Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case report(ISSN: 2641-1687) 
Survival After Radical Surgery for Huge Sarcomatoid Bladder Tumor Volume 1 - Issue 5
Safarik L1*, Handrejch L2, Koch M2, Horáková M2 and Popílka I3
- 1Libor Safarik, Urology Clinic, Czech Republic
- 2Department of Urology and Surgery, General District Hospital, Czech Republic
- 3Department of Surgery, NH Hospital Horovice, Czech Republic
Received: May 10, 2019; Published: May 28, 2019
Corresponding author: Safarik L, Urology Clinic, Czech Republic, Czechia
DOI: 10.32474/JUNS.2019.01.000125
Case Report
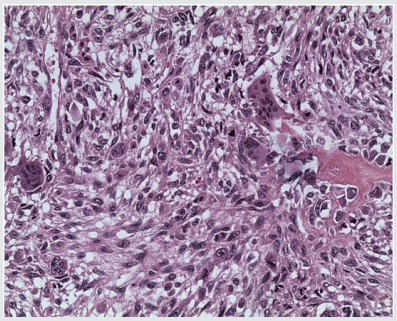
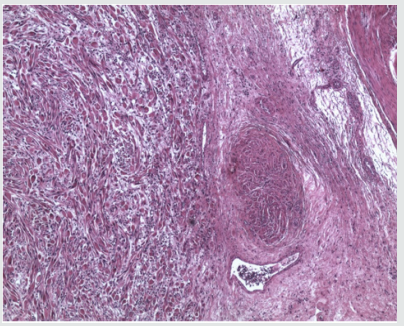
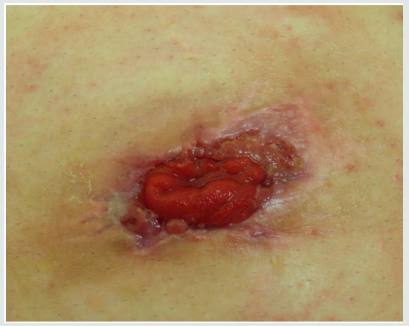
A 58-year-old male with BMI 36,8 was seen due to his allegedly three months lasting dysuria and traces of blood in his urine. His renal function was normal, CRP 18,7 and urinary sediment was flooded with red blood cells, but w/o bacterial infection. There was no dilatation on U/S, but hyperechoic exophytic mass was seen in the bladder. The CT scan showed mass, as on Figure 1a. Biopsy from the mass was taken to disclose sarcomatoid tumor of the bladder. (Figure 2a). Since there was no secondaries observable in time of CT scan and on scintigraphy, the radical cystectomy with ileal conduit was suggested. The patient agreed immediately, but there was the cardiac status in the way, since he had hardly survived severe cardiac attack with successive cardiac failure only two years ago, which did not resolved completely. The cardiac output, e.g. ejection fraction (EF), had improved only on permanent pacemaker to reach only 42%. Patient was made aware of possible serious complications after the surgery, cardiac arrest and possibility of re-operation due to his obesity and unfavorable medical status due to general ischemia and atherosclerosis. Despite that, he opted for surgical approach, since the malignancy was undisputable, he was incontinent due to lack of bladder capacity and there was intermittent urinary bleeding. Radical cystoprostatectomy with incontinent Brickere´s diversion was carried out showing deep bladder smooth muscle involvement (Figure 3a), but without pelvic nodal infiltration. Moreover, early stage prostate cancer pT1a was found despited unsuspected PSA 1.48ug/L, preoperatively. The patient was discharged on the day 16 and despite trained in stoma care together with his wife, it became very soon clear, that this procedure was out of the capabilities of the couple. The patient did not comply with ambulatory care at all, he was not able to keep the stoma clean and hence the cutaneous plate for collecting urinary bag was difficult to seal on the fatty abdominal wall resulting in urinary leakage around it. Patient had to be re-admitted to the hospital and local therapy for subcuticular abscess around the stoma had to carried out. He was discharged cured, (Figure 4a) and IVU showed normal collecting systém on both sides and ileal conduit with no urinary leakage, (Figure 5a). One month later, the man was admitted to the hospital again, due to urosepsis. As it was disclosed later on, he attempted to stop the urine coming out of the stoma with plugging it with the swab (!). He lost on weight substantially and surgical repair of the ileal conduit was suggested to cut it short a little bit, since there was no need to have it so long as it was done originally, when the patient suffered from several obesity. He refused it and bilateral nephrostomy was done successively due to urinary leakage from the abscessed conduit. Patient was left on supra-conduit urinary diversion as the permanent urinary diversion and one year after the radical surgery, he was still without detectable metastases. No adjuvant radio- or chemotherapy was done to prevent possible later malignant spread. The patient succumbed to the widespread metastatic disease after another year, accomplishing two full years after diagnosis and 22 months after radical surgery.
Discussion
Sarcomatoid bladder tumors have very bad reputation regarding the patients´survival and possible treatment. If diagnosed, the afflicted patient has his days usually numbered, as generally observed [1,2]. Despite radical approach and adjuvant chemo and possible radiotherapy, the course of the disease remains straight forward and leads to deaths, almost inevitably. The course of the disease is generally considered to be quick, and the patients experinece frequent complications, as recurrent bleeding, dysuria, infection, urosepsis, sometimes also post-renal anuria. In this case, patient was clinically unfit for chemotherapy from the very beginning, but an adjuvant possible radiotherapy on the pelvis minor (to kill the possible micrometastases in the time of surgery) might have proved to be beneficial. However, the major problem after successful surgery was patient´s uncompliance with post-operative treatment and stoma care, as well as huge obesity. Despite that, the highly demanding surgery was met with quite unusual long patient´s survival, but quality of life was rather dodgy regarding post-operative infections and subsequent urinary drainage through nephostomic catheters. The patient was quite young, 58, had clinical difficulties with bladder capacity and urinary bleeding. He did not showed any mental disorders prior to surgery, but his mental status had probably been underestimated with miserable postoperative compliance with successive medical care and possible oncological adjuvant therapy.
References
- Lopez-beltran A, Pacelli A, Rothenberg HJ (1998) Carcinosarcoma and sarcomatoid carcinoma of the bladder: clinicopathological study of 41 cases. J Urol 159(5): 1497-1503.
- Uemura K, Kawahara T, Ishida H, Nakaigawa N (2018) Sarcomatoid Variant of Bladder Carcinoma: A Case Report. Case Rep Oncol 11(3): 633-637.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...