
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case report(ISSN: 2641-1687) 
Successful Conservative Management of Triple Pelvic Outlet Functional Obstruction Syndrome with Voiding, Menstrual and Bowel Dysfunctions in an Adolescent Girl with long term follow up. Volume 4 - Issue 2
Devkumar J Govani1, Neeva Govani2, Dhaval Govani3, Namrata Panchasara4, Rasila Patel5, Partap Kumar Midha6, Rafael Cavalcante Correia7 and Ramnik V Patel8*
- 1Medical Student, B J Medical College and New Civil Hospital, India
- 2Research scholar, PGICHR and associated Uni Teaching Hospitals, India
- 3Director, Minimal invasive surgery, PGICHR and associated Uni Teaching Hospitals, India
- 4Director, PGICHR and associated Uni Teaching Hospitals, India
- 5Professor/Consultant Pediatrician, PGICHR and associated Uni Teaching Hospitals, India
- 6Medical Director and Trustee, J. Watumull Global Hospital & Research Centre, India
- 7Pediatric Surgeon, Santa Casa de Tatui General Hospital, Sao Paulo, Brazil
- 8Director-Professor, Department of Pediatric Surgery, Postgraduate Institute of Child Health and Research and K T Children Government University Teaching Hospital, India
Received: January 16, 2022; Published: January 24, 2023
Corresponding author: Ramnik V Patel, Director-Professor, Department of Pediatric Surgery, Postgraduate Institute of Child Health and Research and K T Children Government University Teaching Hospital, India
DOI: 10.32474/JUNS.2023.04.000181
Abstract
Triple pelvic outlet functional obstruction syndrome or dysfunctional elimination syndrome is a collective name given to the urinary, genital and colorectal dysfunction of the psycho-neuro-endocrine-target organs axis origin secondary to congenital and acquired disorders characterized by functional pelvic outlet obstruction in the absence of any somatic neurologic deficits. We wish to report an adolescent girl with a voiding dysfunction leading to recurrent urinary tract infection, vesicoureteral reflux and declining renal function; very painful, heavy and irregular periods and chronic refractory constipation who was successfully managed free of cost remotely by conservative management using biofeedback, dietary, micronutrient and pelvic outlet elimination retraining with a long term follow up over a decade without any recurrence of symptoms.
Keywords: Allied Hirschsprung’s disorders; congenital colorectal secreto-motility disorders; dysfunctional elimination syndrome; gastrointestinal malformation; Hinman syndrome; hypoganglionosis; idiopathic adolescent urethritis; menstrual dysfunction; voiding dysfunction
Introduction
Our team has extensive experience of dealing with pelvic outlet triple colorectal, genital and urinary systems anatomical diseases and functional disorders, congenital and acquired involving anatomical and functional problems [1-12]. However, we have never come across such an exciting case involving all three major pelvic outlet systems and implications with regards to the diagnosis and subsequent therapeutic interventions. Dysfunctional elimination syndrome is an uncommon condition in the adolescent population and typically presents earlier, often after toilet training. The condition has been found to resolve after puberty in many cases possibly due to psycho-neurological development and adolescent growth spurt related endocrine hormone surge, but our case seemed to be an exception to this rule. A study which looked at 1000 children with incontinence found that up to 32% had dysfunctional voiding [13], however results from a study evaluating approximately 1000 adult patients with intermittent flow patterns and urethral contractions / pelvic floor activity during micturition undergoing video urodynamics suggested that this disorder is more common than previously recognized, with an incidence of up to 2% [14].
Case report
A 13-year-old adolescent girl born and brought up in the United States who had normal prenatal scans was delivered at term by emergency cesarean section because of increasing fetal distress. The patient was born in good condition with normal APGAR scores and had stable vital signs. Both parents were doctors-mother being an alternative medicine practitioner and father being an internal medicine physician with special interest in nephrology. The patient passed meconium and urine in the first 24 hours but after a few months in infancy developed chronic intermittent constipation treated with laxatives as required. The patient had severe nappy rash with vulvovaginitis initially followed by recurrent febrile urinary tract infections mainly with E Coli. The ultrasound showed dilated refluxing left ureter which was confirmed by a voiding cystourethrogram (Figure 1). The initial DMSA scan showed right kidney function of 52% and left kidney function of 48%. The patient was managed initially with laxatives and wait and watch policy. However, with recurrent febrile urinary tract infections, prophylactic antibiotics were started till the age of five years and then discontinued.
