Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case Report(ISSN: 2641-1687) 
Metastatic Melanoma of the Bladder: A Case-Report and Literature Review Volume 2 - Issue 3
Jackie Bitton1*, Charles Chatzopoulos2, Sandrine Rorive3 and Claude C Schulman4
- 1Department of Surgery, Faculty of Medicine, University of Brussels, Belgium
- 2Department of Urology and Robotic Surgery, Delta Hospital-Chirec, Belgium
- 3Department of Pathology, University of Brussels, Belgium
- 4Department of Urology, Edith Cavell Clinic-Chirec, University of Brussels, Belgium
Received: November 18, 2019; Published: November 21, 2019
Corresponding author: Jackie Bitton, Department of Surgery, Faculty of Medicine, University of Brussels, Belgium
DOI: 10.32474/JUNS.2019.02.000138
Abstract
Melanoma is an aggressive tumour with an increasing incidence. Metastatic melanoma of the bladder is a very rare finding. We report the case of a 78-year-old man who presented with visible hematuria. Cystoscopy revealed bladder lesions that were endoscopically resected and diagnosed as melanoma of the bladder. Past history showed previous skin melanoma eleven years earlier and later recurrence in the left tight in 2016. We will discuss the epidemiology and treatment options of malignant metastatic melanoma based on a review of the literature.
Keywords: Bladder; melanoma; metastatic
Introduction
Melanoma is a solid tumour characterized by the malignant transformation of melanocytes. In the last 50 years, the incidence increased faster than almost any other cancer. Mortality has increased also, with a plateau among females being reached recently, but with continued increase among males [1]. The predominant site is skin with a 5-year overall survival rate of 80% [2]. Melanoma is an aggressive malignancy with a poor prognosis that tends to metastasize mainly into the lungs, brain, liver, bone and gut [3]. Reported cases of metastatic melanoma to the bladder are rare, with less than 30 cases reported until now in the English literature. However, out of autopsy series of patients with extraregional disease, 18-37% also have metastases in the bladder. When it occurs, the main complaints are hematuria or lower urinary tract symptoms [4]. We report the case of a 78-year-old man with hematuria who presented on microscopic examination of transurethral resection of bladder lesions of metastatic melanoma eleven years following his first diagnosis of malignant melanoma of the skin
Case Report
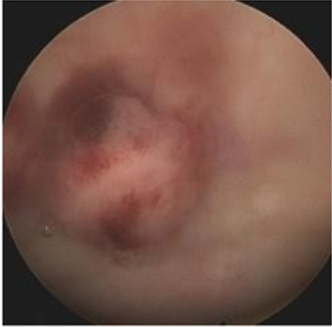
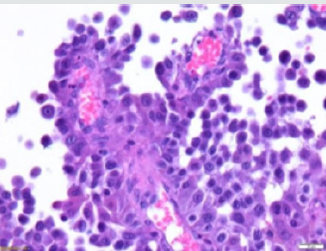
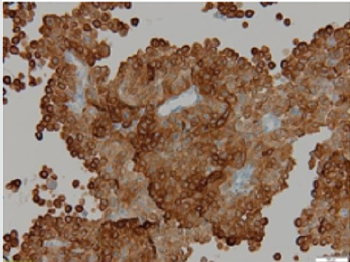
A 78-year-old patient was referred to the Urology Department with macroscopic hematuria. The cytology was negative. A standard assessment associating cystoscopy (Figure 1) and abdominal computed tomography (CT) scan revealed the existence of multiple exophytic lesions located on different locations of the bladder wall without evidence of other lesions on radiological investigations (Figure2). A transurethral resection of the bladder lesions was therefore performed. Histological examination showed infiltrative lesions composed of tumors cells arranged in solid and papillary architecture (Figure3). The tumors cells were negative for Cytokeratins (AE1/AE3, CK5/6, CK7, CK14), GATA 3 and p63 excluding a urothelial origin. A strong reactivity was observed for all melanoma markers (Melan-A, HMB45, S100 and SOX10) confirming the diagnosis of melanoma (Figure4). In addition, Next Generation Sequencing analysis identified the presence of the BRAF V600K mutation in tumors cells. Reviewing his past medical record showed that the patient had a history of two cutaneous lesions diagnosed as melanomas in 2008. The first lesion was located at the right anterior scapular level, management consisted of a resection and the diagnosis of melanoma with a Breslow index of 1mm and a Clarke IV could be established. A control every 3 months was carried out in this context. In 2010, an extended surgery with sentinel lymphadenectomy showed the presence of a positive lymph node. This diagnosis justified an obvious right axillary lymph node dissection showing the presence of an infiltrate lymph node by melanoma. Given the microscopic nature of this node, vaccination with Ag MAGE 3 was not considered. In 2016, recurrence of a melanoma in the left thigh was removed. The patient was under active surveillance with imaging control and showed no recurrence or metastatic disease until his presentation with hematuria. The diagnosis of metastatic melanoma of the bladder was confirmed and additional investigations including PET-CT, showed the presence of multiple metastatic lesions (pulmonary, hepatic and mesenteric lymph node). The patient is now under immunotherapy with nivolumab and ipilimumab and control cystoscopy, MRI and PET- CT will be performed after 3 months.
