
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case report(ISSN: 2641-1687) 
Renal Vein Thrombosis Secondary to Sepsis from Obstructive Pyelonephritis Volume 4 - Issue 3
H. Elkaddouri*, E Cogan, C Schulman, A Corbusier, C Chatzopoulos
- Department of Urology, Delta Hospital (CHIREC), Free University of Brussels, Belgium
Received: May 15, 2023; Published: May 31, 2023
Corresponding author: H. Elkaddouri, Department of Urology, Delta Hospital (CHIREC), Free University of Brussels, Belgium
DOI: 10.32474/JUNS.2023.04.000190
Abstract
Nephrotic syndrome and malignancy are the major causes of renal vein thrombosis (RVT). Pyelonephritis is a less common cause. The treatment is critical because the complication of RVT can be fatal. This is a case report of acute obstructive pyelonephritis complicated with RVT full recovery after antimicrobial, a double J stent and anticoagulation treatment.
Keywords: Renal vein; obstructive pyelonephritis; nephrotic syndrome; malignancy
Introduction
Nephrotic syndrome and malignancy are the major causes of renal vein thrombosis (RVT). Pyelonephritis is a less common cause. The treatment is critical because the complication of RVT can be fatal. This is a case report of acute obstructive pyelonephritis complicated with RVT full recovery after antimicrobial, a double J stent and anticoagulation treatment.
Case Report
A 50-year-old woman presented to the emergency department complaining of left flank pain, nauseas and urinary burns since the day before. She had a history of a herniated L5-S1 disc. Her hemodynamic parameters were normal, and she had no fever. She weighed 69 kg with a height of 172cm. Initial laboratory tests revealed with blood cell count of 18,300/mm3, platelets of 179,000/mm3 sodium of 133mmol/L, potassium 4,5 mmol/L, bicarbonate of 22 mmol/L, chloride of 96 mmol/L, creatinine of 1,3 mg/dL, uric acid of 4,2mg/dL, glucose of 112mg/dL, C-reactive protein (CRP) of 194,9 mg/L, International Normalized Ratio (INR) of 1,3, fibrinogen of 472 mg/dL and liver enzymes were normal. Urinalysis revealed more than 800 withe blood cells, 82 red bloods cells and 500 bacteria per high-power field. The nitrites and proteins were positive in the urine. On examination, she had pain in her left iliac fossa and her abdomen was soft. The COVID screening was negative. A computed tomography (CT) scan of abdomen and pelvis without intravenous (IV) contrast was ordored and showed a lithiasis of 5 mm at the level of the left pyeloureteral junction (Figure 1), dilatation of the pyelocal cavities upstream with a pelvis measuring 17 mm and discrete infiltration of the left peri-renal fat.
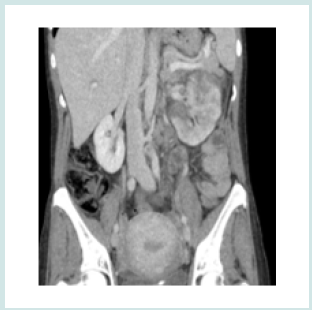
A kidney drainage with a double J stent was placed and empirical antibiotic with amoxicillin-clavulanate on IV injection was given. A bladder tube was placed at the end of the intervention. Unfortunately, the day after her flank pain worsened and edema of the lower limbs was noticed. Her inflammatory parameters (CRP of 397 mg/L) remained elevated. A CT scan of abdomen and pelvis with IV contrast showed a thrombus in the proximal portion of the left renal vein (Figure 2). There was a global enhancement defect of the kidney at the arterial and portal phases. The lithiasis was in an unchanged position. Urines cultures grew Klebsiella Pneumoniae (sensitive to ciprofloxacin, cefuroxime, cotrimoxazole, piperacilinne—tazobactam and resistant to amoxicilline and nitrofurantoin). Antibiotic therapy was changed to ciprofloxacin 500mg twice per day after the results of urinary culture and a supportive therapy with IV fluids and pain killers was administrated. An anticoagulation treatment was initiated with Low Molecular Weight Heparin (60 mg twice daily) during his hospitalization.
Figure 1: A computed tomography (CT) scan of abdomen and pelvis without intravenous (IV) contrast was ordored and showed a lithiasis of 5 mm at the level of the left pyeloureteral junction.

Figure 2: A CT scan of abdomen and pelvis with IV contrast showed a thrombus in the proximal portion of the left renal vein.
