Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Opening of New Hemodialysis Centers in Countries with Limited Resources: Experience at 04 Years of The Ziguinchor Hemodialysis Unit in Southern Senegal Volume 4 - Issue 2
Kane Yaya1*, BA Mamadou Aw1, Kaya K Mukonkole1, Mboup Ndiaye Ousmane1, Mah Sidi Mohamed5, Keita Niakhalen2, Diagne Seynabou2, Dieng Ameth2, Mbengue Mansour2, BA Bacary2, Faye Moustapha2, Koulibaly CA Tidiane2, Achref BH Younes2, Faye Maria2, Lemrabott A Tall2, Cisse M Moustapha4, Seck S Mohamed3, KA El Fary2, Niang Abdou2, Diouf Boucar2
- 1Nephrology and hemodialysis service at the Peace Hospital/CHRZ/Assane Seck Ziguinchor University, Senegal, West Africa
- 2HALD nephrology hemodialysis Department, Dalal Diam, Pikine/UCAD Dakar, Senegal, West Africa
- 3Nephrology and hemodialysis service CHR of St Louis Gaston Berger University, Senegal, West Africa
- 4Nephrology hemodialysis department CHR of Thiès / University of Thiès, Senegal, West Africa
- 5Hemodialysis Nephrology Department / Nouakchott General Hospital, Mauritania, West Africa
Received: March 03, 2023; Published: March 09, 2023
Corresponding author: Kane Yaya, Nephrology and hemodialysis service at the Peace Hospital/CHRZ/Assane Seck Ziguinchor University, Senegal, West Africa
DOI: 10.32474/JUNS.2023.04.000184
Abstract
Introduction: Kidney failure is a common affection and replacement therapy is not always accessible in sub-Saharan Africa. the aim of our study was to evaluate the management of acute and chronic hemodialysis patients at the Ziguinchor hemodialysis unit in southern Senegal after 04 years of activity.
Patients and Methods: This was a descriptive and analytical retrospective study extending from January 1, 2015, to December 31, 2018. The data studied were epidemiological, clinical, par clinical and evolutionary.
Results: One hundred and forty-six (146) patients were included in the study. Seventy-six (76) patients had benefited from dialysis in the context of an ARI (52.05%) and 70 chronic hemodialysis patients (47.95%). The causes of ARI were dominated by infectious causes in 46 cases (60.5%). the evolution of the ARI was favorable, under hemodialysis in 61 cases (80.3%). we deplored 15 deaths (19.7%) in ARI. Regarding CKD patients, the average duration in hemodialysis was 24.13 months. The first hemodialysis session was performed on a central venous catheter in 57 patients (81.4%). The average hemoglobin level was 7 g/dl. Thirtyseven deaths were recorded among IRCs, i.e., 52.9%. There was a significant relationship between taking herbal medicine and the occurrence of ARI (p=0.0001), the vascular access route and the duration of hemodialysis (p=0.0001) in CRI.
Conclusion: The decentralization of hemodialysis centers in the regions of the country has reduced the morbidity and mortality of renal failure in Senegal.
Keywords: Hemodialysis; ziguinchor; Senegal
Introduction
Kidney failure is a major public health problem whether acute or chronic. It is estimated that 2 to 7 million people suffering from renal failure worldwide die prematurely due to lack of access to renal replacement therapy (dialysis or renal transplantation) [1]. The number of people who were on this replacement therapy exceeded 3 million in 2017 and is expected to reach 5.4 million by 2030 [2]. Many countries in sub-Saharan Africa face a serious problem in terms of economic and human resources for the treatment of patients with chronic end-stage renal disease [3]. Hemodialysis is the most widely used renal replacement technique in these countries, expensive in terms of equipment [4], it remains inaccessible for most patients.
In Senegal, it is one of the major concerns of the government. Since 2012, dialysis sessions have been free in public hospitals for all patients with kidney failure who need dialysis [5]. Several dialysis centers have been opened for this purpose, and that of the Ziguinchor region in December 2014. The objective of our work was to evaluate the management of acute and chronic hemodialysis patients in the hemodialysis unit of the Regional Hospital Center of Ziguinchor (CHRZ) after 4 years of activity.
