Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Study of Bone Mineral Density by Dual-Energy X-Ray Absorptiometry in Hemodialysis Patients: about 18 Cases Volume 3 - Issue 5
Mahmoud BOUSAKHRIA1*, Djahid BENDJEDDOU1, Nassim MEGUELLATI1, Nacereddine REGUAIGUIA1, Saïd DIAR2, Mohamed NEZZARI2 and Laid SAHRAOUI2
- 1Department of Nephrology, Military Hospital, Faculty of Medicine, University of Constantine 3 - Salah Boubnider, Algeria
- 2Department of Nuclear Medicine, Military Hospital, Faculty of Medicine, University of Constantine 3 - Salah Boubnider, Algeria
Received: October 10, 2022; Published: October 20, 2022
Corresponding author: Mahmoud BOUSAKHRIA, Department of Nephrology, Military Hospital, Faculty of Medicine, University of Constantine 3 - Salah Boubnider, Algeria
DOI: 10.32474/JUNS.2022.03.000173
Abstract
Introduction: Chronic renal failure is a common pathology that causes early disturbance of phosphate and calcium metabolism, leading to secondary hyperparathyroidism, affecting bone and mineral metabolism, and bone loss is common and silent. It is characterized by osteopenia, deterioration of bone quality, and altered bone structure. Our work aims to determine bone status by examining the clinical, biological characteristics and bone mineral density (BMD) of hemodialysis patients at Constantine Military Hospital (CMH).
Methods: This was a prospective study involving all CMH hemodialysis patients. Biological assessment assesses bone damage and the elements used in current practice (calcemia, phosphate and parathyroid hormone) and two-photon absorptiometry (DXA) assesses BMD.
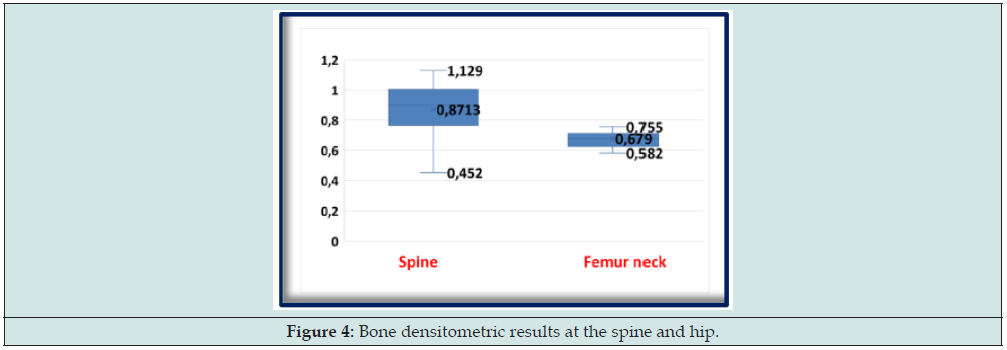
Results: This study involved 18 male and female patients with a sex ratio of 1 and a mean age of 50.94 ± 17.46 years who received hemodialysis for a mean treatment duration of 8.72 years. Hypocalcemia accounted for 44.4%, hyperphosphatemia accounted for 61.1%, and hyperparathyroidism accounted for 50%. The mean BMD for our entire population was 0.871 ± 0.174 g/cm2 in the lumbar spine and 0.679 ± 0.099 g/cm2 in the left hip. Mean T-scores were -1.628 ± 1.197 SD for the lumbar spine and -1.861 ± 0.622 DS for the left hip. We found 33.3% osteoporosis (83.3% trabecular osteoporosis) and 66.7% osteopenia, including 83.3% cortical osteopenia.
