Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Rate of Urinary Complications with Robotic Prostatectomy Surgery: Trial without Catheter 7 versus 10 days Volume 2 - Issue 4
David Caddick1* and Vijay Ramani2
- 1Surgical Advanced Nurse Practitioner, Christie NHS Hospital Foundation Trust, England
- 2Consultant Urology, Christie NHS Hospital Foundation Trust, England
Received: January 25, 2020; Published: February 04, 2020
Corresponding author: David Caddick, Dip Nursing (adult), MSc. Surgical Advanced Nurse Practitioner, Christie NHS Hospital Foundation Trust, Wilmslow Road, Manchester, England
DOI: 10.32474/JUNS.2020.02.000144
Abstract
Research question: Does reducing the time between the Robotic Assisted Laparoscopic Prostatectomy (RALP) operation date and the removal of the urinary catheter have any effect on the rate of urine infection, acute urinary retention, haematuria or dysuria.
Research problem: This study seeks to compare two groups of RALP patients, one with the urinary catheter in situ for 10 days and one group with the catheter in situ for 7 days. The reduction in the time to remove the catheter may have an impact on the frequency of various catheter associated problems including haematuria, rates of urinary infection, dysuria and acute urinary retention and this study seeks to investigate any differences between these groups.
Literature Review: Robotic Assisted Laparoscopic Prostatectomy (RALP) surgery has been increasingly popular over conventional laparoscopic or open prostatectomy due to the suggested reduction in complications and improved recovery time [1-4]. The potential reductions have obvious benefits for reducing length of stay and therefore cost. Although this is offset with larger capital expenditure for the Robot device themselves as well as the maintenance and purchase of the per-patient equipment [5-7] however suggest a more mixed picture in terms of outcomes between laparoscopic and robotic surgery and in fact more complications laparoscopically, such as erectile dysfunction and incontinence but less transfusions and respiratory complications. They do not however distinguish between the robotic and the non-robotic cases, which confuses the picture.
During the procedure a catheter is inserted preoperatively to maintain the bladder patency after the prostate is removed [8- 10] and stays in situ till removed at a later date to give the anastomotic join at the bladder neck time to heal, become patent and therefore water tight.
Time to trial without catheter (TWOC) lengths vary across intuitions from as short as 2 days to as long as 14 with the most frequent duration to be at around 7 days [11;12;8;10;13;15].
At our institution, a large Cancer hospital in the UK, TWOC duration (the time between the operation date and the TWOC date) historically has been 10 days post-operative for RALP patients and had relatively low complication rates at this duration. The TWOC duration was suggested to be reduced from 10 days to 7 as many patients find the catheters uncomfortable and therefore the less time, they are in situ the better the patient experience. In fact, there is evidence that the patency of the anastomosis is secured within a few days. [15] showed that by day 3 or 4 only 3 out of 381 patients showed a leak on cystogram (0.8%). Therefore, the TWOC duration was decreased from 10 to 7 days to improve patient experience and to bring us in line with other centres. There were concerns that changing the TWOC duration would have a deleterious effect on the patients. It was suggested that this could affecting the risk of urinary infection (UTI), the rates of dysuria, acute retention of urine (AUR) and haematuria after the catheter is removed.
Catheters are associated with an increased risk of infection (UTI) which occurs very soon after insertion. Indeed, it is suggested that this happens in nearly all patients who are catheterised long term (28 days) and up to 50% of short term catheterisations (<7 days) are found to been colonised [16]. A Cochrane review (Phipps et al, 2006) has shown that the shorter the duration of the catheter being in situ, the less UTI risk there was. A shorter TWOC duration should reduce the rate of urine infections seen.
Dysuria can become an issue when the catheter is present [17] this is likely due to the bladder losing tone. In fact using flip flow valves rather than catheter bags improves the likelihood of successful voiding after the catheter is removed in one study from 63% to 83% [18] which suggests that bladders which lose the filling and emptying function even for a short time tend to have more problems returning to a normal function. However flip flow values are not indicated in RALP surgery as there needs to be little or no bladder pressure from urine filling the bladder putting strain on the bladder neck anastomosis. [17] highlighted that just the existence of an indwelling catheter is associated with increased dysuria. The less time the catheter is in situ, it seems a reasonable to suggest that dysuria rates should also improve.