Figure 1: A: Previous voiding cystourethrogram showing grade 4 VUR on the left side. B: Immediate post-void radiograph showing significant dilation and tortuosity of the left ureter. C. Recent Indirect MAG3 scan showing reducing renal function LK 40% and RK 60% with large capacity bladder and refluxing dilated tortuous left ureter.
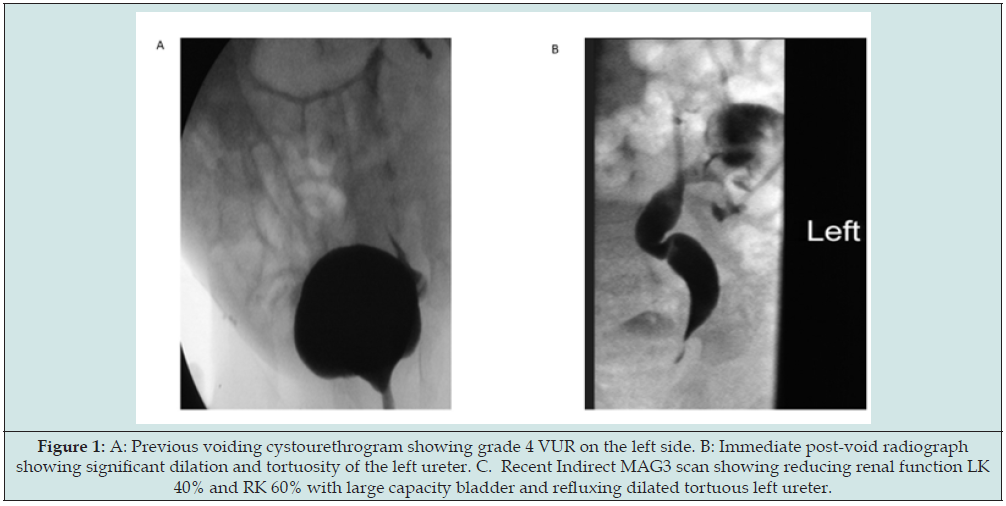
Figure 2: Recent pelvic ultrasound with A: Longitudinal view, B: Transverse view and C: Indirect MAG3 scan showing reduction of left renal function and dilated large bladder with refluxing left dilated and tortuous ureter.
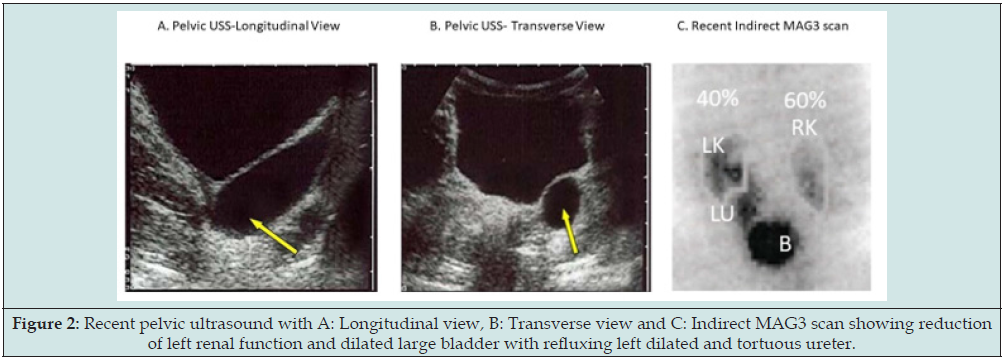
The patient was well for a while but again started having recurrent urinary tract infections with refractory constipation recently once she started her puberty in the last few months and had had breakthrough infections despite prophylaxis. A repeat ultrasound showed worsening dilatation and reflux into the left ureter with increase renal scars on left kidney and the indirect MAG3 scan confirmed left vesicoureteral reflux and the renal function had dropped to left kidney at 40% and right kidney having 60% function (Figure 2). During the last year after starting menarche, periods have started to be painful, with profuse bleeding at times with clots, colic and have gone irregular despite taking tranexamic acid and hormone pills. All laboratory investigations including the complete blood count, biochemical profile and coagulation screen were normal. In view of the worsening urinary symptoms, left renal scars and function; attending urologist consultation was made. A plan to go ahead with extravesical left ureteric reimplantation was made to protect the upper tract and control her recurrent urinary tract infections. However, the mother was not happy with the plan only to address the urinary tract and leaving bowel and genital tract problems as standby. Mother started doing literature search and contacting her friends.