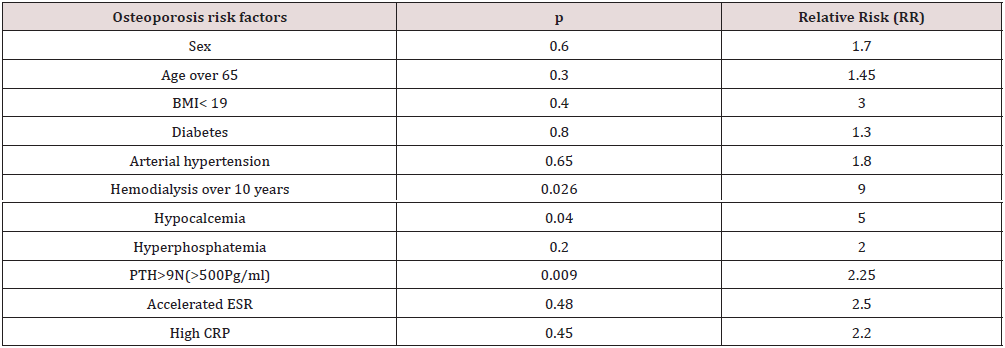
Multivariate analysis could identify 03 risk factors for osteoporosis in a statistically significant manner, namely, duration of hemodialysis greater than 10 years, hypocalcemia, and hyperparathyroidism greater than 500 Pg/ml.
Conclusion: Disturbed calcium phosphate metabolism and its skeletal consequences are certain and common complications in hemodialysis patients. It has a greater effect on cortical bone. Early detection and preventive measures are necessary.
Keywords: Hemodialysis; secondary hyperparathyroidism; bone mineral density; osteoporosis
Introduction
Chronic renal failure (CRF) is associated with dysregulated calcium phosphate metabolism once the glomerular filtration rate falls below 60 ml/min. In addition, CRF disrupts many other functions, such as the regulation of blood pH or nutrition, and is involved to varying degrees in inflammatory phenomena, which are more or less bone-specific [1]. Renal osteodystrophy is the term used to describe the various skeletal symptoms and biological abnormalities of calcium phosphate metabolism observed during CRF. However, in 2006, the KDIGO (Kidney Disease Improving Global Outcomes) consensus meeting proposed the use of the term Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) to define the systemic disease of CKD that affects metabolism. Bone and minerals [2], including biological abnormalities of calcium phosphate metabolism, qualitative and quantitative abnormalities of bone, and vascular calcification.
In hemodialysis patients, bone complications are almost constant, either specific: secondary hyperparathyroidism, adynamic osteopathy, or non-specific: osteoporosis and osteomalacia [3]. These complications lead to an increased risk of fracture. Osteoporosis in patients with CRF is defined as a decrease in bone mineral density (BMD) or the occurrence of an osteoporotic fracture [4]. Biological assessments to assess skeletal involvement include elements used in current practice (calcemia, phosphataemia, total alkaline phosphatase, bone alkaline phosphatase, parathyroid hormone, and 25-OH vitamin D) and other Elements useful in complex clinical situations: markers of bone resorption (crossoverlap) and markers of bone formation (osteocalcin, N-terminal propeptide of collagen type 1, P1NP) [5]. In imaging, dual X-ray absorptiometry (DXA), the reference method for measuring bone mass, has reported a decrease in BMD in dialysis patients [6]. Internationally, several studies have identified risk factors for bone loss in the general population. In hemodialysis patients, BMD could be affected by multiple factors that overlap. These factors are little studied and remain poorly understood by practitioners. Over the past few decades, BMD measurement has demonstrated its reliability in monitoring bone loss in hemodialysis-related osteoporosis. But its use in the evaluation of the bone status of uremic is not yet well established knowing that more than a third of hemodialysis patients present bone loss with a fracture risk four times greater than the general population.
