Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Evaluation of Buccal Mucosal Graft Urethroplasty for The Treatment of Female Urethral Strictures- A Single Centre Experience Volume 3 - Issue 3
Vijay Krishna Nagalla*
- Department of Urology, MS Ramaiah Medical College, India
Received: January 03, 2022; Published: February 11, 2022
Corresponding author: Vijay Krishna Nagalla, Department of Urology, M.S. Ramaiah Medical College, Mathikere Bangalore, India
DOI: 10.32474/JUNS.2022.03.000163
Abstract
Introduction: Female urethral stricture is a highly under-reported and underdiagnosed condition encountered by the
reconstructive urologist. Urethral dilatation is often performed with urethroplasty offered in select cases. In the present study, we
describe our results in a series of women surgically treated for female urethral stricture disease using a suprameatal approach with
a buccal mucosal graft dorsal on lay technique.
Materials and Methods: All females diagnosed of urethral stricture who underwent buccal mucosal graft urethroplasty from
January 2015 to January 2020 were evaluated retrospectively. Intraoperative and postoperative parameters were assessed.
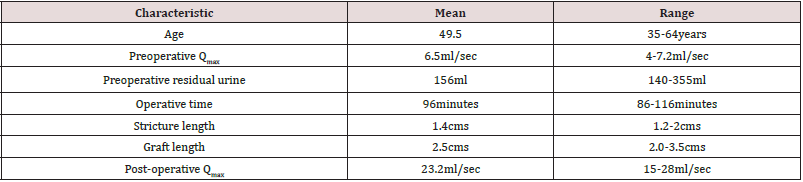
Results: A total of 14 female patients underwent buccal mucosal urethroplasty were evaluated. The mean age of the patients
was 49.5 years ranging from 35 to 64 years. Mean preoperative maximum flow rate [Qmax] on uroflometry was 6.5 ml/second and
the mean residual urine 156 ml. All patients underwent uneventful buccal mucosal graft dorsal on lay technique. At 3 months follow
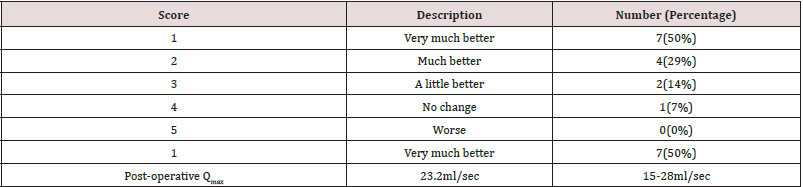
up, the mean Qmax was 23.2 ml/second with mean residual urine of 14 ml. A Self-reporting satisfaction scores using the Patient
Global Impression of Improvement showed that seven patients scored 1 (very much better), four scored 2 (much better), two
patients scored 3 (a little better), and one scored 4 (no change) none of the patients scored a 5 (worse).No recurrence was noted.
Conclusion: Buccal mucosal graft urethroplasty is a feasible surgery for female urethral strictures with minimal short term
complications
Keywords: Buccal Mucosal Graft Urethroplasty; Female Urethral Strictures
Introduction
Female urethral stricture is a highly under-reported and underdiagnosed condition encountered by the reconstructive urologist. The aetiology of urethral stricture is still unclear. Symptoms range from clinically insignificant to severe and debilitating voiding symptoms. Urethral dilatation has been overused for primary and chronic treatment. Urethroplasty with various grafts and flaps have been used with good results in recent times. In this present study, we describe our results in a series of women surgically treated for female urethral stricture disease using a suprameatal approach with a buccal mucosal graft dorsal on lay technique.
