Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Concordance between Urodynamicists: Can We Still Trust the Classification of Urofluxometry Curves? Volume 4 - Issue 1
Paulo Henrique Nahar Barbosa1, Bruno de Andrade Salomão1, Raphael Moura Xavier Enne1, Alex Flávio Mare de Chiara1, João Antonio Pereira-Correia1* and Valter José Fernandes Muller1
- 1*Department of Urology, Servidores do Estado Federal Hospital, Rio de Janeiro, Brazil
Received: December 27, 2022; Published: January 02, 2023
Corresponding author: João Antonio Pereira-Correia, Department of Urology, Servidores do Estado Federal Hospital, Rio de Janeiro, Brazil
DOI: 10.32474/JUNS.2023.04.000177
Abstract
Background: Uroflowmetry is a minimally invasive test for the initial assessment of voiding disorders. Due to its practicality, it is considered a screening tool in the evaluation of such conditions. The evaluation of uroflowmetry curve patterns can, however, generate inter-observer disagreement.
Objective: To assess the degree of interobserver agreement in the interpretation of uroflowmetric flow curves of adult patients.
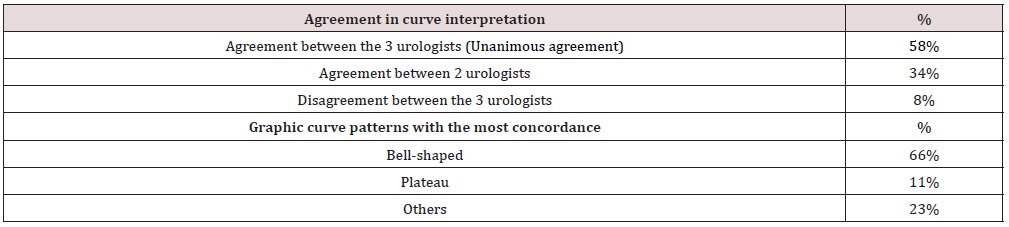
Results: One hundred and thirteen exams were analyzed. Unanimous agreement in curve interpretation was observed in 66 exams (58%) (p=0.0043). Graphic curves with the highest rates of inter-observer concordance were the bell-shaped (66%) and plateau (11%) curves. Among the uroflowmetry tests with interobserver disagreements (47 tests – 42% of the sample), 85% obtained agreement between two researchers (p=0.0001). In these cases, the graphic curve patterns with the most concordance remained the same: bell-shaped (56%) and plateau (13%).
Conclusion: Although we understand that uroflowmetry is still very useful to identify patients for whom more invasive tests are indicated, we believe that better standardization of curve assessment is necessary for greater objectivity and to reduce interpretation biases. In our study, urologists’ experience and dedication to urodynamic study did not affect interobserver agreement in the interpretation of uroflowmetry curves.
Keywords: Uroflowmetry; uroflowmetry curves; interobserver agreement; urodynamic study
Introduction
Uroflowmetry is a minimally invasive test for the initial assessment of voiding disorders. Due to its practicality, it is considered a screening tool in the evaluation of such conditions. Many urologists dedicate their clinical practice to urodynamic diagnosis, using uroflowmetry as a complementary exam during outpatient consultations [1]. The evaluation of uroflowmetry curve patterns can, however, generate inter-observer disagreement. Different examiners may assess the same uroflowmetric curve as having either the “tower” or “bell-shaped” configuration, due to the subjectivity of interpretation. There are still no standardized, objective, or quantitative criteria for classifying flow curves. Clinical studies, conducted primarily in the pediatric population, have shown considerable rates of interobserver variability in the evaluation of such curves [2,3]. Our study aimed to assess the degree of interobserver agreement in the interpretation of uroflowmetric flow curves of adult patients.
Materials and Methods
After approval by the local Ethics Committee, uroflowmetry tests performed by the Department of Urodynamics and Voiding Dysfunction, using the latest version of Dynamed™ urodynamic equipment (Dynamed™, São Paulo, Brazil), were randomly selected using computerized means. The selected exams were presented to three senior urodynamic experts, each having completed more than 4000 exams over a minimal 10-year timespan. After interpretation of the curves, results were evaluated by a fourth researcher who was blinded to the names of the urologists who classified the flow curves. A comparative analysis among groups was conducted using the student´s t-test for continuous data and the Mann-Witney test for categorical data, using a standard significance value of p< 0.01. Statistical analysis was performed using a commercially available data analysis program, GraphPad Prism™, version 5 (La Jolla, CA, USA).
Results
One hundred and thirteen exams were analyzed. Patient demographic data and other results are shown in Tables 1&2, respectively. Unanimous agreement in curve interpretation was observed in 66 exams (58%) (p=0.0043). Graphic curves with the highest rates of inter-observer concordance were the bell-shaped (66%) and plateau (11%) curves. Among the uroflowmetry tests with interobserver disagreements (47 tests – 42% of the sample), 85% obtained agreement between two researchers (p=0.0001). In these cases, the graphic curve patterns with the most concordance remained the same: bell-shaped (56%) and plateau (13%).