Retention of urine after removing the catheter post RALP is also a concern, although rare [15]. There is some evidence to suggest that longer catheter durations improve the rates of retention. In the study by [11] 740 patients were stratified into a TWOC at day 4 and day 7. They found that acute retention was significantly higher (p=0.004) at day 4 (4.5%) than day 7 (0.2%). Another study of 1026 patient by [15] spilt RALP patients into groups with or without acute urinary retention. The duration the catheter was in situ was shorter for the retention group at 4.1 days than the non-retention group at 5.7, suggesting that slight increases in TWOC duration should reduce the incidence of retention. This may be related to the increased surgical oedema in the immediacy of the surgery which improves over time. It appears that longer TWOC durations in some situations may reduce the rates of urinary retention.
Although multiple studies have shown that laparoscopic prostatectomy surgery causes much less blood loss compared to open surgery. In fact, Robotic surgery in particular is consistently lowest in blood loss volumes [19,20]. Some haematuria is expected in the case of RALP patients as result of surgery, catheters themselves by abutting and irritating the delicate mucosa of the urethra can cause haematuria [21]. Therefore, it seems likely that having a catheter in place for less time should reduce the likely hood of trauma and bleeding, however this may be offset by the post op bleeding expected from the RALP procedure itself. In other words, TWOC too early and haematuria may be related to the operation itself, whereas too late and it may be attributable to the catheter. This will be difficult to test which is the cause for this study however this study will also investigate any changes in rates of haematuria.
This study was designed to measure and identify if reducing the TWOC duration from 10 days to 7 days had any effect on the incidence of UTI, dysuria, haematuria and AUR.
Introduction
This was prospective quantitative study of 257 RALP patients
over a period of time of 2 years from 2017 to 2019. Patients were
first identified using Theatreman software to identify all patients
who had a RALP procedure. CWP (Clinical Web Portal) was used to
identify patient information electronically. Culture and sensitivity
data were extracted for pre-operative and post TWOC urine
samples. Urinary infections were controlled (for example likely
skin contamination) in both the preoperative UTI and the post
TWOC UTI groups. A likely contaminant such as skin flora was
not included in the results as true urinary infection. Post TWOC
urine cultures which matched the preoperative and controlled
urine culture were also discounted as true new urinary infection.
This was to ensure that only the new infections were counted, and
ongoing urinary infections were not counted as falsely positive and
skewing the data.
Specialist nursing staff called each patient several weeks after
the catheter is removed to check the status of the patient and this
was recorded on Patient records (CWP). These were used to identify
with in each patient record any mention of problems relating to
haematuria, acute retention or requiring a catheter inserted after
the TWOC or dysuria of any sort. Any mention these would score
either a one or if there was no mention or explicitly excluded would
score a zero.
Patients were excluded if there were incomplete data points
for any fields. This resulted in exclusions of 24 data points due to
incomplete data and 3 dues to having TWOC duration of 14 days.
This left 257 patients (146 patients in the 10-day TWOC group,
111 patients in the 7-day TWOC group). Patients were allocated
to the two groups at surgeon’s choice. Data was anonymised so
that patient identifiable information remained confidential and
therefore consent was not required.
Patient specific data was collected and as already reported only
those patients with a full data set were included in the data set.
UTI status both preoperatively and post catheter removal (TWOC)
were recorded from culture and sensitivity data. The date of TWOC
compared to date of operation and the duration on the catheter
insertion post RALP was calculated to be either day 10 or day 7.
CWP was used to identify any discussion or record about any issues
or lack thereof of dysuria, haematuria or urinary retention after the
first TWOC. This was done with post discharge telephone contact
of the patient by specialist nurse service as part of routine follow
up practice.
Results
There were 256 patients with recorded data in the project, 3
of which were excluded due to having 14 days TWOC and 24 were
excluded due to incomplete data. The table 1 includes the results
of the chi-square tests (or Fisher’s exact test) for UTI pre, UTI post,
retention, haematuria and dysuria. UTI post is only recorded as
positive if the recorded ‘C+S’ is different to the ‘C+S’ value for UTI
pre.
It appears that there is a statistically significant difference in
the proportion of UTIs at the start of the TWOC period between the
groups, with the 7 days group having a higher proportion of UTIs.
This is something to consider in the other analyses as there was a
baseline difference in UTIs.