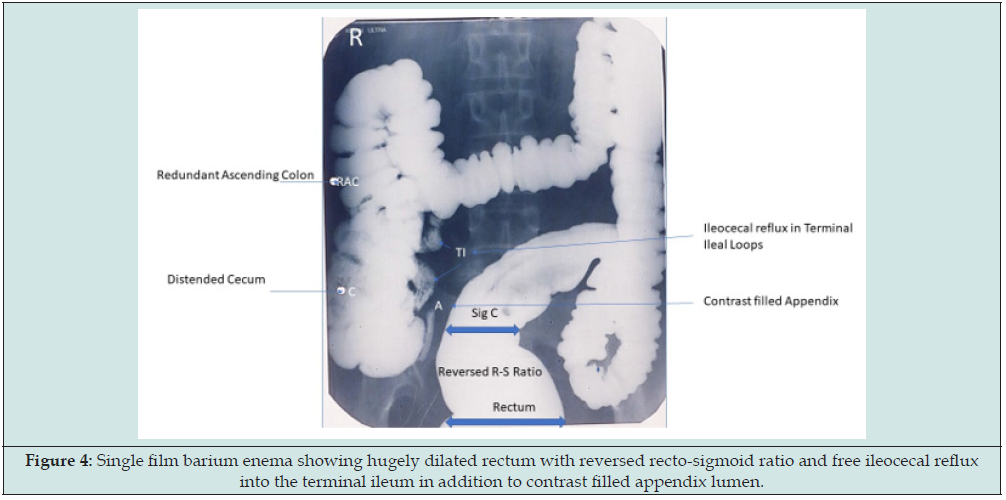
The literature search brought our team into limelight as she found all three system related publications and one of her friends had firsthand experience of successful conservative treatment of a similar adolescent girl with our team and strongly recommended second opinion. Our team was immediately contacted for a second opinion. A full comprehensive history including analysis of input output charts for last few months was undertaken which suggested possibility of congenital colorectal secreto-motility disorder. A large, pigmented patch in the sacrococcygeal skin was present from birth without any symptoms. left colonic fecal loading was grossly evident from the plain abdominal radiograph. This was confirmed by single film lower gastrointestinal contrast and radiological video recording of full procedure. The key radiological findings showed features of hypoganglionosis with gross ileocecal (Figures 3 & 4). The bladder capacity was 540 ml, and the residual urine was 115 ml at first void, 65 ml at second void and 25 ml at third void. The uroflowmetry showed very slow, intermittent and incomplete emptying of the bladder. The nephrology-urology plan to protect upper tracts, control infections and preserve renal function was reasonable from urinary tract point of view for short and medium term but if the VUR recurs then back plan was limited.
Figure 3: Plain abdominal radiograph showing rectosigmoid and left colonic loading with reversed rectosigmoid ratio and dilated redundant air-filled rest of the colon with high riding flexures and air-filled appendix due to back pressure.
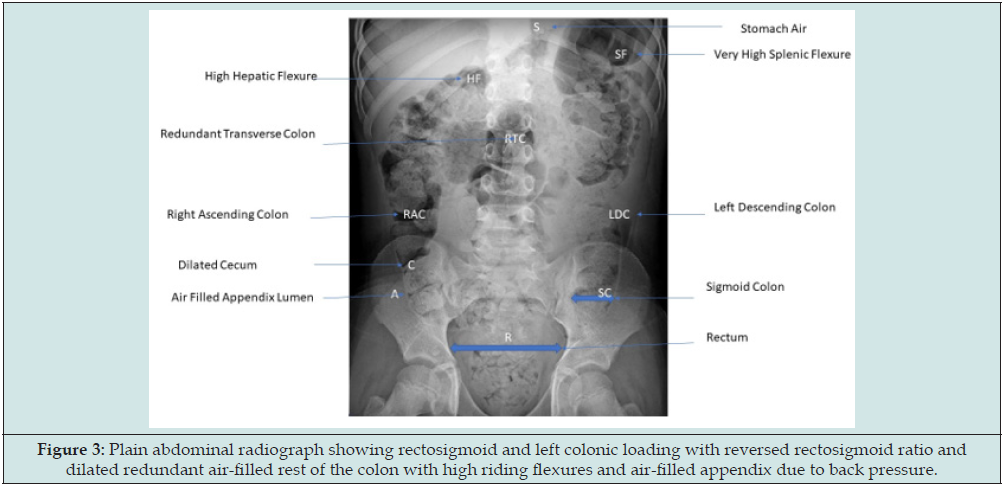
Figure 4: Single film barium enema showing hugely dilated rectum with reversed recto-sigmoid ratio and free ileocecal reflux into the terminal ileum in addition to contrast filled appendix lumen.
