Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Comparative Characteristic of Blood Plasmas Fibrinolytic Activity in Case of Experimental Intra-Abdominal Infection and Underlying Nephrosis-Nephritis Volume 4 - Issue 2
Fedir Grynchuk*, Andrii Grynchuk, Fedir Grynchuk Jr
- Department of Surgery, SSHE of Ukraine, Bukovynian State Medical University, Ukraine
Received: March 13, 2023; Published: March 21, 2023
Corresponding author: Fedir Grynchuk, Professor, Bukovynian State Medical University, Department of surgery, Chernivtsi, Ukraine
DOI: 10.32474/JUNS.2023.04.000185
Abstract
Introduction: Actuality is due to rather understudied state of fibrinolytic reactions in case of NN with acute IAI which is to be found in practice more frequent. Objective of the study was studying of the features of fibrinolytic activity in case of IAI, that is being developed underlying NN.
Materials and Methods: 100 albino non-pedigree rats. IAI was simulated through the intra-abdominal puncture injection of a 20% auto fecal mixture. NN was simulated by subcutaneous introduction of 5% sodium nitrite solution on distilled water. In the course of the study total TFA, NFA and EFA of blood plasma were studied. The animals were divided into such groups: 1 - intact animals with IAI models, 2 - animals with models of IAI underlying NN.
Results: The activity of fibrinolysis in animals with NN models predominated over the one in intact animals. In 6 hours since IAI was modeled, FA started increasing in both animal groups. However, all of TFA, EFA and NFA in group 1 were increasing statistically significantly. Whereas group 2 was affected by a minor increase. In 12 hours in group 1 FA of plasma was increasing statistically significantly. In group 2 FA of plasma was increasing insignificantly. There was a meaningful increase of EFA in group 1, in contrast, it was insignificant in group 2. The ratio between EFA and NFA decreased in group 1. In contrast, this ratio in group 2 increased statistically significantly and the parameters of EFA indicator in group 2 were statistically significantly higher. In 24 hours, parameters of TFA, NFA and EFA indica-tors in both groups have not changed much. At the same time, the ratio between EFA and NFA was increasing statistically significantly in group 1. In group 2 the ratio decreased. In 48 hours, FA plasma and the ratio of different fibrinolysis elements did not change much in group 1. The parameters of TFA and EFA in group 2 were increasing statistically significantly. The parameters of NFA were decreasing statistically significantly. The ratio between EFA and NFA in group 2 was decreasing very significantly.
Conclusion:
a) The increase in the fibrinolytic activity of blood plasma with the non-enzymatic mechanism’s predomination have been found in experimental nephrosis-nephritis case.
b) The activation of fibrinolysis with balance maintenance between its links within 24 hours has been observed in experimental acute intra-abdominal infection case.
c) In 6 hours, the development of acute intra-abdominal infection in animals with simulated nephrosis-nephritis differs substantially in its quantitative characteristics of the fibrinolytic activity of plasma blood, which is shown by its lack of proper increase, development of imbalance be-tween the links of fibrinolysis, uncontrolled increase of the activity of fermentation mechanisms with disseminated intravascular coagulation syndrome in 48 hours.
d) The basis of the differences that have been detected are the changes in the functional activity of the fibrinolytic system caused by nephrosis-nephritis influence that, in addition to changes in the hemostasis system, provide the grounds for disorders of mechanisms of activation, migration and interaction of effector cells, processes of proliferation, etc.
Keywords: Nephrosis-nephritis; intra-abdominal infection; comorbidity; fibrinolytic system
Abbreviations: IAI: Intra-abdominal infection; EFA: Enzymatic fibrinolytic activity; FA: Fibrinolytic activity; FS: Fibrinolytic system; NFA: Non-enzymatic fibrinolytic activity; NN: Nephrosis-nephritis; TFA: Total fibrinolytic activity
Introduction
The incidence of kidney pathologies, nephrosis and nephritis in particular, is constantly growing all over the world in recent years [1-3]. The number of patients with acute IAI associated with nephritis is constantly growing [4] respectively. The mechanisms of development of such comorbid pathological state are still unrevealed. In addition, the changes of FS have not been studied yet. The importance of such research is stipulated by the role of FS components within the inflammation process development, NN and IAI in particular [5-8]. Therefore, the investigation of FS reactions within acute IAI developing against the ground of nephrosis and nephritis appears to be rather topical.