Patients and Methods
A total of 14 female patients with urethral stricture who underwent buccal mucosal graft urethroplasty from January 2015 to January 2020 were evaluated retrospectively. Patients were evaluated with a detailed history, physical examination including focused neurological evaluation, uroflometry, a micturating cystourethrogram and an ultrasound of abdomen and pelvis. Evaluation also included a gentle calibration of urethra with a 14 French catheter to assess the site of stricture. All patients had a history of poor stream of urine, 10 (71%) had a sense of incomplete voiding, 2 (14%) presented with recurrent urinary tract infection and 2 (14%) patients had terminal dribbling. Aetiology of the stricture was idiopathic in 9 (64%) of the patients, instrumentation in 3 (22%) and catheterization in 2 (14%). More than half, that is 8 (57%) of the patients had history of repeated urethral dilatation.
Surgical technique
Routine preoperative antibiotic prophylaxis was given and under general anaesthesia with nasal intubation, the surgery was performed in lithotomy position. An initial Urethroscopy was performed with a 6 French ureteroscope to assess the site of stricture, the proximity of the stricture to the bladder neck and any abnormalities in the bladder and trigone. A diluted mixture of 2% xylocaine and adrenaline was injected submucosally into the periurethral tissue using a 26 gauge needle for hydro dissection and haemostasis. An inverted ‘U’ shaped incision (Figure 1A) was given over the urethra exposing the dorsal part of the urethra. Sharp dissection was then done in order to separate the vulvar mucosa from the urethra (Figure 1B). Utmost care was taken to prevent damage to the clitoral cavernous tissue and the anterior portion of the striate sphincter. A full thickness urethrotomy was made using tenotomy scissors at 12 ‘O’ clock position over a guide wire and then extended proximally till normal healthy mucosa could be visualised. The urethra was then calibrated with 18 French catheter to rule out proximal stricture.
Figure 1: Figure showing surgical steps; 1A:- inverted ‘U’ shaped incision; 1B:- sharp dissection to create a plane between clitoris and dorsal aspect of urethra; 1C:- urethrotomy and buccal graft with apical stitch, 1D: - lateral margins of urethra and graft sutured; 1E:- graft quilted to clitoral body.
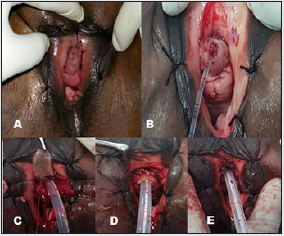
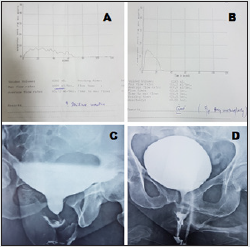
The buccal mucosal graft was then harvested. The Stenson’s duct was marked opposite the upper second molar tooth. Methylene blue was used to mark the graft area to be harvested. A diluted mixture of 2% xylocaine and adrenaline was injected submucosally using a 26 gauge needle for hydrodissection and hemostasis. The buccal mucosal graft was harvested based on the length of the stricture. Haemostasis was achieved with bipolar cautery and the raw area was packed with adrenaline soaked gauze. Buccal mucosa was allowed to heal by secondary intention. Defatting of the graft was performed and the graft was placed in a container with gentamycin and saline. An 18 French catheter was then introduced into the urethra and bulb was inflated. The buccal graft was then sutured to the apex at 11, 12 and 1 ‘0’ clock position (Figure 1C). The lateral margins of the urethra and buccal mucosa were sutured in a dorsal on lay fashion with 4-0 vicryl suture (Figure 1D). This augmented urethra was then quilted to the clitoral body to cover the new urethral roof (Figure 1E). Vulvar mucosa was then approximated with 4-0 vicryl suture. Patients were discharged with catheter after 2 days and were called for catheter removal after 3 weeks (Figures 2A-2D). Patients were followed up after 3 months with assessment of voiding symptoms, examination (Figure 3), uroflometry and a micturating cystourethrogram. The criteria of successful reconstruction were defined as postoperative maximum flow rate (Qmax) greater than 15ml/sec with minimal post void residue (<10% of pre-void). A Self-reporting satisfaction scores using the Patient Global Impression of Improvement was used for assessment of urinary symptoms at 3 months follow up. At subsequent follow ups, the patients were assessed with voiding symptoms and an uroflometry.
