Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case report(ISSN: 2641-1687) 
Incidental Penile Cancer - Presentation of A Case Volume 4 - Issue 2
Raucel Vera Granada1*, Gilda Díaz Dueñas2, Israel Darío Carrillo Quisnia2, Lázaro Deiny and Rodríguez Borrego1
- 1University Hospital, Iván Portuondo, Cuba
- 2General University Hospital, Calixto García, Cuba
Received: January 25, 2022; Published: February 01, 2023
Corresponding author: Raucel Vera Granada, University Hospital, Iván Portuondo, Cuba
DOI: 10.32474/JUNS.2023.04.000182
Abstract
Penile cancer is a condition that usually occurs between the ages of 50 and 70. Its ethylology is multifactorial. Different variants of squamous cell carcinoma are part of more than 95% of cases. Doubtful penile lesions should be biopsied and histologically verified before local treatment. The objective of the work is to describe a clinical case of genital trauma and incidental penile cancer diagnosis. We present a 34-year-old patient who was presented for penile zipper trauma. The biopsy result reporting squamous cell carcinoma is received and a partial penectomy is performed. It is concluded that penile carcinoma is a rare malignant disease. Early detection and identification of penile cancer is of vital importance. The treatment of penile cancer is surgical, reserving chemotherapy and radiotherapy for adjuvant.
Keywords: Penile cancer; lymphadenectomy; penis
Introduction
Penile cancer is a condition that generally occurs between 50 and 70 years of age, 1/3 of the cases affect men under 50 years of age; being 1% of all urogenital tumors. It is associated with the presence of phimosis, poor hygiene, chronic inflammatory conditions of the penis, cigarette smoking, and human papillomavirus infection. The only known protective factor is circumcision before puberty, but there is no evidence that supports its massive application [1,2]. The different variants of squamous cell carcinoma are part of more than 95% of the cases of malignant disease. Biopsy and histological verification should be taken of doubtful penile lesions before local treatment. Penile cancer can be cured in up to 80% of cases if diagnosed early. Local treatment, while potentially lifesaving, can be crippling and potentially devastating to the patient’s psychological well-being [3].
Clinical Case
A 34-year-old white male patient, with a history of health, who attended the emergency room due to a jamming of the foreskin in the zipper, with increased volume, inflammatory signs and pain, for which he was treated as penile cellulitis; with antibiotic therapy and general measures without presenting improvement in the 6 subsequent days. The patient returns to the emergency room of the Iván Portuondo General Teaching Hospital in San Antonio de los Baños, province of Artemisa, where he is evaluated by the urology service and admission for emergency surgical treatment is decided with the diagnosis of penile abscess; prior informed consent (Figures 1 & 2).
On Physical Examination
Penis with increased volume, pain on palpation, swollen, hyperemic, hot, with discharge of purulent discharge, stench, with inability to retract the foreskin and fluctuating areas.
Leucograma.
Hb:12.6 g/l Hto:0.38
Ltos:16.9x 10 9 P:0.70 L:0.30
Glicemia: 6.3 mmol/l Creatinina: 90 mmol/l
Abdominopelvic ultrasound: presence of 0.9 cm enlarged inguinal lymph nodes, the largest in the right inguinal region. In the intraoperative period, a circular and dorsal incision is made in the foreskin, evidencing the presence of a bleeding, necrotic and abscessed tumor mass that prevents visualization of the glans penis, so the dissection is continued until the entire penis is discovered, appreciating that the tumor mass infiltrates the prepuce, glans penis and distal third of penis. Necrectomy of the skin of the foreskin is performed, extensive washings with antiseptic solutions and a sample for biopsy is taken from the area of the tumor lesion. The piece is sent to the department of pathological anatomy and they report:
a) Foreskin: epidermoid carcinoma, exophytic, ulcerated.