Materials and methods
The research has been carried out on 100 albino non-pedigree rats, with the weight of 180 to 200 g. The animals were divided into following groups: intact (10), NN model (10), group 1 – intact animals with simulated IAI (40), group 2 – animals with simulated IAI on the background of NN (40). IAI was simulated according to the common method through the intra-abdominal puncture injection of a 20% auto fecal mixture at a dose of 1 ml per 100 g of mass [9]. NN was simulated by subcutaneous introduction of 5% sodium nitrite solution on distilled water in the dose of 0,5 mg per 100 g of mass [10]. IAI was induced 12 hours after NN had been simulated. Before modeling IAI, as well as in 6, 12, 24, 48 hours from the moment of its inducement, blood from the jugular vein was taken for analysis. While carrying out the study the researchers kept to the basic guideline of Vancouver Convention (1979, 1994) concerning biomedical experiments. The animals were taken out of the experiment by anesthetic overdose. All manipulations were performed under the sevoflurane anesthesia. The Bioethics Committee of HSEE of Ukraine «Bukovinian State Medical University», the Ministry of Public Health of Ukraine found the work to be done according to the basic moral and legal principle while conducting the experimental medical research. Total fibrinolytic activity (TFA), non-enzymatic (NFA) and enzymatic fibrinolytic activity (EFA) of blood plasma that determined by the level of azofibrin lysis by O.L. Kukharchuk method were studied [11]. The hypothesis of normal data distribution (Gaussian distribution) was tested in selections by Shapiro-Wilk criterion. Verification of the hypothesis of average data equality was carried out by Wilcoxon and Mann-Whitney-Wilcoxon criterion. The results of the study were statistically processed by the Microsoft® Office Excel (build 11.5612.5703) tables.
Results
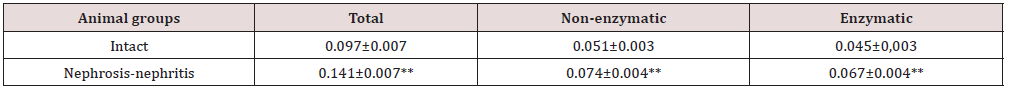
The activity of all fibrinolysis elements with simulated NN statistically significantly prevailed over those of the intact animals (Table 1). In 6 hours since IAI was modeled, FA started increasing in both animal groups. How-ever, all of TFA (Figure 1), EFA (Figures 2 & 3) and NFA in group 1 were increasing statistically significantly. Whereas group 2 was affected by a minor increase, this was probably due to the high baseline. At the same time, the parameters of TFA, EFA and NFA indicators were statistically significantly higher in group 2. FA was increasing in in both groups, mainly at the expense of EFA (Figure 4). The interaction between different fibrinolysis bars in group 2 was statistically significantly lower (p<0,05). In 12 hours in group 1 FA of plasma was increasing statistically significantly. In group 2 FA of plasma was increasing insignificantly. But the parameters of TFA, NFA and EFA indicators in group 2 prevailed predominantly. There was a meaningful increase of EFA in group 1, in contrast, it was insignificant in group 2. But the parameters of EFA indicator in group 2 were higher. The ratio between EFA and NFA decreased in group 1. In contrast, this ratio in group 2 increased statistically significantly (p<0.01) and the parameters of EFA indicator in group 2 were statistically significantly higher (p<0.05).
Figure 1: Note: *- validity coefficient Р between adjacent groups < 0,05, **- < 0,01; +- validity coefficient between adjacent terms of observation < 0,05, ++ - < 0,01 (only statistically significant differences are given). Figure 1: The dynamics of total fibrinolytic (Е440 / ml / h) blood plasma activity of experimental animals in the process of acute intra-abdominal infection development.