Patients and Methods
This was a descriptive and analytical retrospective study extending from January 1, 2015, to December 31, 2018. The study took place in the hemodialysis unit of the CHRZ located 450 km from Dakar in the south of the country. Were included in this study, all patients with acute and chronic renal failure who had benefited from hemodialysis sessions since the opening of the center.
For each patient, the following parameters were studied:
a) Epidemiological: age, sex, marital status, profession, geographical origin, type of renal failure, causal nephropathy.
b) Initial management: emergency dialysis, nephrological follow-up before starting dialysis.
c) Hemodialysis: place of first dialysis, duration in dialysis, mode of entry into dialysis, vascular access, number of sessions per week, tolerance of the dialysis session.
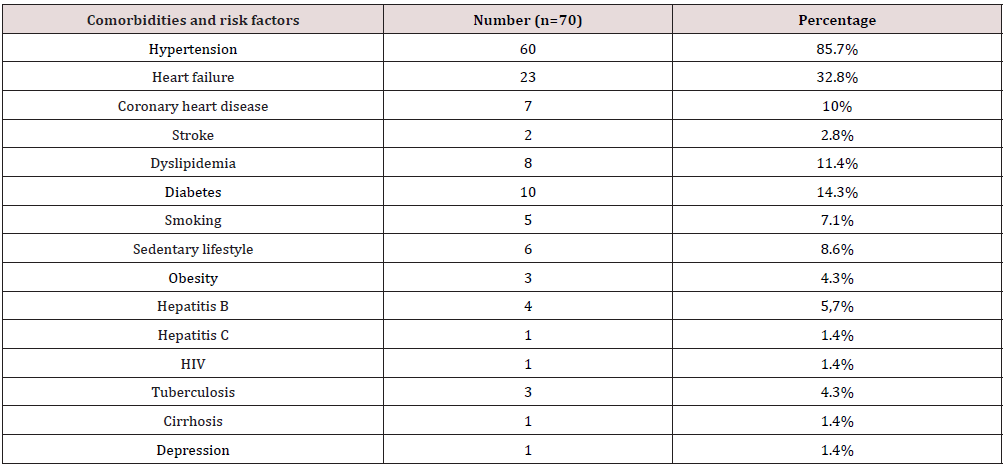
d) Hemoglobin level, phosphocalcic disorders, nutritional status, comorbidities and cardiovascular risk factors: heart failure, stroke, coronary disease, obesity, hepatitis B, HIV, smoking.
e) The causes of acute (AKF) and chronic (CKF) kidney failure.
f) The evolution of AKF and CKF.
Dialysis tolerance was defined by hemodynamic instability (arterial hypotension, arrhythmia) during the dialysis session. The nutritional status of the patients was assessed by the dosage of serum albumin, protein and body mass index. Malnutrition was defined by hypoalbuminemia below 40 g/l, hypoprotidemia below 70 g/l and a body mass index below 18.5 kg/m2. Hemodialysis sessions were free. But the non-nationals, with support at the level of their country, paid for a session at a price ranging from 60,000 to 200,000 CFA francs. Data were entered using Sphinx software version 5.1.0.2 and analyzed using SPSS software version 18. The descriptive study was carried out with the calculation of frequencies and proportions for the qualitative variables and the calculation of the averages and standard deviations for the quantitative variables. The analytical study was made with cross tables. To compare the frequencies, we used Pearson’s Chi-square test or Fisher’s twosided exact test depending on their conditions of applicability, the comparison of the averages was made with the analysis of the variance test with a threshold of significance p < 0.05.
Results
During our study period, 146 were included, of which 76 AKF or 52.05% and 70 CKF or 47.95%.
