Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case Report(ISSN: 2641-1687) 
Pre-Operative Diagnose of Inguinal Bladder Hernia: Typical Radiological Findings Volume 2 - Issue 3
Camila R T Burity*, Fábio T Ferreira, Edson S Bezerra, Dorival M Duarte, Euclides J Nunes and Ricardo D Saade
- dr. Mário Gatti Municipal Hospital, Campinas, Brazil
Received: November 20, 2019; Published: November 25, 2019
Corresponding author: Camila R T Burity, Rua Artur Ramos, 558, Campinas, SP, Brazil
DOI: 10.32474/JUNS.2019.02.000139
Abstract
A sliding hernia occurs when the hernia sac is partially formed by the wall of an abdominal organ, as sigmoid colon, appendix, cecum, and urinary bladder. The presence of bladder is rare, occurring in less than 4% of the cases. This case series shows typical radiology findings in three men with bladder inguinal hernia and how the pre-operative diagnoses can prevent complications.
Keywords: Inguinal hernia; Bladder; Cystography
Introduction
A sliding hernia occurs when the hernia sac is partially formed by the wall of an abdominal organ, as sigmoid colon, appendix, cecum, and urinary bladder [1]. First described by Levine [2] in 1951, an inguinal bladder hernia is a rare event between the abdominal wall defects, occurring in less than 4% of the cases [3]. Clinical presentation is variable and can include inguinal swelling, low tract urinary symptoms (LUTS), pain, and the need for inguinal compression when voiding [3]. This case series shows typical radiology findings in three men with bladder inguinal hernia followed in this service.
Cases Presentation
Case 1
Figure 1: A -right inguinoscrotal hernia / B- Retrograde cystogram showing dumbbell-shaped urinary bladder in a sliding inguinal hernia/ C- Contrast cystography after hernia repair.

A 58 years-old man with right inguinal hernia surgical repair schedule was referred to urology for LUTS investigation. During clinical history, the IPSS showed a severe score with a predominance of voiding symptoms. He denies comorbidities or previous surgeries. Physical examination revealed a right inguinoscrotal hernia (Figure 1A) and a prostate of 30g in the digital rectal exam. He was treated with doxazosin 4mg/day, without success. A retrograde cystogram was requested (Figure 1B), and it exhibited a bladder herniation with a dumbbell shape (Figure 1C). Based on this result, an inguinal hernia repair with the Liechtenstein technique was performed with complete remission of urinary symptoms.
Case 2
Figure 2: A and B- cystography indicating the prolapse of urinary bladder/ C- Abdominal CT showing the inguinal bladder hernia -coronal view and D- sagittal view.
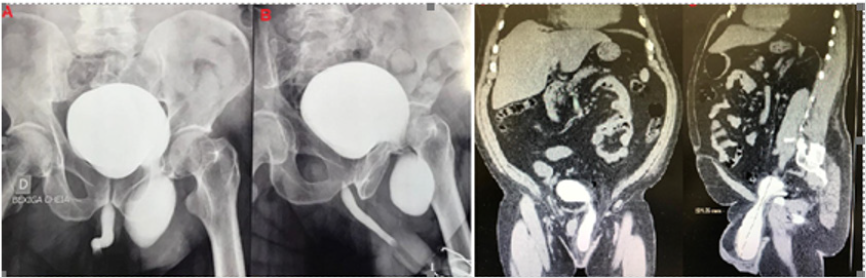
A 70 years-old man, obese, hypertensive, diabetic, complaining of inguinal swelling and urinary symptoms for three years, sought the urologist. Previous surgeries include a right inguinal hernioplasty and a transurethral resection of the prostate. Among the signs, the need for inguinal compression for complete bladder emptying stood out. Physical examination presented a significant irreducible left inguinal bulging and a prostate of 40g. Retrograde urethrocystography (Figure 2A) revealed a sizeable secular image projected on the left inguinal region; confirmed the diagnoses with computerized tomography (CT), measuring 8.3 x 5.2cm (Figure 2B). An open repair using the Lichtenstein technique was done (Figure 2C), with remission of voiding symptoms (Figure 2D).