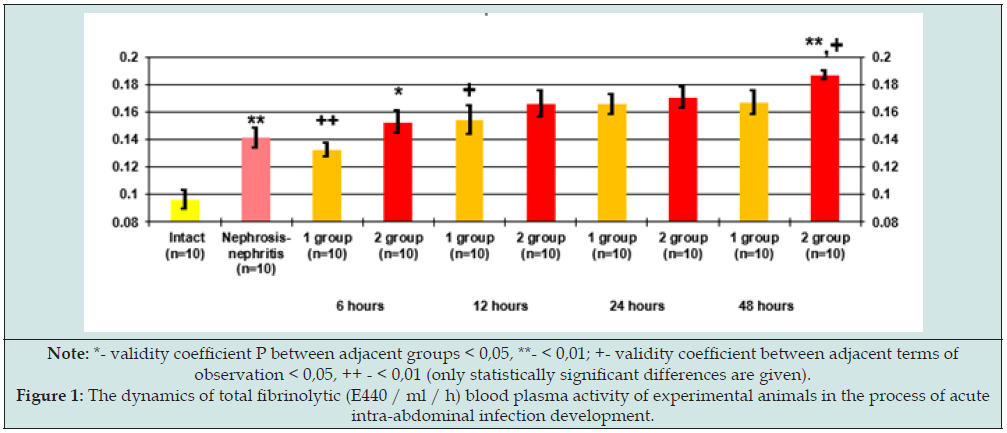
Figure 2: Note: *- validity coefficient Р between adjacent groups < 0,05, **- < 0,01; +- validity coefficient between adjacent terms of observation < 0,05, ++ - < 0,01 (only statistically significant differences are given). Figure 2: The dynamics of non-enzymatic fibrinolytic activity (Е440 / ml / h) of blood plasma of experimental animals in the process of acute intra-abdominal infection development.
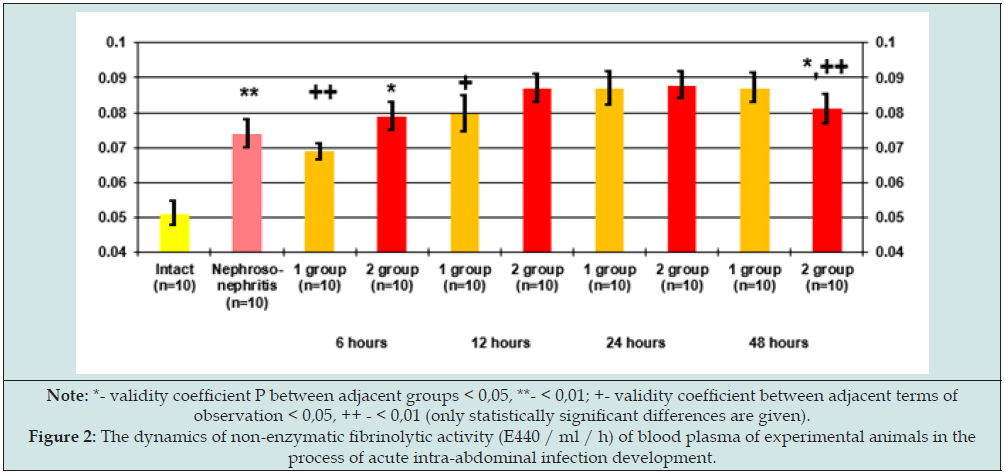
Note:** - validity coefficient Р < 0,01 (only statistically significant differences are given).
In 24 hours, parameters of TFA, NFA and EFA indicators in both groups have not changed much. At the same time, the ratio between EFA and NFA was increasing statistically significantly (p<0.01) in group 1 showing the non-enzymatic mechanisms of fibrinolysis pre-dominance. In group 2 the ratio decreased being indicative of the fermentation fibrinolysis activation. In 48 hours, FA plasma and the ratio of different fibrinolysis elements did not change much in group 1. The parameters of TFA and EFA in group 2 were increasing statistically significantly and statistically significantly prevailed. At the same time the parameters of NFA were decreasing statistically significantly and became statistically significantly lower than in group 1. The ratio between EFA and NFA in group 2 was decreasing very significantly (p<0.01). At the beginning of the experiment, we used more animals. But all animals with IAI models on the background of NN died after 48 hours. Therefore, in this article, the observation period is limited to 48 hours.
Discussion
To our mind, the increase in plasma fibrinolytic activity may be caused by changes in coagulation, which usually occur in NN [12- 14]. Taking into account a regulatory role of the fibrinolytic system in the implementation of protective function against inflammation [15,16], the identified FA of plasma increase in animals with NN models can be considered as one of the most important features changing IAI development. Such changes can occur through the influence of the fibrinolytic system factors on the proliferation mechanisms, which interrupt the processes of the inflamed place delimitation as well as the influence on activation factors and cells migration - inflammation effectors [17,18]. The increase of FA of plasma in case of IAI is a natural process, which is caused by different factors, among which are components of the complement and kallikrein-kinin system, immune complexes, growth of the activity of the coagulation system, etc. [19-21]. At the same time, in addition to hypercoagulation changes compensation, the important mechanisms of inflammation progress are associated with the fibrinolytic activation. Plasmin activates growth factors, C8 - a complement fraction. Direct plasmin effect on the endothelium improves the cells migration, effectors of inflammation in the place [22,23], and the products of enzymatic degradation of fibrin are the activators of immunocompetent cells and chemoattractant and they can play the role of opsonin’s.