Concerning AKF patients
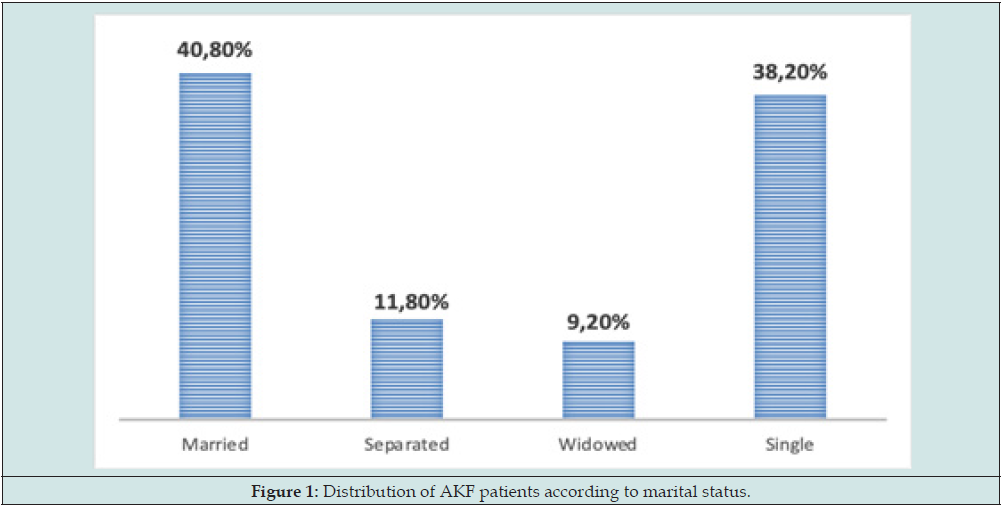
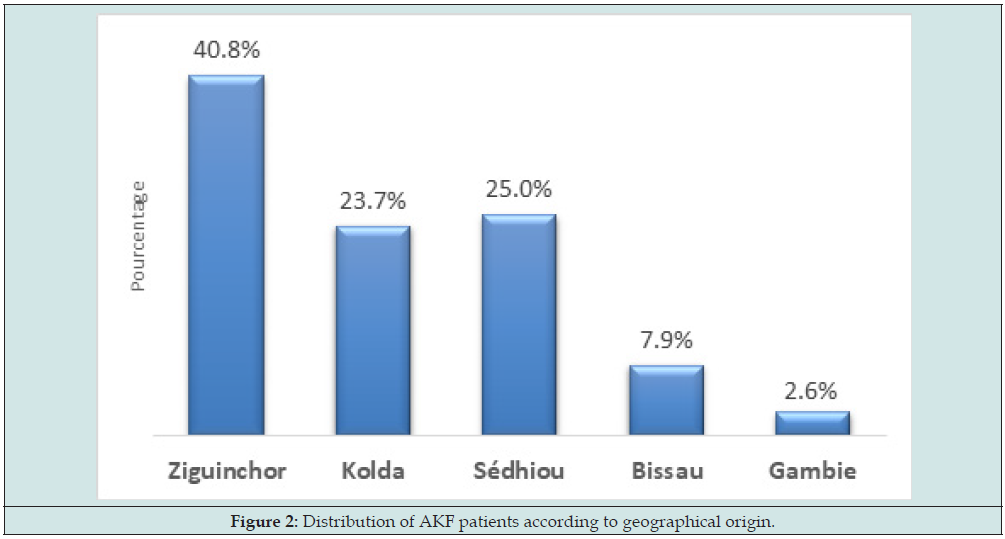
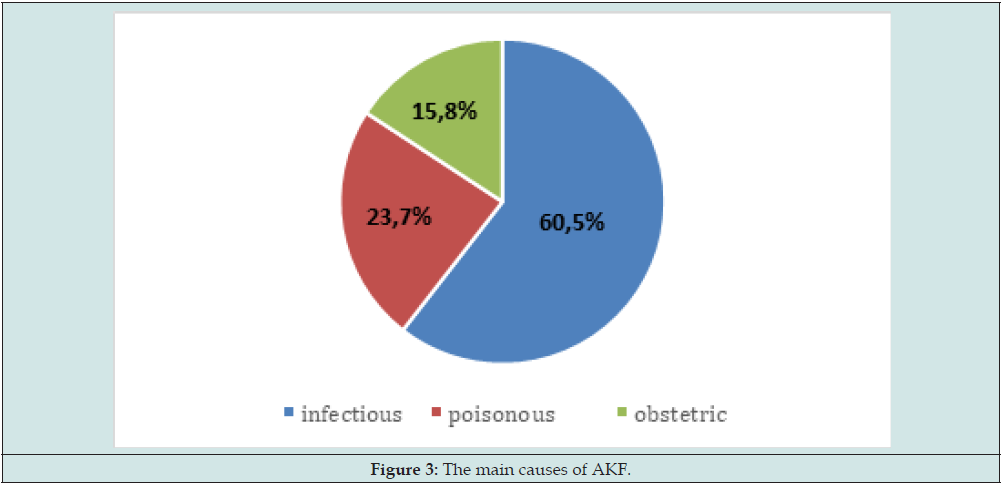
The average age was 39.71 ± 19.62 years with extremes of 7 and 82 years. The most affected age group was between 20 and 29 years old. There were 40 men (52.6%) and 36 women (47.4%) with a sex ratio of 1.11. There were 31 married (40.8%) and 29 single or 38.2% (Figure 1). Thirty-one patients, or 40.8% came from the Ziguinchor region and 19 patients came from Sedhiou or 25% (Figure 2). The majority of AKFs, i.e., 60 patients, had taken oral herbal medicine (78.9%). Among the AKF, 39 patients came from the Reception and Emergency Department (SAU) i.e., 51.3%, 19 from internal medicine i.e., 25%, from intensive care i.e., 17.1% and 5 others from pediatrics, i.e., 6.6%. The causes of AKF were dominated by infections in 46 patients or 60.5% followed by toxic and obstetric causes respectively in 18 and 12 cases i.e., 23.7% and 15.8%. Among the infectious causes, pneumopathy was more common in 29 cases, i.e., 63%, followed by malaria, urinary tract infection and skin infections in 23.9%, 10.9% and 2.2% respectively(Figure 3).
Sixty-six AKF patients tolerated dialysis well, i.e., 86.8%, and 10 patients, i.e., 13.2%, had poor dialysis tolerance. Sixty-nine patients or 90.8% had anemia. The mean hemoglobin level was 7.68 ± 2.29 g/dl with extremes of 4.2 and 13.5 g/dl. The evolution of the AKF was, favorable in 61 patients or 80.3% with a total recovery of the renal function, unfavorable marked by the occurrence of 15 cases of death or 19.7%. Deaths were