Figure 2: Figure 2A, B showing pre-operative uroflometry and micturating cystourethrogram; 2C, 2D: post-operative uroflometry and micturating cystourethrogram
Results
A total of 14 female patients underwent buccal mucosal urethroplasty from January 2015 to January 2020. The mean age of the patients was 49.5 years ranging from 35 to 64 years. Mean preoperative maximum flow rate [Qmax] on uroflometry was 6.5ml/ second ranging from 4 to 7.2ml/second (Table 1). The mean residual urine was 156 ml. In all the patients, calibration with 14 Fr catheter was not possible preoperatively. The mean operative time was 96 minutes ranging from 84 minutes to 116 minutes. Mean stricture length was 1.4 centimetres ranging from 1 to 2.2 centimetres. The mean length of the harvested graft was 2.5 cms ranging from 2.0 to 3.5 cms. Our mean follows up period was 22 months ranging from 6 months to 45 months. None of the patients developed any evidence of graft necrosis post operatively. No wound infection was noted in our series. No donor site complication was noted in our series. Mean hospital stay was 2.5 days ranging from 2-4 days. At 3 months follow up, the mean Qmax was 23.2 ml/second with mean residual urine of 14ml. A Self-reporting satisfaction scores using the Patient Global Impression of Improvement was used which showed that that seven patients scored 1 (very much better), four scored 2 (much better), two patients scored 3 (a little better), and one scored 4 (no change) none of the patients scored a 5 (worse) (Table 2). None of the patients developed recurrence, incontinence, or sexual dysfunction during the course of our follow up.
Table 2: Self-reporting satisfaction scores using the Patient Global Impression of Improvement at 3 months.
Discussion
Female urethral stricture has been described for almost 200
years but is still a widely underdiagnosed condition [1]. Brannen
described the history of female urethral stricture and said that
it was first described by Liz Frank in 1824 and the first case of
female urethral stricture was reported to the earl of London in
1828 [2]. The exact incidence of this entity remains unknown
with very few case reports and retrospective case series reported
in contemporary literature till date [3]. The aetiology for female
urethral stricture has been attributed to idiopathic (49%), chronic
irritation, Prior dilatation, catheterization, instrumentation (7%)
and trauma (6%) [4-7]. Trauma may be in the form of obstetric
injuries, blunt pelvic trauma, or even repeated vigorous coitus
[2]. In our study, idiopathic stricture was the most common cause
accounting for 64% of the cases. Patients usually present with long
standing complaints of voiding and storage symptoms, recurrent
urinary tract infections and sometimes upper urinary tract changes.
Irritative voiding symptoms may be the presenting complaint in
35% of the patients [8].
Evaluation of the patients include a detailed history including
history of stress and urge incontinence, local examination of
the meatus, uroflometry and measurement of residual urine.
Examination should also include gentle calibration with a 14
French catheter [9]. Radiological evaluation of the stricture with a
micturating cystourethrogram helps visualise the stricture. Options
for management of these strictures include urethral dilatation,
urethroplasty with grafts (oral/vaginal) or flaps (vaginal/labial)
[4]. Urethral dilatation alone has a dismal success rate of 47% at a
mean follow up of 43 months [4]. The mean time to recurrence of
stricture has been reported to be around 12 months [10]. Dilatation
combined with daily intermittent self-catheterization is said to have
a success rate of 57% [10,11]. Like in males, it appears that, if a single
dilatation fails, then it is probable that further dilatations are likely
to be palliative rather than curative [4]. Urethral reconstruction in
women is different from that of men because of the shorter length
of the urethra and that the female urethra is sphincter active. Hence
any urethral surgery in the female carries a substantial risk of
incontinence. Anastamotic urethroplasty has not been described till
date. The various approaches to urethral reconstruction are ventral
approach or a dorsal approach. We preferred the dorsal approach
because of the good mechanical and vascular support provided
by the clitoral and cavernosal tissue, it prevents the downward
angulation of the urethral meatus, which may have a subsequent
impact on the direction of the urinary stream and further, it spares
the ventral aspect of urethra for further anti-incontinence surgery.