Methods
This is a descriptive, prospective study, of interest to all chronic renal failure patients on hemodialysis at Constantine Military Hospital (CMH) in 2021. The data is collected prospectively and recorded on a data collection medium including age, sex, history and initial nephropathy. A biological assessment assessing bone damage and including elements used in current practice: calcaemia, phosphatemia and parathyroid hormone (PTH) and other assessments (hemoglobin, uric acid, erythrocyte sedimentation rate (ESR) and C-reactive protein). The bone densitometric study of the patients was carried out by DXA using a Hologic® Horison type device located in the nuclear medicine department. The data collected was entered into an Excel table and then exported in a format that could be analyzed by SPSS version 25. The qualitative variables are described according to their percentage distribution. For quantitative variables, we calculated the mean, 95% confidence interval, and standard deviation. The risk of alpha error is set at 5% and the p represents the degree of significance of the statistical test.
Results
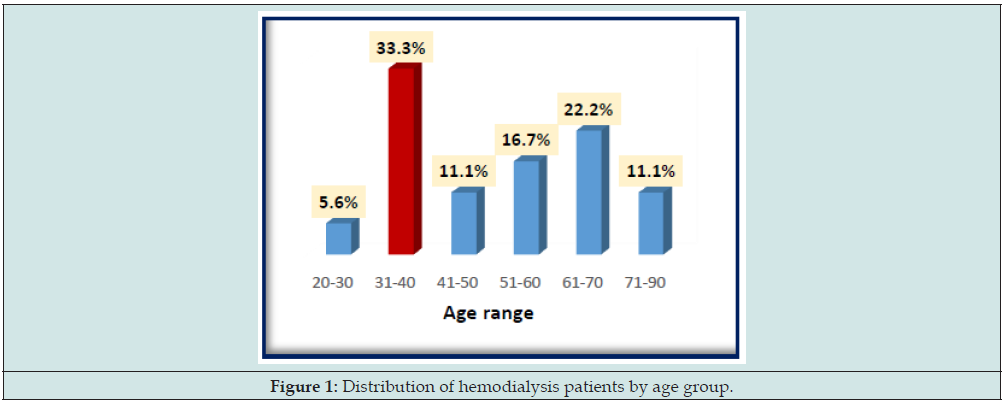
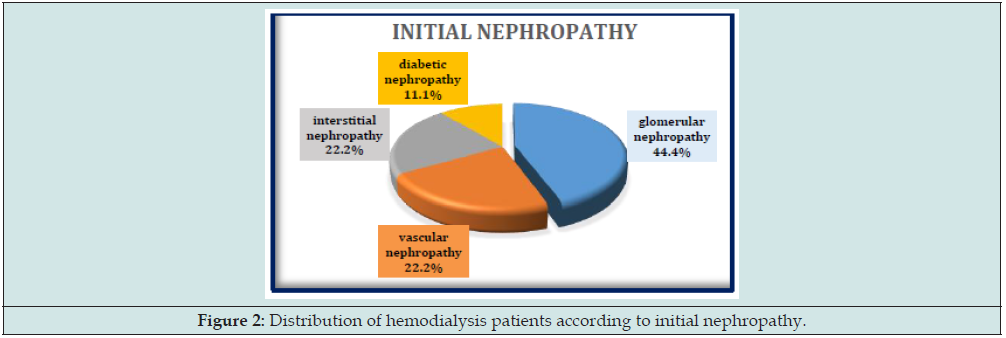
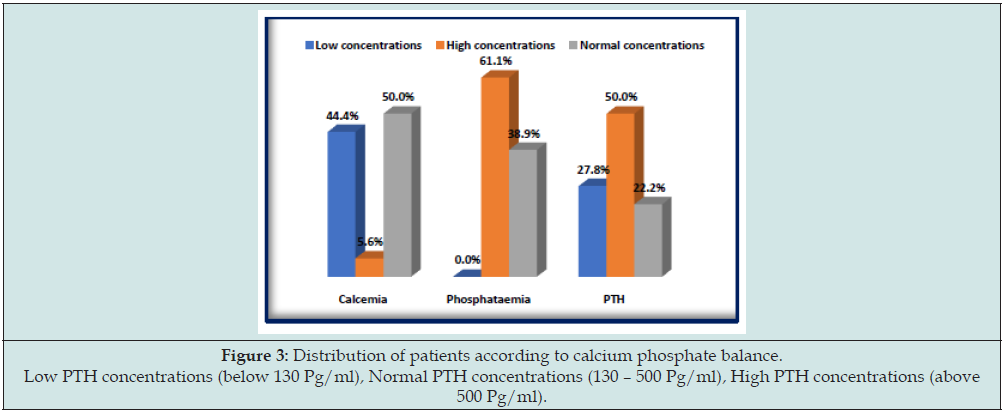
Our study was conducted in 2021 in 18 chronic hemodialysis patients at CMH. There are 9 men and 9 women, with a sex ratio of 1. The average age is 50.94±17.46 years. The median is 49.5 years with age extremes ranging from 26 to 88 years. Half of our patients are under 50 years old. The 31-40 age group is the most represented in 33.3% (Figure 1). Glomerular nephropathy is the leading cause of end-stage CRF in our patients in 44.4% (Figure 2). The average duration of hemodialysis is 8.72 ± 3.878 years. According to the KDIGO 2009, the biological targets for calcium phosphate balance proposed for patients with CRF and on dialysis are total serum calcium between 2.1 and 2.55 mmol/l, serum phosphate towards the norm (0.8–1.45 mmol/l) and a serum PTH concentration two to nine times the upper limit (130–500 Pg/ml). Our patients have a correct calcemia in 50% and hypocalcemia in 44.4%. Hyperphosphatemia is found in 61.1% and PTH greater than 500 Pg/ml is found in 50% of cases (Figure 3). The inflammatory assessment finds: an accelerated ESR in 66.7% and a high C-reactive protein in 27.8%, anemia is found in 44.4% and uric acid is greater than 74 mg/l in 55.6% cases.
