Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Reasons and Outcome of Patients after Permanent Transfer from Peritoneal Dialysis to Hemodialysis: A Review of 16 years of Experience in Senegal Volume 3 - Issue 3
Maria Faye1,2*, Ahmed Tall Lemrabott1,2, Niakhaleen Keita1, Moustapha Faye1,2, El Hannani S1, Mansour Mbengue2,3, Bacary Ba1, Seynabou Diagne1, Abdou Niang2,3 and El Hadj Fary Ka1,2
- 1Nephrology Department, Aristide Le Dantec University Hospital, Senegal
- 2Cheikh Anta Diop University, Dakar Senegal
- 3Nephrology Department, DalalJamm Hospital, Senegal
Received: November 16, 2021; Published: November 24, 2021
Corresponding author: Faye Maria, Department of Nephrology, Aristide Le Dantec University Hospital, 30, Avenue Pasteur, Dakar, Senegal
DOI: 10.32474/JUNS.2021.03.000161
Abstract
Introduction: Peritoneal dialysis (PD) and haemodialysis (HD) are two complementary and non-competitive renal replacement
therapy (RRT). A patient can be transferred from one technique to the other. The objective of this study was to assess the reasons for
transferring patients from PD to HD and to follow their outcome.
Patients and Methods: This is a 16-year descriptive and analytical retrospective study (March 1, 2004 - August 31, 2020)
conducted at the PD unit of the Aristide Le Dantec University Hospital in Dakar. Were included, patients on PD for at least 30 days,
over 18 years of age and permanently transferred to HD. The probability of survival for any duration of post-transfer follow-up was
estimated by the Kaplan-Meier method.
Results: The analysis covered 98 out of 113 cases. The mean age of the patients was 45.2 ± 14.09 years at the initiation of PD
and 47 ± 13.91 years at the time of transfer, with a sex ratio of 0.66. The mean duration in PD was 19.9 ± 17.25 months [range,
1.0-90.0 months]. The transfer to HD concerned 73.5% of patients in the first two years. The reasons for transfer were mainly
associated with infection (82.7%), mechanical complications (23.5%), social reasons (12.2%) and inadequate dialysis (6.1%). It
was programmed in 11.4% of cases and 6% of patients had a permanent approach. At the endpoint date, the mean duration in
hemodialysis was 43.3 months with 42.8% of patients still in HD. There was a kidney transplant patient; a return to PD. Mortality
was 34.6%. The mean HD survival was 126 months. There was a statistically significant relationship between infection as a reason
for transfer and mortality (p = 0.047).
Conclusion: The main reasons for transferring PD to hemodialysis identified in the literature are found in our context. This
transfer must be anticipated to reduce morbidity and mortality.
Keywords: Peritoneal dialysis; Transfer of Patients; Peritonitis
Introduction
Peritoneal dialysis (PD) and haemodialysis (HD) are two complementary modalities of renal replacement therapy. There is an increasing use of PD in the world, with a prevalence multiplied by 2.5 between 1997 and 2008 [1]. Indeed, this technique has shown survival rates similar to HD [2] or even better [3]. The main limitations of PD are related to the failure of the technique, forcing patients to switch to HD [4]. In the 2010 ANZDATA (Australia and New Zealand Dialysis and Transplant) report, 20% of PD patients were definitively transferred to HD [5]. Similar rates have been reported in other countries [6]. According to the REIN registry, each year 10% of patients in PD are transferred to HD, mainly during the first two years of treatment [7]. The most common causes of technique failure are peritoneal infection, inadequate dialysis, catheter dysfunction or patient choice [8-10]. In addition, the risk of transfer to HD is relatively high during the first 6 months of the onset of PD [8,9]. Several risk factors for PD technique failure have been identified. They include advanced age, high permeability of the peritoneal membrane, reduced peritoneal ultrafiltration, malnutrition, diabetes, and increased body mass index [8-11]. In Senegal, there is little or no data available that has examined the reasons for transfer and the outcome of patients transferred from PD to HD. This is why we conducted this work in order to assess the reasons for transferring patients from PD to haemodialysis and to monitor their future on haemodialysis.
Patients and Methods
This was a descriptive, analytical and multicenter retrospective
study over a period from March 01, 2004, to August 31, 2020. Were
included, all patient in PD for at least 30 days, over 18 years of age
and permanently transferred to HD. The data were collected on an
operating sheet, from the medical files.