related, in 10 patients to severe sepsis (66.7%), in 4 patients to multi-organ failure (26.7%) and in 1 patient to acute pulmonary edema (APO) (6.7%). The analytical study had shown that there was a significant relationship between taking herbal medicine and the occurrence of AKF (p=0.0001). Patients who had taken herbal medicine were more likely to develop AKF.
Concerning CKF patients
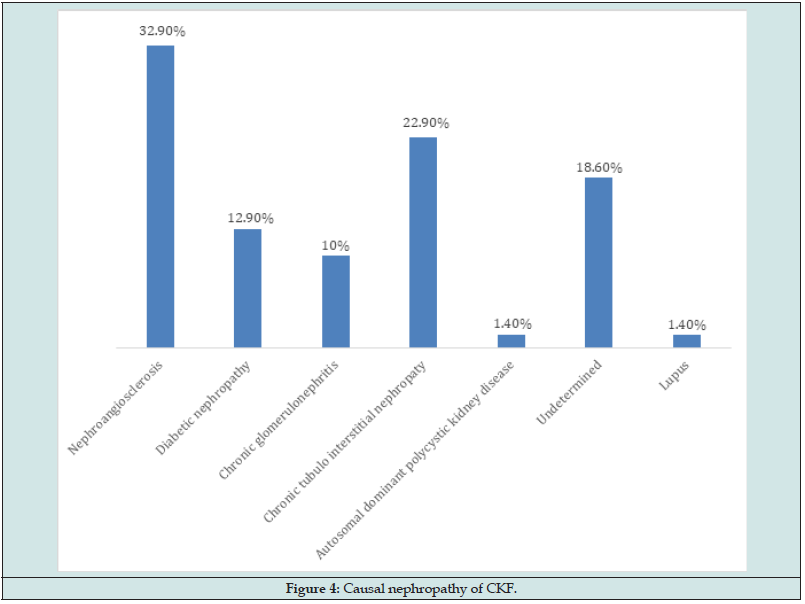
The average age was 41.38 ± 12.89 years with extremes of 10 and 67 years. There were 37 men (52.9%) and 33 women (47.1%) with a sex ratio of 1.12. The causal nephropathy of CKF was dominated by nephroangiosclerosis in 23 patients (32.9%) (Figure 4). Among CKF patients, the majority, 42 (60%) were on emergency dialysis. Only 25 patients (37.5%) had nephrology follow-up before entering dialysis. The first hemodialysis sessions were started in Dakar in 35 patients, i.e., 50%, and in Ziguinchor in 27 patients, i.e., 38.6%. The average duration in hemodialysis of CKF patients was 24.13 ± 21.77 months with extremes of 1 and 125 months. The first hemodialysis session was performed on a central venous catheter in 57 patients, i.e., 81.4%. Twenty-eight patients (40%) were hemodialyzed with AVF and 21 patients (30%) with a tunneled catheter. Forty-eight CKF patients (68.6%) benefited from 3 sessions per week and 22 patients (31.4%) benefited from 2 sessions per week. Sixty-seven CKF patients tolerated their dialysis session, i.e., 95.7%. Twentyseven patients. Fifty-four patients (77.1%) had hypocalcemia, 10 patients (14.3%) had hypophosphatemia and 18 patients (25.7%) hyperphosphatemia.