Figure 3: Distribution of patients according to calcium phosphate balance. Low PTH concentrations (below 130 Pg/ml), Normal PTH concentrations (130 – 500 Pg/ml), High PTH concentrations (above 500 Pg/ml).
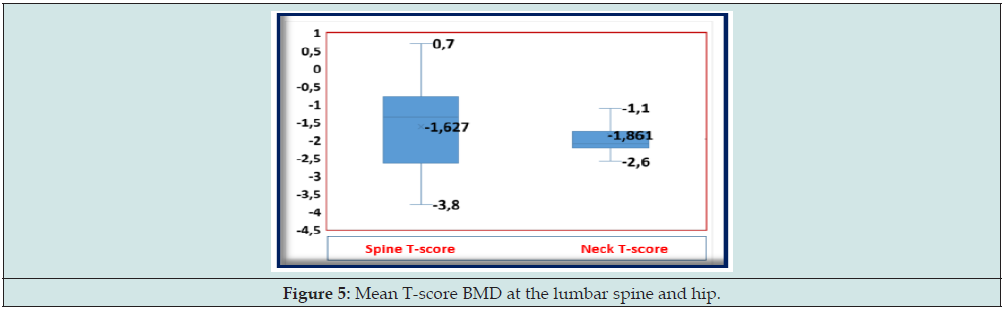
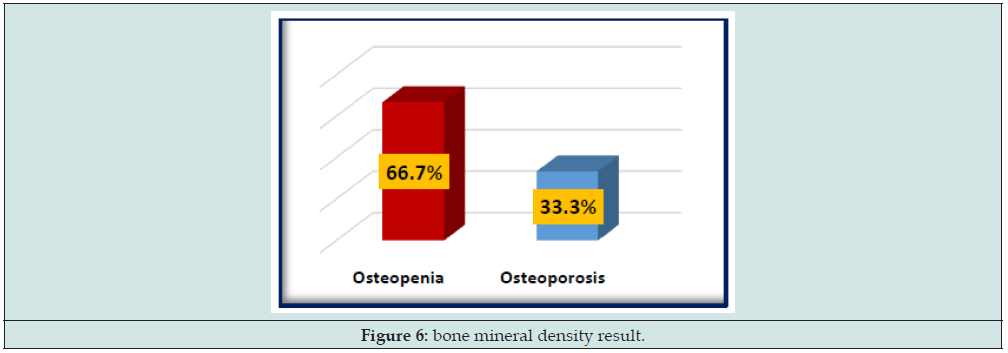
The measurement of BMD by dual X-ray absorptiometry finds an average BMD at the level of the spine is 0.871 ± 0.173 g/cm2 with a maximum of 1.129 g/cm2 and a minimum of 0.452 g/cm2, and 0.679±0.099 g/cm2 at the left hip with a maximum of 0.755 g/ cm2 and a minimum of 0.582 g/cm2 (Figure 4). The mean standard deviation T-scores, all sexes combined, is -1.628 ± 1.197 SD at the level of the spine and negative -1.861 ± 0.622 SD at the level of the left hip. (Figure 5). Patients with a T-score < -2.5DS at the hip or spine were classified as having had osteoporosis. The prevalence of osteoporosis is 33.3% (T-score <2.5) including 83.3% trabecular osteoporosis, while osteopenia is found in 66.7% including 83.3% osteopenia cortical (Figure 6). The multivariate analysis made it possible to note in a statistically significant way 03 risk factors of osteoporosis and which are the duration of hemodialysis superior to 10 years (p=0,026), the hypocalcemia (p=0,04) and the hyperparathyroidism greater than 500 Pg/ml (p=0.009). These risk factors are represented in the Table 1.
BMI: body mass index, PTH: parathyroid hormone, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein.
Discussion
In our study, the results of bone densitometry by DXA showed that all hemodialysis patients have bone fragility, of which 33.3% of cases have osteoporosis. But they remain less obvious in comparison with the data of the literature. This could be explained by the small size of our sample and the relatively young age of our patients. Several studies have already found that BMD was