Epidemiological data: existence of comorbidities at the start
of PD and at the time of transfer to HD (the Charlson comorbidity
score [12] was calculated retrospectively at the initiation of PD and
at the start of treatment with HD); the stay in PD and entry into HD
were analyzed. As of the August 31, 2020, point date, we have also
collected the following parameters:
a) Haemodialysis parameters: weekly number and duration
of HD sessions, mean inter-dialytic weight gain over one-week,
average dialysis dose over one week, type of vascular access:
b) For the outcome of the patients:
a. Duration in HD.
b. Status: deceased, kidney transplant returned to PD, still in
HD or lost to follow-up.
c. If death: date / year, cause.
d. If returned in DP: reasons.
Results
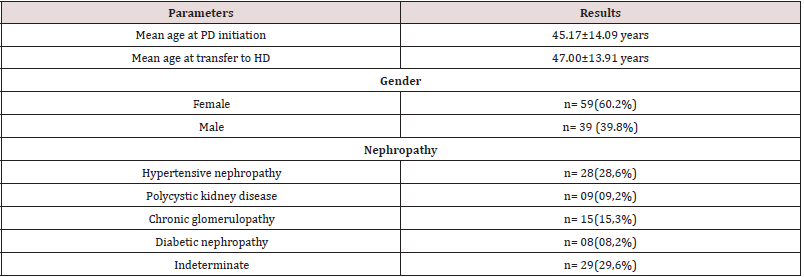
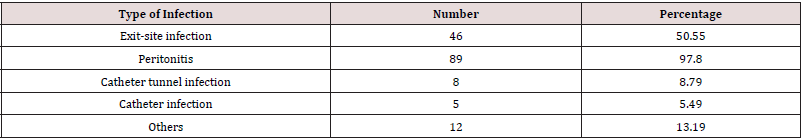
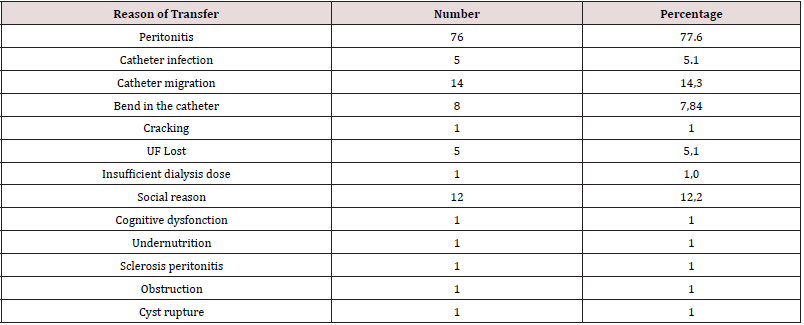
Ninety-eight (98) were included in the study. The mean age at initiation of PD was 45.17 ± 14.09 years. At the time of transfer the mean age was 47.00 ± 13.91 years. There was a female predominance with a sex ratio of 0.66. The initial nephropathy was undetermined in 29.6% of cases. Nephroangiosclerosis and chronic glomerulonephritis of undetermined origin accounted for 28.6% and 15.3% respectively (Table 1). Forty-nine (49) patients received hemodialysis before access to PD. At the initiation of PD, high blood pressure was the most common medical history (94.90%), followed by diabetes and a history of cardiovascular disease (8.16%). The mean Charlson’s index was 2.88 ± 1.31. The mean distance traveled to reach the PD unit was 68.62 ± 104.61 km. The mean length of stay in PD was 19.94 ± 17.25 months. Seventy-two (72) patients were transferred during the first two years of PD. The majority of patients had infectious complications (92.85%) (Table 2) and 59.18% of cases had mechanical complications (Table 3). The main reason for transfer was infection (82.7%), followed by mechanical causes (23.5%) and social reasons (12.2%) (Table 4). There was a statistically significant relationship between infection as a reason for transfer and mortality (p = 0.047). Transfer was program in 9 patients (11.4%). The vascular access at the first haemodialysis session was permanent in 6 patients. Twenty-seven (27) patients had a permanent vascular access after transfer. The mean time to have arterio-venous fistula was 6.46 ± 4.60 months. The mean duration on Haemodialysis was 43.29 ± 44.82 months.
Regarding the outcome, the majority of patients (42.8%) were still in HD, and 34.6% of cases had died. The mean survival according to the Kaplan Meier method was 126.51 ± 11.66 months.