Figure 4: Diffuse positivity of tumor cells for Melan A (immunohistochemical staining with anti-Melan A antibody, x20).
Discussion
Metastatic bladder constitutes less than 5% of all bladder tumors and metastatic malignant melanoma to the bladder is very rare with only few cases reported in literature [5]. Clinical evidence of this type of cancer is infrequent and, in most cases, patients presented with hematuria or other urinary tract symptoms. Cystoscopy performed as a first examination allows the recognition of characteristic pigmented lesions. In case of negativity of urothelial markers, a series of melanocyte markers such as HMB- 45, S-100, Melan-A can be tested as well as a research for the BRAF mutation to characterize the lesions. In our case, we did not know whether it was a primary or a metastatic melanoma. Ainsworth et al. [6] have established criteria to facilitate the difference:
a) a detailed clinical history that shows no evidence of a
regressed cutaneous melanoma,
b) a complete dermatological exam including the use of a
Wood’s light to exclude primary cutaneous lesions,
c) an ophthalmic exam to rule out primary melanoma of the
eye,
d) exhaustive clinical studies showing no visceral primary
sites and no visceral site presentation since initial diagnosis,
e) recurrence pattern showing consistency with the primary
tumors and no widespread metastasis after the primary tumor
diagnosis, and
f) the presence of atypical melanocytes at the tumor margins
on microscopic examination.
Therefore, in our case, a subsequent diagnosis could be made on the basis of cystoscopy findings, histopathologic features and a clinical history of previous melanoma lesions. Several treatments for malignant melanoma metastatic to the bladder are available. It is essential to take into account, the performance status of the patient, as well as the anatomic location of the metastases, the existence of bladder symptoms and the life expectancy. Radical cystectomy is an aggressive approach and should be proposed only for limited metastatic disease and favorable prognostic factors. For management of bladder symptoms, conservative transurethral resection of the bladder or partial cystectomy is considered. Treatments with systemic chemotherapy were reported as an adjunct to endoscopic resection; however, this should be limited to patients with good performance status [7]. Special attention should also be paid to patients presenting with BRAF V600 mutation; since two practical approaches can be considered: targeted therapy (anti-BRAF/MEK) versus immunotherapy (anti-CTLA4, anti-PD-1) and sequential versus combination regimens [8]. These treatments are associated with an overall survival and progression free survival better than chemotherapy or interleukin 2 though there is an increased risk of systemic toxicities.
Conclusion
Reported cases of metastatic melanoma to the bladder are rare. Patients are often asymptomatic and clinically evident metastases usually indicates an advanced disease. Given the difficulty to establish the diagnosis, combination of patient’s past clinical history, cystoscopy, imagery and histopathological findings is necessary to determine the primary or metastatic nature of the tumors. Management of the patient should be guided by his age, general condition, symptoms, number and location of metastases, as well as the life expectancy. Despite the variety of treatments such as the advent of immunotherapy or targeted-systemic therapy showing extended survival of patients, the prognosis of metastatic melanoma remains poor.
References
- Berwick M, Buller DB, Cust A, Gallagher R, Lee TK, et al. (2016) Melanoma Epidemiology and Prevention. Cancer Treat Res 167: 17‑49.
- Cancer Network (2019) Mucosal Melanoma: New Insights and Therapeutic Options for a Unique and Aggressive Disease.
- Krishnan A, Caravaglio JV, Jhaveri F (2017) Metastatic Malignant Melanoma of the Urinary Bladder in a Patient with Benign Prostatic Hyperplasia and Urethral Stricture. Clin Genitourin Cancer15:119‑121.
- Patil RV, Woldu SL, Lucas E, Quinn AM, Francis F, et al. (2017) Metastatic Melanoma to the Bladder: Case Report and Review of the Literature. Urol Case Rep11: 33‑36.
- Topal CS, Kır G, Daş T, Sarbay B, Tosun Mİ (2016) Metastatic malignant melanoma of the urinary bladder: A case report and review of the literature. Indian Journal of Pathology and Microbiology59: 532-534.
- Ainsworth AM, Clark WH, Mastrangelo M, Conger KB (1976) Primary malignant melanoma of the urinary bladder. Cancer37: 1928‑1936.
- Paterson A, Sut M, Kaul A, Altieri V, Mutch F, et al. (2012) Metastatic malignant melanoma of the urinary bladder: Case report and literature review. Cent European J Urol65: 232‑234.
- Cancer Network(2019) Optimal Treatment Selection for Patients with Metastatic Melanoma.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...