decreased in dialysis patients [7]. In the Benhiba study [8], in 57 hemodialysis patients, BMD revealed the existence of osteopenia in 12 patients (21.1%) and osteoporosis in 6 patients (10.5%) at the level of the lumbar spine. At the hip, osteopenia affected 15 patients (26.3%) and four patients had osteoporosis (8.8%). While in the Ramirez study [9], the majority of hemodialysis patients present with low bone density BMD either at the level of the spine or the left hip. About half of these patients have at least a T-score <-2.5DS (osteoporosis). In the Gharsallah study in 2014 [10], in 45 hemodialysis patients, he noted 33.3% osteoporosis, 37.8% osteopenia, and 28.9% normal bone status.
In hemodialysis patients, the BMD is lowered, but it alone cannot account for the quality of the bone and its mechanical resistance. Thus, several elements must be taken into consideration when interpreting BMD results in this population. On the one hand, mineralization disorders are frequent in uremic patients, and we can no longer, then, assimilate bone mass to BMD. On the other hand, a decrease in BMD in a patient on dialysis does not necessarily mean pure bone loss, but may result, to varying degrees, from primary and secondary mineralization disorders. Furthermore, CRF affects the trabecular and cortical compartments differently. Finally, the measurement of the lumbar spine is an anteroposterior projection of the spine and therefore includes aortic calcifications in the results, which are frequent in patients with renal failure. It has been proposed that the wrist site is preferred because it is less biased in CRF [11], and that the Z-score be used instead of the T-score in the interpretation of the results [12]. These elements most likely account for the low prevalence of bone loss in this study. Indeed, apart from the size of the sample and the young age of the patients, this prevalence is underestimated by the frequency of osteoarthritis in the lumbar spine, the presence of aortic medical cosis and calcifications of the soft tissues due to phosphorus deposits. These elements make the BMD artificially increase a priori.