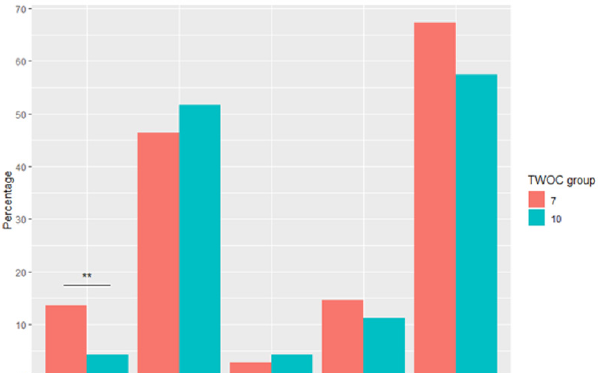
Table 1: Chi squared test data.

Fisher’s exact test.
Note: Fisher’s exact test is a small samples equivalent to the chi-square test.
There was no statistically significant difference between the 7
days and 10 days groups for UTIs at the end of the TWOC period,
incidence of retention, haematuria nor dysuria (see Table 1).
There appears to be small differences (see Graph 1) between the
groups for UTI post, retention and haematuria (all differences are
less than or equal to 5.3%). However, despite the non-statistically
significant result for dysuria, there being 10% more patients with
dysuria (67% vs 57%) in the 7 days group compared to the 10 days
group is a potential concern.
Limitations
Patients were not randomly allocated to the day 7 or day 10 TWOC groups as the consultants allocated the TWOC duration on the day of surgery. No demographic data was collected which mean that homogeneity comparisons between groups could not be done. There reasonable number proportion of patients that were excluded du to having incomplete data sets. This worked out at 6.8% exclusion rate which is not insignificant. All the data points were from patients in a tertiary centre, which means the conclusions may not necessarily to extrapolate to the district general population. Furthermore, these were Robotic Prostatectomy patients and the conclusions should not generalise to laparoscopic or open prostatectomy surgery.
Discussion
There were no statistical differences in terms of UTI risk,
dysuria, haematuria and episodes of acute urinary retention. There
were however minor differences in numbers between the two
groups. Rates of haematuria and dysuria were increased, whereas
rates of urinary infection and retention decreased.
Rates of haematuria increasing post operatively may be a
reflection of the healing anastomosis being slightly more friable
after the catheter is removed at day 7 compared to day 10. However,
a small non-significant elevation 3.2% means that there is no
difference between the groups. Reducing the TWOC duration does
not appear to significantly affect the rate of haematuria.
Rates of dysuria somewhat unexpectedly also increased with a
reduction of the TWOC period by a larger (10.0%) but again this
was not statistically significant. The longer the catheter is in situ
the more likely that the bladder has reduced tone and more likely
to suffer problems with dysuria. These data do show a rather
paradoxical picture. This may be a reflection of the bladder being
more irritable at day 7 than day 10 however since the results are
not statistically significant, it is difficult to draw any conclusions.
Reducing the TWOC duration does not appear to significantly affect
the rate of dysuria.
Retention of urine had an overall small number in both the
groups. However, the small reduction in retention rates may be
a reflection of the decreased bladder tone in the day 10 group
compared to the day 7 group. The difference was small at 1.5% and
again not statically significant so it appears that TWOC duration
does not appear to significantly affect the rate of urinary retention.
A reduction in the frequency of UTIs were seen when the
TWOC duration was reduced to 7 days (5.7%), however this was
not statistically significant. This reduction in UTI incidence may
reflect the reduced time that bacteria have to colonise the catheter
resulting in fewer UTIs post RALP in the day 7 group. However, given
the non-statistical significance we can only state that reducing the
TWOC duration does not appear to significantly affect the rate of
incidence of UTI.
Interestingly the only statistically significant difference
between groups was between the pre-operative UTI rates which
were significantly higher for the day 7 group compared to the day 10
group. However, since this was prior to any medical interventions at
that point it difficult to see why there should be any difference here
and is likely to be of indeterminate significance since the duration
of the TWOC is decided usually after the operation.
This study has clearly demonstrated that reducing TWOC
duration post RALP, does not statistically affect the rates of UTI,
retention, haematuria or dysuria. Reducing the duration of the
TWOC however is likely to improve the patient comfort and
experience. It is therefore a safe clinical practice for this cohort of
patients.