Discussion
Urodynamic graphs are essential in the evaluation of voiding function. Curves are directly influenced by the contractility of the detrusor muscle, abdominal effort, coordination of the pelvic musculature, and anatomic obstructions. Consequently, the International Children’s Continence Society (ICCS) updated the standardized nomenclature used in the management of voiding function in 2016. The ICCS report described five types of urinary flow curves: bell-shaped, tower, staccato, interrupted, and plateau [4]. Gammie et al. have asserted that although the utility of urodynamic patterns in the diagnosis of lower urinary tract disorders has been empirically validated, greater clarity and consistency in the description of such voiding graphics are needed [5]. Furthermore, good technique and systematic analyses of results are essential to ensure the diagnostic accuracy of uroflowmetry.5,6 Better definitions for urinary flow time are also needed. The International Continence Society (ICS) considers flow time as “the time when measurable urinary flow actually occurs”, without defining “measurable” [6]. Such variations can change the graphic flow pattern, depending on the demarcation of beginning and end milestones.
A 2007 Italian study evaluated interobserver concordance in the visual assessment of uroflowmetry plots. The agreement was satisfactory in the evaluation of normal flow curves but varied widely in the interpretation of abnormal patterns [7]. The report also commented on the variability of examiner profiles. In addition to experience, the degree of dedication to urodynamic practice increases the rate of interobserver agreement. Diagnoses provided by “pure urodynamicists” (those with greater experience with more invasive urodynamic tests) exhibit higher rates of intraobserver agreement. Urologists with more than 10 years of dedication to urodynamic diagnosis have displayed greater interobserver concordance than those who have dedicated 5 to 10 or less than 5 years to urodynamic testing [8]. However, our study showed that just over half of the flow curves yielded complete agreement among the three examiners, even though the evaluators had extensive experience, each with more than 10 years of urodynamic practice. The first studies to question the role of subjectivity in the interpretation of urinary flow graphs date from the late 1970s [9]. Consequently, measures to increase the objectivity of uroflowmetry have already been proposed by the ICS, and include the use of maximum flow values, flow-volume nomograms, multiple uroflowmetric measurements, and electroneuromyography. In agreement with the conclusions of other investigators, we believe that quantitative indicators must be developed to standardize the interpretation of abnormal uroflowmetric curves, thus reducing the subjectivity of graphic interpretation.
Conclusion
Although we understand that uroflowmetry is still very useful to identify patients for whom more invasive tests are indicated, we believe that better standardization of curve assessment is necessary for greater objectivity and to reduce interpretation biases. In our study, urologists’ experience and dedication to urodynamic study did not affect interobserver agreement in the interpretation of uroflowmetry curves.
Conflict Of Interests
None declared.
References
- Van de Beek C, Stoevelaar HJ, McDonnell J, Nijs HG, Casparie AF, et al. (1997) Interpretation of Uroflowmetry Curves by Urologists. Urol 157(1): 164-168.
- Franco I, Franco J, Lee YS, Choi EK, Han SW (2016) Can a quantitative means be used to predict flow patterns: Agreement between visual inspection vs. flow index derived flow patterns. J Pediatr Urol 12(4): 218.e1-8.
- Faase MA, Nosnik JP, Diaz-Saldano D, Hodgkins KS, Liu DB, et al. (2015) Uroflowmetry with pelvic floor electromyography: inter-rater agreement on diagnosis of pediatric non- neurogenic voiding disorders. J Pediatr Urol 11(4): 198.e1-6.
- Austin PF, Bauer SB, Bower W, Chase J, Franco I, et al. (2016) The Standardization of Terminology of Lower Urinary Tract Function in Children and Adolescents: Update Report from the Standardization Committee of the International Children’s Continence Society. Neurourol Urodyn 35(4): 471-481.
- Gammie A, Rosier P, Rui L, Harding C (2018) How can we maximize the diagnostic utility of uroflow?: ICI-RS 2017. Neurourol Urodyn 37(S4): S20-S24.
- Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, et al. (2002) Good Urodynamic Practices: Uroflowmetry, Filling Cystometry, and Pressure-Flow Studies. Neurourol Urodyn 21(3): 261-274.
- Gacci M, Del Popolo G, Artibani W, Tubaro A, Palli D, et al. (2007) Visual assessment of uroflowmetry curves: description and interpretation by urodynamists. World J Urol 25(3): 333-337.
- Liu YB, Yang SS, Hsieh CH, Lin CD, Chang SJ. (2014) Inter-Observer, Intra-Observer and Intra-Individual Reliability of Uroflowmetry Tests in Aged Men: A Generalizability Theory Approach. Low Urin Tract Symptoms 6(2): 76-80.
- Gammie A, Steup A, Kaper M (2016) Flow time and voiding time – definitions and use in identifying detrusor underactivity. Neurourol Urodyn 35: S68-S69.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...