The disadvantages being increased chances injury to the sphincter
and neurovascular bundle which may lead to in continence or
sexual dysfunction.
A total of 15 studies with 115 patients described urethroplasty
for female urethral strictures, with 6 studies describing flaps and 10
studies describing the use of free grafts for urethral augmentation
[4]. A total of 6 studies have described the use of oral grafts for
female urethral strictures [12-17]. The individual success rate
with the use of oral mucosal graft was 94% with a mean follow up
of 15 months [4]. There were no reported incidences of de novo
incontinence. Oral mucosa is particularly helpful when vaginal
atrophy and fibrosis precludes the use of a local flap. In our series,
there were no cases with recurrence and none of the patients
complained of urinary incontinence post op. With the use of vaginal
or labial grafts, the success rate was reported to be around 80% at a
mean follow up of 22 months [4]. Successful outcome with the use
of vaginal flaps is reported to be around 91% at 32 month follow up.
The main drawbacks of this study are the retrospective nature of
study, lack of control group and short term follow up. A randomized
study with a control group and long term follow up is needed to
further validate this procedure.
Conclusion
Buccal mucosal graft urethroplasty is a feasible surgery for female urethral strictures with minimal short term complications.
References
- Keegan KA, Nanigian DK, Stone AR (2008) Female urethral stricture disease. Curr Urol Rep 9(5): 419-423.
- BRANNAN D (1951) Stricture of the female urethra. J Urol 66(2): 242-253.
- Schwender CEB, Ng L, McGuire E, Gormley EA (2006) Technique and results of urethroplasty for female stricture disease. J Urol 175(3): 976-980.
- Osman NI, Mangera A, Chapple CR (2013) A Systematic Review of Surgical Techniques Used in the Treatment of Female Urethral Stricture. Eur Urol 64(6): 965-973.
- Simonato A, Varca V, Esposito M, Carmignani G (2010) Vaginal flap urethroplasty for wide female stricture disease. J Urol 184(4): 1381-1385.
- Powell Eb (1949) The female urethra; a clinico-pathological study. J Urol 61(3): 557-567.
- Gormley EA (2010) Vaginal flap urethroplasty for female urethral stricture disease. Neurourol Urodyn 29 (S1): S42-S45.
- Smith AL, Ferlise VJ, Rovner ES (2006) Female urethral strictures: successful management with long-term clean intermittent catheterization after urethral dilatation. BJU Int 98(1): 96-99.
- Singh M, Kapoor R, Kapoor D, Kapoor R, Srivastav A, Chipde S (2013) Dorsal onlay vaginal graft urethroplasty for female urethral stricture. Indian J Urol 29(2): 124-128.
- Romman AN, Alhalabi F, Zimmern PE (2012) Distal Intramural Urethral Pathology in Women. J Urol 188(4): 1218-1223.
- Smith Al, Ferlise VJ, Rovner ES (2006) Female urethral strictures: successful management with long-term clean intermittent catheterization after urethral dilatation. BJU Int 98(1): 96-99.
- Ellis LR, Hodges CV (1969) Experiences with female urethral reconstruction. J Urol 102(2): 214-220.
- Scopus preview-Scopus-Document details.
- Migliari R, Leone P, Berdondini E, De Angelis M, Barbagli G, Palminteri E (2006) Dorsal Buccal Mucosa Graft Urethroplasty for Female Urethral Strictures. J Urol 176(4): 1473-1476.
- Tsivian A, Sidi AA (2006) Dorsal Graft Urethroplasty for Female Urethral Stricture. J Urol 176(2): 611-613.
- Berglund RK, Vasavada S, Angermeier K, Rackley R (2006) Buccal mucosa graft urethroplasty for recurrent stricture of female urethra. Urology 67(5): 1069-1071.
- Castillo OA, Sepúlveda F, Feria-Flores MA (2011) Urethroplasty with dorsal oral mucosa graft in female urethral stenosis. Actas Urológicas Españolas 35(4): 246-249.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...