The mother wanted a holistic plan to resolve all three system related symptoms preferably without any invasive operative procedure. The mother asked directly if she was your daughter how you would go ahead with it. In the first instance, we use protection of health failing which prevention of conversion of disorder to disease would be the next step and unfortunately both steps have already bypassed in this case. We discussed pros and cons of all available conservative, medical, interventional and operative options and consensus that we will give a go with the conservative treatment first whole heartedly and if successful will continue steadfastly with it. However, concerns were raised whether the teenager would comply with the strict protocols and procedures for some time, but the patient proved them futile as she was determined to get back normal at any cost. Biofeedback comprehensive therapy, behavioral therapy, dietary measures with balanced diet with prebiotic, probiotic, postbiotic and holobiotic therapy, regular double or triple 2 hourly voiding and drinking liquids between 2-3 liters daily, balance between exercise and rest, pelvic muscle relaxation techniques, meditation, relaxing music therapy, micronutrient therapy, evacuation of colorectal loading to remove the reservoir of microbes and hydrodistension of the left colon to reduce the incidence and severity of ileocecal reflux and associated small intestinal bacterial overgrowth by using warm normal saline enemas initially continuously followed by intermittent ones for couple of months followed by regular laxatives to keep stools soft and formed.
Patients responded well to the treatment due to wellcoordinated and executed plans by patients and parents at home, teachers and nurses at school and at biofeedback therapy by the experts. The parents thought that taking her to their home country may help achieve their aims and objectives fast but after visiting over there they experienced the contrary and their visit was therefore curtailed, and measures continued aggressively. Within 12 months of the holistic therapy, all her symptoms of bowel, menstrual and urinary tract got resolved. The left ureteric dilatation and VUR gradually started reducing and by three years the left ureter was normal in size and shape and the VUR got resolved. The patient moved from school to college and finally to the university with very high grades at all levels and now has graduated. The patient is very much motivated to get admission to a graduate admission medical school and has become our brand ambassador for detection and correction of these disorders in her colleagues at school, college and university. The patient, parents, professionals and all parties involved in her care are very happy with the successful holistic positive outcome.
Discussion
In most children with elimination syndrome, the symptoms are mild to moderate and usually improve with advancing age. Occasionally a sever variant especially with acquired risk factors may prove refractory with worsening symptoms and failing medical management. These disorders are more common in females and associated with a higher incidence of urinary and genital tract symptoms. In the elimination syndrome, the precise pathophysiology involves bowel, bladder and cervical outlet functional obstruction. The bowel dysfunction appears to be the primary, bladder secondary and genital tract cervical outlet obstruction seems to be tertiary. The congenital colorectal secretomotility disorders are a heterogenous group of functional bowel disorders, having challenging diagnostic and management issues, are a group of allied Hirschsprung’s disorders (AHA) or Variants of Hirschsprung’s disease.” These are conditions that clinically resemble Hirschsprung’s disease (HD), despite the presence of ganglion cells in rectal suction biopsies requiring specific histological, immunohistochemical and electron microscopic investigations to detect them.