Discussion
At the time of HD transfer, the mean age of transferred patients
was 47.00 ± 13.91 years in our series, while it was 60.0 ± 14.2 years
according to Chen et al. [13], and 68.6 ± 16.8 years according to
Habib et al. [14]. Contrary to what is conventionally described in
the literature, our transferred patients were younger. This can be
explained by the reluctance of elderly patients to change modality,
preferring to stay on PD rather than doing multi-weekly HD sessions.
We can also assume that these older patients are transferred less
frequently, as they die before an HD transfer is necessary. The mean
PD duration was 19.94 ± 17.25 months, and the median was 15.50
months [1.0-90.0]. Habib et al. reported a mean duration of 25.9 ±
23.44 months, [14] and Panagoutsos et al. found a mean of 36 ± 16
months [15]. Ferreira et al. and Szeto et al. found a mean PD duration
of 40.9 ± 26.3 months and 50.9 ± 41.5 months [16,17] respectively.
This disparity between studies is related to the definition of PD
technique failure adopted by each team. In some studies, technique
failure was defined as a 30-day transfer to HD and others defined
it as a transfer of 60 days or more. In the literature, the timing of
transfer from PD to HD depends on the centers and definitions of
the variables. The transfer at 6 months varied between 7% and
25%, while at 1 year it was between 21 and 44%. Eighty-eleven
(91) patients developed infectious complications during their PD
stay. The mean of infectious episodes was 3.36 episodes [1]. Eightynine
(89) patients had peritoneal infections (97.80%). The mean
time to onset of the first episode of peritoneal infection was 9.73
+/- 11.51 months [1]. In France in Le Maner’s series, 53.62% of
patients transferred after 6 months of PD had presented one or
more episodes of peritonitis [18]. While in the Béchade series,
2.60% of patients transferred early (during the first 6 months)
had peritoneal infections [19]. In Australia, Lan et al. found that
50% of cases had peritoneal infections [4]. The occurrence of
peritoneal infection within the first 6 months is considered a risk
factor for transfer from PD to HD. This is explained by the structural
modifications of the peritoneal membrane, which will result in the
failure of the technique.
The high rate of peritoneal infections in our study may be
related to the tropical climate. The heat and humidity promote the
loosening of the dressings and the proliferation of germs. Several
teams, in Australia and Hong Kong, have shown that the rates of peritoneal infections vary with the seasons, and increase with
temperature and humidity [20]. The main reason for transfer was
infection, 76 (77.6%) patients were transferred due to peritoneal
infection. In second place come the mechanical causes in 23.5% of
the patients, and the social reasons come in third place in 12.2% of
the cases then the inadequate dialysis in 6.1% of the cases. Severe
undernutrition and sclerosis peritonitis accounted for only 1%
each. Szeto et al. found that 71.1% of patients were transferred
following peritoneal infection and catheter ablation while 28.9%
of transfers were due to loss of UF and other medical causes [17].
In Panagoutsos’s serie , the causes of transfer were peritoneal
infections (61%), loss of UF (27%), sclerosis peritonitis (9%) and
social reasons (3%) [21]. The mean duration on haemodialysis in
53 patients was 43.29 ± 44.82 months. The majority of patients
(42.8%) were still in HD, 34.6% of cases had died and one patient
was transplanted (1%). According to Le Maner, 73 patients (62.4%)
had died, 22 patients (18.8%) were transplanted, and 22 patients
(18.8%) were still on hemodialysis [18]. In Szeto’s serie, 61.4% of
patients had died, 18.3% were transplanted, 4.6% were transferred
to another center and 15.7% were still in HD [17]. Thirty-four
(34.6%) patients had died. Eight (61.5%) patients had died during
the first 12 months of the transfer. Patient survival according to the
Kaplan Meier method was on average 126.51 ± 11.66 months, and
the median was 152 months. The 5-year survival was 77%. Szeto et
al. found a 5-year survival of 39.9%. They also noted that mortality
was high during the first 12 months. Analysis of survival in patients
who remained alive after 12 first months showed a rate of 65.2%
[17]. According to Habib et al. the mean survival was 79.2 months,
and the median was 90 months [14]. While in Van Biesen’s serie,
the median survival was 95.7 months [22].
Conclusion
The main reasons for transferring PD to haemodialysis identified in the literature are found in our context. This transfer must be anticipated to reduce morbidity and mortality.
References
- Jain AK, Blake P, Cordy P, Garg AX (2012) Global trends in rates of peritoneal dialysis. J Am Soc Nephrol 23(3): 533-544.