Case 3
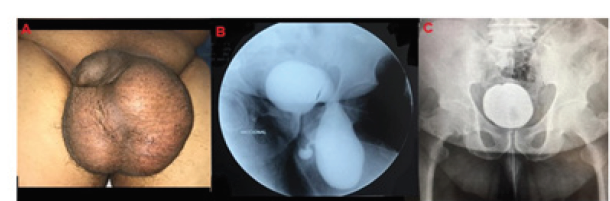
A 57-years-old man complaining of testicular enlargement associated with voiding dysfunction. He reports the need for groin compression for complete emptying. He denies previous surgery or other comorbidities. Physical examination showed fluid in the left scrotum (Figure 3A). Cystogram pointed a bladder protrusion in the left inguinal canal with a refluxing ureter present in the hernial sac (Figure 3B). An open repair was done with excellent results (Figure 3C). Cystogram control showing a bladder with high capacity and no more herniation.
Figure 3: A- left inguinal hernia with fluid in scrotum/ B- urethrocystography illustrating the protrusion of the bladder in the left side and a refluxing ureter C- cystogram after inguinal repair.
Discussion
Bladder hernia is a rare disease frequently appearing in mid-age males that should be suspected in every patient with obstructive urinary symptoms and inguinal swelling. Fewer than 7% of bladder hernias are discovered before surgery [4], which increases the risk of inadvertent intraoperative injuries. Between the possible radiological exams, we highlight the cystography and CT-scan. In cystograms, the typical images are described as dumbbell or dogear shape of the bladder [5,6], as observed in these three cases. It is an easily interpretable test that should be requested in case of diagnostic doubt or presence of scrotum fluid on ultrasound. CT can add invaluable information during the pre-operative planning of these patients, like the size, position, and contents of the hernial sac, beyond identify associated pathologies or complications such as hydronephrosis or strangulation [7]. If it has done with contrast, as in case 2, the bladder content in the hernia is better demonstrated.
Conclusion
Bladder hernia is a pathology that should be reminded in every male patient with obstructive symptoms and associated inguinal hernia. Retrograde and voiding cystourethrogram and Computerized Tomography are two of the possible radiological diagnostic tests in these cases. Preoperative diagnosis improves the therapeutic approach and prevents complications.
References
- AlMohaya N, Marwah Nasser EA, Khalid AlAnazi, Ahmed Mohammed AM,Hesham Eltomy (2019) Bilateral inguinal bladder hernia following unilateral transabdominal preperitoneal repair. A case report and review of the literature. Ann Med Surg (Lond) 46: 23-26.
- Levine B (1951) Scrotal cystocele. JAMA147(15):1439-1441.
- Branchu B, Renard Y, Larre S, Leon P (2018) Diagnosis and treatment of inguinal hernia of the bladder: a systematic review of the past 10 years. Turk J Urol44(5):384-388.
- GonzalezUrquijo M, MayagoitiaGonzalez JC, RodarteShade M, BermeaMendoza JH, GilGalindo G (2019) Large inguinal bladder hérnias: can a preoperative diagnosis be made? Hernia.
- Malhotra MK, Kapoor Y (2012) Pre surgical evaluation of scrotal cystocele by conventional radiography (cystogram). Niger J Surg18(1):34-36.
- Mahadevappa B, Suresh SC, Natarajan K, Thomas J (2009) Cystogram with dumbbell shaped urinary bladder in a sliding inguinal hernia. J Radiol Case Rep3(2):7-9.
- Khan A, Beckley I, Dobbins B, Rogawski KM (2014) Laparoscopic repair of massive inguinal hernia containing the urinary bladder. Urol Ann6(2):159-162.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...