They include intestinal neuronal dysplasia, intestinal ganglioneuromatosis, isolated hypoganglionosis, immature ganglia, absence of the argyrophil plexus, internal anal sphincter achalasia and congenital smooth muscle cell disorders such as megacystis microcolon intestinal hypoperistalsis syndrome, intestinal pseudo-obstruction, ganglionitis, degenerative neuropathy, diffuse ganglioneuromatosis, malformations of the muscularis propria, degenerative leiomyopathy, leiomyositis, and mitochondriopathies [15,16]. These colorectal motility disorders of their own may remain silent but during psychological stress to the fetus, infant or child; the flight or fight mode is on and the imbalance between the sympathetic and parasympathetic nervous system leads to incoordination between involuntary internal sphincter and voluntary pelvic sphincter muscles in the bowel, bladder and cervical regions leading to increased resistance to evacuate the contents with retention reservoir associated with increased risk of growth and development of resistant microbes and lead to back pressure with reflux into the ileocecal valve, vesicoureteral reflux or retrograde flow into the fallopian tubes into the peritoneal cavity with dysmenorrhea, menorrhagia, retrograde menstruation, recurrent vulvovaginitis or ascending pelvic infection and infertility.
It is understood to be an abnormal, learned response to uncontrolled bowel, bladder or cervical contractions which usually develops early in life. These disorders may manifest as markers similar to spina bifida occulta and neurocutaneous lesions in the sacrococcygeal region without any neurological deficits. At birth, use of nappy in the neonatal and early child hood period leads to holding behaviour as wet or dirty nappy irritates the perineal area and they start holding the stool and urine which may get intensified during toilet training period and finally when they go to nursery remain busy with toys and friends and forget to drink enough water and hold their urine and stool which behaviour is often rewarded by their teachers as civilized behaviour. The lumbosacral magnetic resonance imaging in these children may have abnormalities including increased T2 signals, lower fractional anisotropy values and higher mean diffusivity values as evident from recent observations suggesting that some neurological element may be involved in addition to the psychological component in its causation [17].
This hitherto unreported observation of the triple pelvic outlet functional obstruction involving three of the major body systems alerts us to the need to carefully take detailed history from prenatal period to the current circumstances, examine the input and output diary critically, uroflowmetry, ultrasound, and evaluating all the risk factors together with any abnormal or grey zone clinical and investigative findings in such cases. Findings in our case certainly shed new light on the possible pathogenesis of this hind gut colorectal congenital secretomotor functional disorder and its natural course of the disease Increasing fecal retention may be the primary problem providing reservoir of the resistant microbial flora on one hand compressing other pelvic structures and secondarily affecting urinary tract by repeated infections and causing VUR with upper tract involvement [18] and genital tract is active only in child bearing age and can affect it tertiarily. The case has value in extending the observations that even a very educated, experienced and adult professional specialist parent and their colleagues in the friend’s circle where they have shared their problem were unable to clearly understand the nature of the problem.
Conclusion
In conclusion we believe that the series of risk factors led to the delay in the accurate diagnosis and once the underlying pathophysiology was clearly explained; the team worked so well and implemented it vigorously with very good functional recovery of the bowel, bladder and menstrual dysfunctions. Identifying and reporting these unusual cases is essential to further expand our understanding of these conditions and their potential associations. These cases illustrate the anatomic spectrum of variants of autonomic innervations of these systems as well as support intermittent spontaneous recovery of the symptoms when the circumstances being favourable thereby confusing the patient, parents, professionals and public alike thinking that the patient being nearly normal at times and have worsening symptoms especially during taxing times of the major pubertal growth spurts when they have almost used all their reserves on one hand the body growth demands goes up sharply. The professionals having knowledge, training, qualifications and experience in pediatric, surgical, urological and gynecological fields with broad spectrum coverage may be more beneficial than single system specialist to evaluate such complex case effectively holistically and comprehensively with minimum risk and maximum returns.
Acknowledgments
We are grateful to the mother of this patient who is herself an alternative medicine practitioner, patient’s father who is an internal medicine physician with special interest in nephrology and their attending urologists for referring the patient to us, being very co-operative and collaborating with her care and for subsequent implementation of the management plan and monitoring the growth, development and follow up care. We are very much indebted to this index patient for her enthusiasm and active participation to reverse all her pathophysiology within short period of 12 months and being brand ambassador for correcting many of her colleagues’ functional disorders based on her own experience and superb understanding of the underlying pathophysiology and how to reverse it back to normal physiology.
Conflict of interest
The authors have no conflict of interest to declare. No funding source was involved in this study.
Ethical approval
All procedures performed on human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the parents and all the relatives involved prior to all the procedures. Parents and all involved parties were informed about the various diagnostic and therapeutic procedures.