- Termorshuizen F, Korevaar JC, Dekker FW, Van Manen JG, Boeschoten EW, et al. (2003) Netherlands Cooperative Study on the Adequacy of Dialysis Study Group. Hemodialysis and peritoneal dialysis: comparison of adjusted mortality rates according to the duration of dialysis: analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis 2. J Am Soc Nephrol 14(11): 2851-2860.
- Liem YS, Wong JB, Hunnik MGM, De Charro FT, Winkelmayer WC (2007) Comparison of hemodialysis and peritoneal dialysis survival in The Netherlands. Kidney Int 71(2): 153-158.
- Lan PG, Clayton PA, Saunders J, Polkinghorne KR, Snelling PL (2015) Predictors and outcomes of transfers from peritoneal dialysis to hemodialysis. Perit Dial Int 35(3): 306-315.
- McDonald S, Hurst K (2011) 34th Annual ANZDATA Report.
- Chiarelli G, Beaulieu M, Cozzolino M, Singh S, Kiaii M, et al. (2008) Vascular access planning in peritoneal dialysis patients. Perit Dial Int 28(6): 585-590.
- Ayav C, Le Maner O, Frimat L, Peters N, Cridlig J (2017) Factors associated with late transfer, beyond six months, from peritoneal dialysis to hemodialysis in a cohort of patients with renal insufficiency receiving dialysis. Rev Epidemiol Sante Publique 65: S55.
- Guo A, Mujais S (2003) Patient and technique survival on peri¬toneal dialysis in the United States: evaluation in large incident cohorts. Kidney Int Suppl 88: S3-12.
- Descoeudres B, Koller MT, Garzoni D, Wolff T, Steiger J, et al. (2008) Contribution of early failure to outcome on peritoneal dialysis. Perit Dial Int 28(3): 259-267.
- Mujais S, Story K (2006) Peritoneal dialysis in the US: evaluation of outcomes in contemporary cohorts. Kidney Int Suppl 103: S21-26.
- Chidambaram M, Bargman JM, Quinn RR, Austin PC, Hux JE, et al. (2011) Patient and physician predictors of peritoneal dialysis technique failure: a population based, retrospective cohort study. Perit Dial Int 31(5): 565-573.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5): 373‑3
- Chen JH, Johnson DW, Hawley C, Boudville N, Lim WH (2018) Association between causes of peritoneal dialysis technique failure and all-cause mortality. Sci Rep 8(1): 1-10.
- Habib A, Anne Claire D, Sambuc R (2020) Switching between Dialysis Modality: A Descriptive Study in Provence-Alpes-Côte D'azur. Ann Nephrol 5(1): 60-70.
- Panagoutsos S, Kantartzi K, Passadakis P, Yannatos E, Theodoridis M, et al. (2006) Timely Transfer of Peritoneal Dialysis Patients to Hemodialysis Improves Sur-vival Rates. Clin Nephrol 65(1): 43-47.
- Ferreira H, Nunes A, Oliveira A, Beco A, Santos J, et al. (2018) Planning Vascular Access in Peritoneal Dialysis Defining High-Risk Patients. Perit Dial Int 38(4): 271-277.
- Szeto CC, Kwan BCH, Chow KM, Pang WF, Kwong VWK, et al. (2010) Outcome of hemodialysis patients who had failed peritoneal dialysis. Nephron Clin Pract 116(4): c300-c306.
- Le Maner O (2016) Study of the predictors of late transfer from peritoneal dialysis to hemodialysis. Example of Lorraine from 2001 to 2010. Thèse med Université de lorraine hal-01947111.
- B chade C (2017) Study of the care pathway for patients with chronic renal insufficiency: ways of optimizing the transition phases. Thèse med Normandie Université tel-01593460.
- Cho Y, Badve SV, Hawley CM, McDonald SP, Brown FG, et al. (2013) Effects of Climatic Region on Peritonitis Risk, Microbiology, Treatment, and Outcomes: a Multicenter Registry Study. Perit Dial Int 33(1): 75-85.
- Grenêche, Sylvie, D'Andon, Anne, Jacquelinet, Christian et al. (2005) The choice between peritoneal dialysis and hemodialysis: a critical review of the literature. Néphrol Ther 1(4): 213-220.
- Van Biesen W, Vanholder RC, Veys NIC, Dhondt A, Lameire NH (2000) An evaluation of an integrative care approach for end-stage renal disease patients. J Am Soc Nephrol 11(1): 116-125.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...