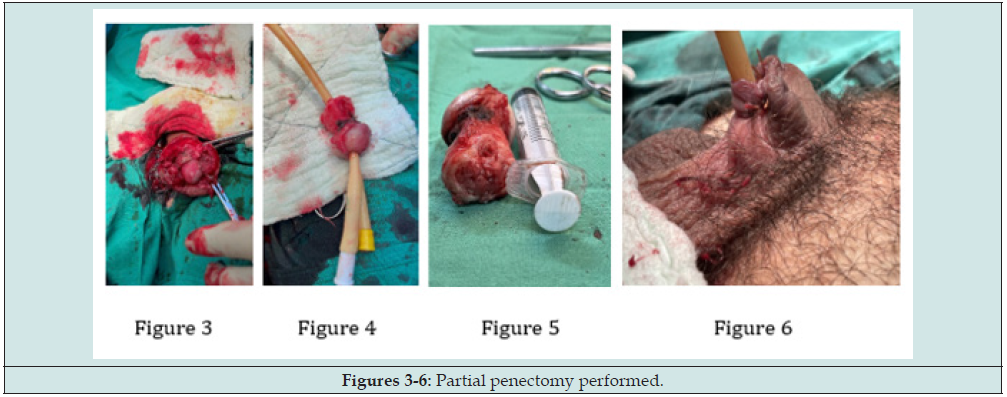
By the clinical symptoms and signs, as well as the results of the biopsy; The case is discussed collectively and partial penectomy is performed with the prior informed consent of the patient and their relatives of the procedure.
b) Glans and penis biopsy: exophytic, ulcerated squamous cell carcinoma (2x2.5x1 cm) infiltrating, moderately differentiated. Moderate inflammatory response, vascular and lymphatic permeation.
c) Corpus cavernosum: Focus of mild dysplasia of the lining epithelium, koilocytosis, and abundant vascularization. The patient was referred to the cancer institute to complete studies and third level treatment (Figures 3-6).
Discussion
Penile carcinoma is a rare malignant disease in developed countries, 0.1-0.7 per 100,000 inhabitants. However, in underdeveloped countries the incidence increases considerably to represent 10-20% of malignant tumors in men. The usual age for this type of tumor is between the 6th and 7th decade of life [4]. Our patient was 34 years old; this finding differs from most of the reviewed literature; where the mean age of the patients was over 60 years of age. Penile cancer can variably present as a mass in 50% of cases, the available bibliography suggests that it can appear as an ulcerative lesion in 25% of cases or as an inflammatory lesion in 10% of them, CaP usually drains through the inguinal, iliac, and pelvic nodes; it is frequently associated with a bacterial infection with a fetid and purulent discharge, coinciding with what was stated by Johnston and Nigam in their study [5]. As stated by González et al. The organs that are the focus of hematogenous metastasis are: lung, liver and bones. It is vitally important to know the involvement of lymph nodes, as well as the presence of metastases, since they are parameters that allow us to evaluate the prognosis of these patients. Generally due to lack of clinical knowledge and because in some regions they are considered taboo, patients do not come until the lesions are associated with ulcers, pus, or lymphedema of the lower limbs and genitals, which is related to the case presented [6]. In current protocols, partial or total penectomy will depend on the clinical status of the patient and the lesions.
Currently, there is no consensus on performing lymphadenectomies systematically in all patients operated on for PCa. The current trend is to study the sentinel node. using lymphoscintillography with or without dye, results that are presented in the study by Carlos et al [7]. Phimosis and chronic irritative processes related to poor hygiene are associated with the development of penile cancer, as stated in the reviewed literature, and its incidence is directly linked to low social status, poor hygiene habits, inappropriate sexual behavior, regions with population rural and very rarely the trauma, so each patient must be treated individually; In the case of our patient, the diagnosis was made as a finding after penile trauma [8]. On many occasions, the patient delays in going to his first consultation or medical treatments are used that initially mask the definitive diagnosis as what happened in this case. In our patient, the mean time between the first treatment and the moment of surgical treatment was 6 days. According to reviewed studies, the primary tumor is located preferably in the glans penis in 48%, prepuce in 21%, in both 9%, in the balanopreputial groove in 6% and in the penile body less than 2%. In our study, the location of the tumor was in the glans penis, coinciding with 50% of the cases. The traditional treatment is resection of the tumor with total penectomy in search of free margins with lymphadenectomy or resection of the sentinel node [9].