References
- Yadav K, Patel RV, Singh JM (1987) Fetal Surgery - An experimental gastroschisis model in fetal rabbits. Ind J Surgery 49(3&4): 118-125.
- Patel RV, Anthony FM, Govani ND, Govani DR, Panchasara N, et al. (2022) Abdominal Wall Defects and Hernias-lessons learnt from observations from the experimental fetal surgery gastroschisis model in rabbits and their clinical extrapolation. Medp Pediatr Child Health Care 1(1): 8-15.
- Aye A, Cho C, Wong V, Gayen A, Patel RV (2022) Gynecological Audit of Intravesical Injection of Botulinum toxin A for the Treatment of Overactive Bladder. Medp J Obstet Gynaecol 1(1): 202201001.
- Peeraully R, Lam C, Mediratta N, Patel R, Williams A, et al. (2019) Intradetrusor injection of botulinum toxin A in children: a 10‑year single centre experience. Int Urol Nephrol 51(8): 1321-1327.
- Govani DJ, Trambadia RA, Chhaniara RA, Mirani ZR, Zaparackaite I, et al. (2023) Gastroschisis- Past, Present and Future. JSM Gastroenterology and Hepatology.
- Govani DJ, Trambadia RA, Chhaniara RA, Mirani ZR, Corracia RC, et al. (2023) Pre-operative diagnosis of Infantile Waugh’s Syndrome associated with hypoganglionosis- key radiological findings. SMP Pediatrics and Child Health. SciMedPress EMS.
- Trambadia RA, Anthony FM, Chhaniara RA, Govani D, Corracia R, etal. (2023) Congenital Neonatal Colonic Atresias arising in watershed areas of the colonic blood supply. JIMA.
- Govani DJ, Trambadia RA, Chhaniara RA, Mirani ZR, Patel RV, et al. (2022) “Is anemia frequently recognized in gastroschisis compared to omphalocele? A multicenter retrospective study in southern Japan” by Sugita, K et al. Pediatr Surg Int 39(1): 26.
- Govani DJ, Anthony FM, Trambadia RA, Chhaniara RA, Midha PK, et al. Toxic Shock Syndrome in an Adolescent Girl who had Previous Hematometrocolpos. J Gynecol Women’s Health 24(2).
- Trambadia RA, Anthony FM, Chhaniara RA, Govani DR, Correia RC, et al. (2022) Hirschsprung- Associated recurrent enterocolitis in a case of trisomy 21 an atrioventricular septal defect. Front Infect Dis Microbiol 2: 110-113.
- Patel RV, Gorasia RP, Govani ND, Anthony FM, Govani DR, et al. (2022) Successful Resolution of Secondary Infertility following Treatment of Fourth-Degree Perineal Tear through Neglected Recto-Vestibular Fistula in an Adult Female with Anorectal Malformation. Medp J Obstet Gynaecol 1(1): 202204001.
- Peeraully R, Handerson K, Fairbrother K, Patel R, Fraser N, et al. (2020) Effect of Surgical Specialty on Management of Adnexal Masses in Children and Adolescents: An 8-Year Single-Center Review. J Pediatr Adolesc Gynecol 33(1): 89-92.
- Hoebeke P, Van Laecke E, Van Camp C, Raes A, Walle J (2001) One thousand video-urodynamic studies in children with non-neurogenic bladder sphincter dysfunction. BJU Int 87(6): 575-580.
- Groutz A, Blaivas JG, Pies C, Sassone AM (2001) Learned voiding dysfunction (non-neurogenic, neurogenic bladder) among adults. Neurourol Urodyn 20(3): 259-268.
- Friedmacher F, Puri P (2013) Classification and diagnostic criteria of variants of Hirschsprung's disease. Pediatr Surg Int 29(9): 855-872.
- Muto M, Matsufuji H, Taguchi T, Tomomasa T, Nio M, et al. (2018) Japanese clinical practice guidelines for allied disorders of Hirschsprung's disease, 2017. Pediatr Int 60(5): 400-410.
- Tiryaki S, Eraslan C, Soyer T, Calli C, Ulman I, et al. (2019) Nonneuropathic neuropathic bladder - is it really nonneuropathic? J Urol 201(4): 802-809.
- Sinha S (2011) Dysfunctional voiding: A review of the terminology, presentation, evaluation and management in children and adults. Indian J Urol 27(4): 437-447.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