The multivariate analysis made it possible to note in a statistically significant way 03 risk factors of osteoporosis and which are the duration of hemodialysis higher than 10 years, the hypocalcemia and the hyperparathyroidism higher than 500Pg/ml. Our study did not show that advanced age is involved in bone loss in chronic hemodialysis patients, since our population at a young age, unlike other studies, they all concluded that the older the age of hemodialysis is higher the more the bone loss is important, in particular for the female sex. Thus, we did not find a link between sex and osteoporosis, knowing that multiple studies have found correlations between female sex and low BMD of the hip and lumbar spine and the risk of have a femoral neck fracture [13]. We now know that low weight and a BMI of less than 19 kg/m2 are considered risk factors for osteoporosis in ordinary people [14]. In chronic hemodialysis patients, studies have reported the same observation. Our study did not show this link. Several studies have found a positive correlation between BMI and BMD at the hip and lumbar spine. A study even reported that a low BMI is the most important factor of bone loss in subjects on hemodialysis [15].
The protective role of the high BMI can be explained by the importance of the fatty layer, particularly at the level of the points of impact such as the hip, which would play a role of shock absorber during falls, and the role of adipocytes that produce estrogen by aromatization of adrenal androgens after menopause [16]. Several studies have shown that the BMD of patients decreases with increasing duration of hemodialysis [17,18]. The relative hypocalcemia due to the decrease in renal tubular reabsorption and intestinal absorption of calcium as well as the use of calcimimetics or bisphosphonates, directly stimulates the synthesis of PTH mRNAs, as well as its secretion, by stimulation of the calcium-sensitive receptors (CaSR) of parathyroid cells, this increase in PTH induces bone loss. Hypocalcaemia, whatever the cause (calcium deficiency, vitamin D deficiency, use of calcimimetics or bisphosphonates) promotes bone mineralization disorders (osteomalacia). Although our patients had very high phosphate levels on average, we found no relationship with osteoporosis.
PTH greater than nine times the upper limit (> 500 Pg/ml) is considered a risk factor for osteoporosis by our work. In the literature, the various studies have been discordant as to the threshold of PTH favoring bone loss in subjects with hemodialysis. Some authors consider that a low PTH (less than 70 Pg/ml) is a risk factor [19]. On the other hand, many studies demonstrate the deleterious effect of a high level of PTH and alkaline phosphatase on the BMD of the hip and lumbar spine. Excess PTH affects the development of different bone cells and thus alters the quality of bone, especially cortical bone, by increasing the rate of bone remodeling. Finally, according to a last study, a PTH between 227 and 538 pg/ml was protective compared to the other thresholds: this is the optimal level to respect [20]. The preventive therapeutic measures making it possible to avoid renal osteodystrophy in chronic hemodialysis patients are based on the prevention of phosphorus retention and hypocalcemia by the administration of a native or 25 hydroxylated vitamin D supplement, and by the contribution alkaline calcium salt which prevents the retention of phosphorus [21].
Conclusion
Disturbance of calcium phosphate metabolism and its consequences on the skeleton (bone loss) is a certain and frequent complication in hemodialysis patients. It affects more significantly the cortical bone. Kidney patients on hemodialysis are particularly at risk of osteoporosis. Our work revealed the existence of osteopenia in 12 patients (66.7%) including 83.3% cortical osteopenia and osteoporosis in 6 patients (33.3%) including 83.3% trabecular osteoporosis. Our study showed that among the risk factors for osteoporosis in chronic hemodialysis patients are a duration of hemodialysis greater than 10 years, hypocalcemia and hyperparathyroidism. It is therefore necessary to define a preventive strategy for these populations of patients aimed at identifying the patients most at risk of osteoporosis according to biological and especially radiological data by taking advantage of new bone imaging techniques, in particular bone densitometry. Early detection and preventive measures are necessary.
References
- Mac Way F, Lessard M, Lafage-Proust M (2012) Pathophysiology of renal osteodystrophy. Revue du Rhumatisme 79: A18-A21.