At present, the trend towards partial penectomy has increased in search of an aesthetic improvement in the results of surgery, accompanied by a lymphadenectomy without metastasis as was done in the case of our patient. Mohs surgery is another trend in which resection of the tumor is performed in layers until reaching free edges of the tumor [10]. In advanced diseases, chemotherapy with cisplatin is recommended, which may or may not be accompanied by methotrexate, 5-fluorouracil, bleomycin may be added. Radiotherapy or brachytherapy are intended for very particular cases that leave us with rescue surgical resection as a second option, among its complications is meatal stenosis and telangiectasias. Follow-up is performed every four months during the first two years, then every 6 months for two years and then annually for the next 5 years. Follow-up consists of an exhaustive physical examination with a study of the lymph nodes with abdominal pelvic CT and chest X-ray [11]. When diagnosed early, penile cancer is highly curable. Due to the rarity of this cancer, clinical trials specifically for penile cancer are rare. Patients with advanced-stage cancer may be candidates for clinical trials evaluating new drugs, biologics, or surgical techniques to improve local control and distant metastases. The selection of treatment depends on the size, location, invasion and stage of the tumor [12-14]. The most important adverse prognostic factors are the presence of adenopathies, the clinical stage at diagnosis, and the degree of cell differentiation.
Conclusion
Penile carcinoma is a rare malignancy. Early detection and identification of penile cancer is of vital importance for timely treatment and to reduce the risk of metastasis and complications. This type of tumor usually occurs between 50 to 70 years of age. Even if the patient consults for traumatic injuries, other types of injuries in the genital area should always be ruled out. The most effective treatment for penile cancer is surgical, reserving chemotherapy and radiotherapy for adjuvant or salvage therapy.
Conflict of interest
The authors have declared that there are no conflicts of interest.
Authors Contribution
Dr. Raucel Vera Granada: Conception and design of the work, collection, analysis and interpretation of data. Writing and critical review of the article.
Dr. Gilda Díaz Dueñas: Conception and design of the work. Analysis of the results and critical review of the article.
Dr. Israel Darío Carrillo Quisnia: Data collection, analysis of results.
Dr. Lázaro Deinys Rodríguez Borrego: Analysis of the results and critical review of the article.
References
- González Espinosa C, Martínez Ramírez A, Calderón Marín C, Bouzó López A, Vázquez Luna F, et al. (2019) Validation of the sentinel node selective biopsy´s technique in penile cancer. Rev Cub Urol 8(3).
- Sánchez Monzón M (2018) Cáncer de pene. Una tragedia evitable visto desde la enfermerí Rev Cub Urol 7: e28.
- Di Capua C, Marco S, Solchaga G, Alba M, Pontones A, et al. (2009) Cancer of the penis. Our experience in 15 years. Actas Urol Esp 33(2): 143-148.
- Soto Delgado M, Arredondo Martínez F, Pedrero Márquez G, Basquero González B, Zurera Cosano A, et al. (2003) Cancer of the Penis. A review of 18 Cases. Actas Urol Esp 27(10): 797-802.
- Johnston M, Nigam R (2019) Recent advances in the management of penile cancer. F1000Res 8: 1-9.
- González M, González C (2011) Domingo M. Cáncer de pene: ¿hay indicaciones actuales de radioterapia? Revisión desde la perspectiva de oncología radioterá Arch Esp Urol 64(4): 351-362.
- Carlos A, Jonathan H, Elena S (2011) Cáncer de pene; presentación de 10 casos. Rev Mex Urol 71(1): 40-46.
- Medline Plus (2019) Opciones de tratamiento por estadio (cáncer de pene). Instituto Nacional del Cá
- Blanco F (2015) Condicionantes demográficos y clínicos para la elección inicial de la vía de administración de metotrexato y motivos para un posterior cambio de vía (Estudio MOTICAR). Acta Reumatológica 1(5): 68-70.
- Im E (2017) Urología en imá Arch Esp Urol 70(3): 373-374.
- Lima T, Meiners M, Soler O (2010) Treatment adherence profile of hypertension patients from the Municipal Health Unit of Fátima, City of Belém, Pará, Amazônia, Brazil. Rev Pan-Amaz Saúde 1(2): 113-120.
- Garcés Erazo K, Quisilema Ron V, Pacheco Romero K, Bungacho Moreno D (2020) Diagnóstico en cáncer de pene. Revista Científica Mundo de la Investigación y el Conocimiento 4(1): 114-121.
- Medlineplus (2020) Lo sentimos, pero no hemos podido encontrar la página que usted ha solicitado.
- Oncolink (2020) La página que ha solicitado no se ha encontrado.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...