Thus, the lack of proper enzymatic fibrinolysis activation in animals with NN models in 6 hours after IAI inducement serves as a precondition to regulate disorders of the inflammatory process. Further IAI progress in 12 hours is provided with a growing activation of the fibrinolytic system. At the same time, in group 1, the activity of various components of fibrinolysis increases significantly. This is a natural reaction to the progression of IAI. A high level of enzymatic fibrinolysis predominates, indicating the activation of inflammation regulation mechanisms. As for group 2, at first sight, the relatively lower level of fibrinolysis in group 2 is a manifestation of greater activity of non-enzymatic mechanisms aimed at activating coagulation and limiting inflammation. But the following should be taken into account. The liver and kidneys are known to be one of the most significant physiological sources of plasminogen. Their functions are affected in NN cases, moreover, they are affected even more in IAI cases because of toxic damage [24]. Therefore, some relative lag in the activity of enzymatic fibrinolysis in group 2 may be caused by kidney damage and disruption of urokinase synthesis, which causes inhibition of the exogenous pathway of plasminogen activation. FA of plasma was increasing during 24 hours in group 1, mainly, due to the nonenzymatic factors.
Taking into account a direct connection between NFA level and the amount of thrombin [25,26], it may be interpreted as the consequence of coagulation system activation, which is aimed at restraining and delimiting the inflammatory process in the peritoneal cavity. It can explain a slight increase of EFA as well. A stable level of FA in group 2 indicates, allegedly, the balanced function of mechanisms of inflammation regulation. At the same time, the level of EFA increased, and the level of NFA almost did not change. Taking into account the inhibition of urokinase synthesis at NN, the increase in the level of EFA enables us to suggest, that an increasing level of EFA in group 2 is due to the initiation of other plasminogen donators, activated leukocytes, endothelial cells, microorganisms, broken tissues, etc. A high level of EFA in group 2 contribute to a significant number of circulating activators of plasminogen of different origin - blood, tissue, endothelial, bacterial, etc. [27-29]. The absence of significant changes in the indicators studied in group 1 in 48 hours is evidenced by the balance between the coagulation and anti- coagulation systems, on the one hand, and by the functional stability of factors - regulators of fibrinolysis, on the other.
A significant decrease of NFA in 48 hours in group 2 is indicative by decrease of the thrombin content and hypocoagulative changes in blood, whereas a synchronous significant increase in FFA level is indicative of the development of the initial stage of disseminated intravascular coagulation syndrome [30,31]. Considering the duration of IAI which causes disorders of the liver functions, being the main source of factors and inhibitors of fibrinolysis, and initial and subsequent kidney disorders, such EFA increase also confirms the development of unlimited fibrinolysis, which has the nature of a cascade of autocatalytic progressive reactions. Occurrence of the syndrome disturbs the functioning of organs and tissues, liver and visceral peritoneum in particular, which represent antiproteinase barrier. On this background, the plasmin of plasma, which is known to be a major factor of enzymatic fibrinolysis, easily goes into the tissue, in particular, into the peritoneum, which leads to disorders of proliferation processes, resulting in unrestrained spread of inflammation in the peritoneal cavity. Finally, it should be added that we found similar changes in the state of fibrinolysis in the case of another comorbid condition - IAI on the background of diabetes [32]. This shows that the development of IAI against the background of comorbidity has common mechanisms.
Conclusions
a) The increase in the fibrinolytic activity of blood plasma with the non-enzymatic mechanism’s predomination have been found in experimental nephrosis-nephritis case.
b) The activation of fibrinolysis with balance maintenance between its links within 24 hours has been observed in experimental acute intra-abdominal infection case.
c) In 6 hours, the development of acute intra-abdominal infection in animals with simulated nephrosis-nephritis differs substantially in its quantitative characteristics of the fibrinolytic activity of plasma blood, which is shown by its lack of proper increase, development of imbalance between the links of fibrinolysis, uncontrolled increase of the activity of fermentation mechanisms with disseminated intravascular coagulation syndrome in 48 hours.
d) The basis of the differences that have been detected are the changes in the function-al activity of the fibrinolytic system caused by nephrosis-nephritis influence that, in addition to changes in the hemostasis system, provide the grounds for disorders of mechanisms of activation, migration and interaction of effector cells, processes of proliferation, etc.