The pains disappeared progressively, and the patient was able to return home with ciprofloxacin and oral anticoagulant (rivaroxaban) 20 mg per day after five days. Rivaroxaban was continued for three months and ciprofloxacin for six weeks. A follow up CT scan at four weeks showed a partial improvement of the pyelonephritis and a complete resolution of the renal vein thrombosis. Thrombophilia screenings were normal. Extracorporeal lithotripsy focused on lithiasis was performed two weeks after anticoagulation withdrawal. The CT scan of abdomen and pelvis without IV contrast performed showed the disappearance of the lithiasis. The blood test performed at 4 months showed a normal renal function and no inflammatory syndrome. On the urinalysis at 4 months there is still proteinuria.
Discussion
RVT is a rare pathology. The most common etiologies of RVT are hypercoagulable state like in sepsis, nephrotic syndrome, malignancy, traumatic injury, protein C, protein S or antithrombin deficiency, antiphospholipid syndrome, hemorrhage, compression of renal vein in retroperitoneal malignancy and renal transplantation. Acute pyelonephritis is a very rare cause of RVT [1]. RVT is more common in males and in the left side [2]. The particularity of our case is that RVT is caused by obstructive pyelonephritis (lithiasis). This is the third case reported in the literature of pyelonephritis with lithiasis [3,4]. Pyelonephritis leads to a state of hypercoagulability that results in RVT. Endotoxins released by Gram-negative bacteria (Klebsiella pneumoniae) can cause endothelial damage leading to thrombus formation. The most common symptoms of RVT are acute flank pain, haematuria, nausea, vomiting and fever. The symptoms vary with the degree of obstruction [5]. RVT is diagnosed by imaging studies. But the blood and urine tests can support this diagnosis. It can show an anemia, an increased creatinine level, a high C-reactive protein (CRP) level, microscopic hematuria, proteinuria and albuminuria (>3g/day indicates a nephrotic syndrome), hypercoagulability disorders and hypercholesterolemia.
Abdominal ultrasound (US) can show initially a renal enlargement and later a reduction in the renal size and atrophy. The Color Doppler Ultrasound reveals a reversal of arterial diastolic flow, absent venous flow and visualization of thrombus in the lumen and a high resistance in the renal artery [6]. Computed Tomography (CT) of abdomen and pelvic with IV contrast is the imaging of choice for RVT. The thrombosis can be seen as a defect during venous phase imaging and the kidney has perfusion abnormalities. The treatment of RVT is oriented by etiology. It includes IV fluid hydration, pain killers, antibiotics and anticoagulation. Anticoagulation treatment includes low-molecular-weight heparin injections or oral anticoagulation. It should be initiated immediately after the diagnosis. The duration of anticoagulation is variable in the studies, but it should be continued for 2 to 12 months [7]. The goal of anticoagulation is not only to prevent complications of pulmonary embolism but also to delay the extension of thrombosis. Surgery like nephrectomy or thrombectomy are outdated with the medical treatments. Surgery is reserved for cases that do not improve with medical treatment. RVT can be complicated by pulmonary embolism, acute kidney injuries, hypertension, renal atrophy with end-stage renal disease and recurrent thromboembolism. The mortality of RVT has improved since the new medical therapy. The risk is that thrombosis leads to atrophy several months later.
Conclusion
Nephrotic syndrome and malignancy are the major causes of renal vein thrombosis (RVT). Pyelonephritis is a less common cause. The particularity of our case is that RVT is caused by a obstructive pyelonephritis (lithiasis). The best diagnostic method is CT with IV injection. The treatment includes antibiotics and anticoagulation. Complications can be fatal so treatment must be initiated as soon as the diagnosis is made.
References
- Ganeshan AS, Chongo AAC (2017) Renal Vein Thrombosis secondary to pyelonephritis: Case presentation. Open Science Journal 2(2): 1-11.
- Asghar M, Ahmed K, Shah SS, Siddique MK, Dasgupta P, et al. (2007) Renal Vein Thrombosis. Eur J Vasc Endovasc Surg 34(2): 217-223.
- Yildiz H, Van Nieuwenhove S, Doyen M, Yombi JC (2016) Acute pyelonephritis and renal vein thrombosis : a case report and review of literature. J Infect Chemother 22(11): 759-761.
- Lurz K, Hanna D, McGreen B, Schanne F (2018) A rare case of renal vein thrombosis secondary to Klebsiella pneumoniae pyelonephritis. Urol Ann 10(1): 103-105.
- Pollak V, Kark R, Pirani C, Shafter H, Muehrcke R (1956) Renal Vein Thrombosis and the nephrotic Syndrome. Am J Med 21(4): 496-520.
- Kang SK, Park SK (1987) Nephrotic Syndrome Associated with Renal Vein Thrombosis. Korean J Intern Med 2(1): 125-130.
- Harris LA, Van Every MJ, Fundell LJ (2012) Acute bilateral vein trhombosis secondary to sepsis from pyelonephritis. Int Braz J Urol 38(1): 132-134.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