No patient benefited from an assay of parathyroid hormone (PTH) or vitamin D because it was not available. The mean hemoglobin level was 7.07 ± 1.32 g/dl with extremes of 4.3 and 11 g/dl. Only 23 patients (32.9%) benefited from treatment with an erythropoiesis-stimulating agent. Forty-nine patients (70%) were transfused. Among the CKF patients, 60 (85.7%) were presented with hypertension, 23 (32.8%) with heart failure (Table 1). The evolution of CKF was marked by the occurrence of 37 deaths or 52.9%. Causes of death were dominated by chronic uremia in 14 patients (37.8%), sepsis in 9 patients (24.3%), acute pulmonary edema and myocardial infarction in 6 patients (16.2%). One case of hemorrhage by rupture of AVF and 1 case of catheter malfunction, i.e., 2.7% each, were noted. In our study, there was a significant relationship between the vascular access route and the duration of hemodialysis (p=0.0001). Patients who had permanent access were more likely to have a longer duration on hemodialysis than those who had temporary access.
Discussion
The average age of the patients was 39.7 years. This result is similar to other studies carried out in Africa. Bensalem in Algeria [6] and Mahoungou in Congo Brazzaville [7], had found an average age of 48 years. In France in 2006, the study by Vinsonneau and al showed a higher average age of 65 years [8]. In the Western series, it is between 60 and 80 years against 35 to 45 years in developing countries [9]. The youth of our study population is explained by the relative youth of the African population in general and Senegalese in particular [10]. Nephroangiosclerosis was the main cause of CKF in our study (32.9%). Some studies carried out in Senegal in 2014 in Tambacounda [11], 2016 [12] and 2019 [13] in Dakar, nephroangiosclerosis was also the most frequent initial nephropathy with respectively 52.8%; 56.3% and 58%. This high frequency is also found in Algeria 50% [14] and in Madagascar 33.3% [15]. In our study, hypertension is the first because that leads patients to dialysis. This could be explained by its frequency and severity in African Americans, difficult access to expensive antihypertensive treatments and increased salt consumption. In our study population, 60 patients or 35.7% had nephrology followup before starting dialysis.
The delay in diagnosis largely explains these results, as kidney disease usually progresses asymptomatically. Awareness raising and mass screenings organized on a routine basis will enable the early diagnosis of this scourge, the vital prognosis of which can be threatened in the short term. The first hemodialysis session was performed on central venous catheter in 81.4% of patients. Our results are similar to those of Kane in Tambacounda, Coulibaly in Dakar and Medkouri in Morocco who found 96.6% [16], 86.6% [17] and 83.6% [18] respectively. Regarding chronic kidney disease in developed countries, the approach of the terminal stage requires the making of an arteriovenous fistula. Thus, central venous catheters only concern 2 to 3% of patients [19]. Among the 70 patients who were presented with CKF, we recorded 37 deaths, i.e., 52.9%. This result is higher than those of Ramilitiana and Kane who found 25.6% and 18.6% respectively. Mortality related to chronic kidney disease is mainly due to the delay in diagnosis which subsequently compromises management. The causes of death were dominated by chronic uremia (37.8%). The reduced number of dialysis generators required the performance of 2 hemodialysis sessions in our structure.