- Moe S, Drüeke T, Cunningham J, Goodman W, Martin K, et al. (2006) Definition, evaluation, and classification of renal osteodystrophy: a position statement from kidney disease: Improving Global Outcomes (KDIGO). Kidney Int 69(11): 1945-1953.
- Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, et al. (2000) Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int 58(1): 396-399.
- De Vernejoul M-C, Cohen-Solal M (2001) Osteoporosis of renal osteodystrophy. Revue du Rhumatisme 68(8): 691-692.
- Ureña P, Vernejoul MC (1999) Circulating biochemical markers of bone remodeling in uremic patients. Kidney Int 55(6): 2141-2156.
- Gonzalez E, Lamy O, Hans D, Favre, Pralong F (2015) Imageriepar DXA: the multifunction Swiss army knife? Revue Médicale Suisse 11: 645-650.
- Jean G, Chazot C (2019) Complications and treatment of mineral and bone disorders in chronic kidney disease. Nephrol Ther 15(4): 242-258.
- Benhiba I, Niamane R (2010) Prevalence of bone loss and osteoporotic fractures in chronic hemodialysis patients.
- Ramirez C (2012) Diagnosis and prognosis of mineral and bone disorders associated with chronic kidney disease in hemodialysis: Contribution of clinical and biological markers. pp. 27-33.
- Tliba A, Gharssalah I, Metoui L, Ajili F, Labidi J, et al. (2013) Étude de la densité minérale osseuse chez les patients hémodialysés : à propos de 45 cas. La Revue de Médecine Interne 34: A82.
- Yamaguchi T, Kanno E, Tsubota J, Shiomi T, Nakai M, et al. (1996) Retrospective study on the usefulness of radius and lumbar bone density in the separation of hemodialysis patients with fractures from those without fractures. Bone 19(5): 549-555.
- Cunningham J, Sprague SM, Cannata-Andia J, Coco M, Cohen-Solal M, et al. (2004) Osteoporosis in chronic kidney disease. Am J Kidney Dis 43(3): 566-571.
- Huang GS, Chu TS, Lou MF, Hwang SL, Yang RS (2009) Factors associated with low bone mass in the hemodialysis patients–a cross-sectional correlation study. BMC Musculoskelet Disord 10: 60.
- Maurice Audran (2004) Intérêt, limites et conséquences de la recension des facteurs de risque d'osté Revue du Rhumatisme 71(9): 734-736.
- Rasic-Milutinovic Z, Perunicic-Pekovic G, Stojanovic O, Tica J, Popovic V, et al. (2009) Body composition and bone mineral density in hemodialysis patients. 11th European Congress of Endocrinology, BioScientifica, Europe.
- Shilbayeh S (2003) Prevalence of osteoporosis and its reproductive risk factors among Jordanian women: a cross-sectional study. Osteoporos Int 14(11): 929-490.
- Urena P, Bernard-Poenaru O, Ostertag A, Baudoin C, Cohen-Solal M, et al. (2003) Bone mineral density, biochemical markers and skeletal fractures in haemodialysis patients. Nephrol Dial Transplant 18(11): 2325-2331.
- Zayour D, Daouk M, Medawar W, Salamoun M, Fuleihan G (2004) Predictors of bone mineral density in patients on hemodialysis. Transplant Proc 36(5): 1297-1301.
- Coco M, Rush H (2000) Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis 36(6): 1115-1121.
- Stehman-Breen CO, Sherrard DJ, Alem AM, Gillen DL, Heckbert SR, et al. (2000) Risk factors for hip fracture among patients with end-stage renal disease. Kidney Int 58(5): 2200-2205.
- Harbouche L, Shahapuni I, Monge M, Araar B, Rahmouni K, et al. (2006) Place des nouveaux traitements de l'ostéodystrophie rénale: dérivés 1α-hydroxylés de la vitamine D «non hypercalcémiants», complexants non calciques, non magnésiens et non aluminiques des phosphates, et calcimimé Immuno-analyse & Biologie Spécialisée 21(1): 9-32.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...