC Emergency Medicine and Critical Care 3(6).
- Ghanem AN (2002) Experience with cystoprostadenectomy with “prostatic capsule sparing” for orthotopic bladder replacement: overcoming the problems of impotence, incontinence, and difficult urethral anastomosis. BJU Int 90(6): 617-620.
- Ghanem AN (2002) Leading Article. Features and Complications of Nephroptosis Causing the Loin Pain and Haematuria Syndrome: Preliminary Report. Ghanem AN. Saudi Med J 23(2): 447-455.
- Ghanem AN (2020) New Discoveries in Medicine and Physiology Originated in Urology. Surgical Medicine Open Access Journal.
- Ghanem AN (2020) Update on Ghanem’s new scientific discoveries in physics, Physiology, and Medicine. Research in Infectious Diseases and Tropical Medicine 2(1): 52-57.
- Ghanem AN (2020) Editorial. Goodbye Starling's law, hello G tube J Urol Nephrol 5(1).

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