Conclusion
In Senegal, although the care of patients with kidney disease has experienced considerable growth, particularly with the opening of dialysis centers in the different regions, access to care is not always easy. The majority of patients are seen at a terminal stage and the prognosis is often life-threatening. Efforts must be made by the health authorities to allow access to the various treatments, better monitoring of these patients and above all parallel prevention to detect AKF and CKF as soon as possible and prevent their progression towards the terminal stage.
References
- Liyanage T, Ninomiya T, Jha V, Neal B, Patrice H, et al. (2015) Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet 385(9981): 1975-1982.
- Jha V, Martin DE, Bargman JM, Davies S, Feehally J, et al. (2017) Ethical issues in dialysis therapy. Lancet 389(10081): 1851-1856.
- Bamgboye EL (2003) Hemodialysis: management problems in developing countries, with Nigeria as a surrogate. Kidney Int Suppl 83: S93-S95.
- G Ashuntantang, C Osafo, WA Olowu, F Arogundade, A Naing, et al. (2017) Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: A systematic review. Lancet Glob Health 5(4): e408-e417.
- Niang A, Lemrabott AT (2020) Global dialysis perspective in Senegal. Kidney360 1(6): 538-540.
- Bensalem S (2009) Specificities of fistula complications arteriovenous disease in diabetics on hemodialysis. Diabetes and Metabolism 5(1): 40-42.
- Gmahoungou DT, Eyeni Sinomono E, Foungou Tshiloulou (2021) Dialytic emergencies: epidemiological, clinical, etiological and evolutionary aspects. Nephrol Therap 17(5): 368.
- Vinsonneau C, Camus C, Combes A, Beauregard M, Klouche K, et al. (2006) Continuous venovenous hemodiafiltration with multipleorgan dysfunction syndrome: a multicenter randomized trial. Lancet 368(9533): 379-385.
- Payen D, Berton C (2005) Acute renal failure: epidemiology, incidence and prognostic criteria. Ann Fr Anesth Reanim 24(2): 134-139.
- (2013) ANSD (National Agency for Statistics and Demography) Situation economic and social situation in Senegal.
- Kane Y, Leye MM, Tondi ZM, Tall LA, Maria F, et al. (2016) Decentralization of Dialysis In Senegal: 1 Year Experience of The Center of Tambacounda in The East of The Country. ESJ 12(36): 164-173.
- Rafie H (2016) Bone-mineral disorders in chronic hemodialysis patients in the nephrology-hemodialysis department of Aristide Le Dantec hospital. Thesis in Nephrology 24.
- EL Faize LK (2019) Evaluation of tunneled catheters in chronic hemodialysis patients: multicenter study in four hemodialysis centers in Dakar. Dissertation of DES in Nephrology 316.
- Salima T, Amel B, Amer B (2016) Epidemiological study of chronic renal failure in Tébessa (Algeria), case of 71 patients. Antropo 36: 91-98.
- Ramilitiana B, Rakotoarivoni ST, Raben Janahara (2010) Epidemioclinical profile and outcome of chronic renal failure recipients of hemodialysis at the CHU HJRP Antananarivo Madagascar. Review of Anesthesia-Resuscitation and Emergency Medicine 2(1): 11-14.
- Kane Y (2014) One-year evaluation of the activity of the hemodialysis unit of the regional hospital center of Tambacounda. Dissertation DES in Nephrology 929.
- Coulibaly JM (2010) Monitoring and management of complications of arteriovenous fistulas in chronic hemodialysis patients in Dakar from January 2002 to December 2008. Dissertation from DES en Néphrologie 256.
- Medkouri G, Aghai R, Anabi A Yazidi A, Benghanem M, et al. (2006) Analysis of vascular access in hemodialysis unit in Casablanca. Saudi J Kidney Dis Transplant 17(4): 516-520.
- Leye A, Diouf B, Ndongo S (2004) Secondary hyperparathyroidism in chronic hemodialysis patients in Dakar. Dakar Med 49(1): 23-27.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...