References
- Cao L, Yang Z, Qi L, Chen M (2019) Robot-assisted and laparoscopic vs open radical prostatectomy in clinically localized prostate cancer: perioperative, functional, and oncological outcomes: A Systematic review and meta-analysis. Medicine 98(22): e15770.
- Patel VR, Chammas Jr MF, Shah S (2007) Robotic assisted laparoscopic radical prostatectomy: a review of the current state of affairs. International journal of clinical practice 61(2): 309-314.
- Park JW, Won Lee H, Kim W, Jeong BC, Jeon SS (2011) Comparative assessment of a single surgeon's series of laparoscopic radical prostatectomy: conventional versus robot assisted. Journal of endourology 25(4):597-602.
- Yaxley JW, Coughlin GD, Chambers SK, Occhipinti S, Samaratunga H (2016) Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. The Lancet 388(10049): 1057-1066.
- Bolenz C, Gupta A, Hotze T, Ho R, Cadeddu JA (2010) Cost comparison of robotic, laparoscopic, and open radical prostatectomy for prostate cancer. European urology 57(3): 453-458.
- Murphy DG, Bjartell A, Ficarra V, Graefen M, Haese A (2010) Downsides of robot-assisted laparoscopic radical prostatectomy: limitations and complications. European urology 57(5): 735-746.
- Hu JC, Gu X, Lipsitz SR, Barry MJ, D’Amico AV (2009) Comparative effectiveness of minimally invasive vs opens radical prostatectomy. Jama 302(14): 1557-1564.
- Carlucci JR, Nabizada-Pace F, Samadi DB (2009) Robot-assisted laparoscopic radical prostatectomy: technique and outcomes of 700 cases. International journal of biomedical science: IJBS 5(3): 201-208.
- Gettman MT, Hoznek A, Salomon L, Katz R, Borkowski T (2003) Laparoscopic radical prostatectomy: description of the extraperitoneal approach using the da Vinci robotic system. The Journal of urology 170(2): 416-419.
- Huynh LM, Ahlering TE (2018) Robot-Assisted Radical Prostatectomy: A Step-by-Step Guide. Journal of endourology 32(S1): S28-S32.
- Alnazari M, Zanaty M, Ajib K, El-Hakim A, Zorn KC (2018) The risk of urinary retention following robot-assisted radical prostatectomy and its impact on early continence outcomes. Canadian Urological Association Journal 12(3): E121-E125.
- Cadeddu JA (2019) Re: Removing the Urinary Catheter on Post-Operative Day 2 after Robot-Assisted Laparoscopic Radical Prostatectomy: A Feasibility Study from a Single High-Volume Referral Centre. The Journal of Urology 201(4): 648.
- Menon M, Tewari A, Baize B, Guillonneau B, Vallancien G (2002) Prospective comparison of radical retropubic prostatectomy and robot-assisted anatomic prostatectomy: the Vattikuti Urology Institute experience. Urology 60(5): 864-868.
- Yasui T, Tozawa K, Okada A, Kurokawa S, Kubota H (2014) Outcomes of robot-assisted laparoscopic prostatectomy with a posterior approach to the seminal vesicle in 300 patients. International scholarly research notices.
- Khemees, TA, Novak, R,Abaza R (2013) Prospective comparison of radical retropubic prostatectomy and robot-assisted anatomic prostatectomy: The Vattikuti Urology Institute experience. Adult urology189(4): 1432-1436.
- Donlan RM (2001) Biofilms and device-associated infections. Emerging infectious diseases 7(2):277-281.
- Michels TC, Sands JE, Sands JE (2015) Dysuria: Evaluation and Differential Diagnosis in Adults. American family physician 92(9): 778-786.
- Virdi G, Hendry D (2015) Urinary Retention: Catheter Drainage Bag or Catheter Valve? Current urology 9(1): 28-30.
- Banapour P, Patel N, Kane CJ, Cohen SA, Parsons JK (2014) Robotic-assisted simple prostatectomy: a systematic review and report of a single institution case series. Prostate cancer and prostatic diseases17(1): 1-5.
- Finkelstein J, Eckersberger E, Sadri H, Taneja SS, Lepor H (2010) Open versus laparoscopic versus robot-assisted laparoscopic prostatectomy: the European and US experience. Reviews in urology 12(1): 35-43.
- Robinson J (2004) A practical approach to catheter-associated problems. Nursing Standard 18(31): 38-42.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...