Conflict of Interest
The authors state that there is no conflict of interest.
References
- Nüsken E, Weber LT (2022) IgA vasculitis nephritis. Curr Opin Pediatr 34(2): 209-216.
- Schurder J, Buob D, Perrin P, Thervet E, Karras A, et al. (2021) Acute interstitial nephritis: aetiology and management. Nephrol Dial Transplant 36(10): 1799-1802.
- Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, et al. (2021) Executive summary of the KDIGO 2021 Guideline for the Management of Glomerular Diseases. Kidney Int 100(4): 753-779.
- Grynchuk FV, Shurma AI, Sheremet MI, Grynchuk AF, Tarabanchuk VV, et al. (2022) Optimization of diagnosis in patients with diabetes mellitus and other comorbid pathology in emergency abdominal surgery. Rom J Diabetes Nutr Metab Dis 29(3): 306-309.
- Oe Y, Hayashi S, Fushima T, Sato E, Kisu K, et al. (2016) Coagulation Factor Xa and Protease-Activated Receptor 2 as Novel Therapeutic Targets for Diabetic Nephropathy. Arterioscler Thromb Vasc Biol 36(8): 1525-1533.
- Sumi A, Yamanaka-Hanada N, Bai F, Makino T, Mizukami H, et al. (2011) Roles of coagulation pathway and factor Xa in the progression of diabetic nephropathy in db/db mice. Biol Pharm Bull 34(6): 824-830.
- Akahoshi T, Sugimori H, Kaku N, Tokuda K, Nagata T, et al. (2015) Comparison of recombinant human thrombomodulin and gabexate mesylate for treatment of disseminated intravascular coagulation (DIC) with sepsis following emergent gastrointestinal surgery: a retrospective study. Eur J Trauma Emerg Surg 41(5): 531-538.
- Bilookyi OV, Hrynchuk FV, Bilookyi VV, Rohovyi YuIe (2022) Diahnostuvannia i likuvannia zhovchnoho perytonitu [Diagnosis and treatment of biliary peritonitis]. Chernivtsi: BDMU.
- Lee M, Kim K, Jo Y, Lee J, Hwang J (2016) Dose-dependent mortality and organ injury in a cecal slurry peritonitis model. J Surg Res 206(2): 427-434.
- Vozianov OF, Hozhenko AI, Fedoruk OS (2003) Hostra nyrkova nedostatnist [Acute renal failure]. Odesa: Odesskyi meduniversytet.
- Kukharchuk OL (1996) Patogenetychna rol’ ta metody korekcii’ integratyvnyh porushen’ gormonal’no-mesendzhernyh system reguljacii’ gomeostazu natriju pry patologii’ nyrok [Pathogenetic role and correction methods of integrative sodium hormonal-messenger regulation systems disorders in kidney pathology]. Odesa.
- Biederman LE, Conces M, Shenoy A (2023) Acute Interstitial Nephritis in the Pediatric Population: A Review of Etiologic Associations, Histologic Findings, and Clinical Outcome. Pediatr Dev Pathol 26(1): 13-17.
- Oh H, Park HE, Song MS, Kim H, Baek JH (2022) The Therapeutic Potential of Anticoagulation in Organ Fibrosis. Front Med (Lausanne) 9: 866746.
- Xia M, Liu D, Peng L, Li Y, Liu H, et al. (2020) Coagulation parameters are associated with the prognosis of immunoglobulin a nephropathy: a retrospective study. BMC Nephrol 21(1): 447.
- Monastyrs’kyj VA. (2007) Trombin - plazminova systema - odna z osnovnyh reguljatornyh system organizmu [Trombin-Plasmin System - One of the main regulatory systems of the organism]. Lviv Nac Med. Un-t im. D. Galyc’kogo, Nauk. t-vo im. G. Shevchenka. Lviv: Liga-Pres.
- Serhan CN, Ward PA, Gilroy DW (2010) Fundamentals of Inflammation. Cambridge University Press.
- Cole E, Davenport R, De’Ath H, Manson J, Brockamp T, et al. (2013) Coagulation system changes associated with susceptibility to infection in trauma patients. J Trauma Acute Care Surg 74(1): 51-57.
- Ferluga J, Kouser L, Murugaiah V, Sim RB, Kishore U (2017) Potential influences of complement factor H in autoimmune inflammatory and thrombotic disorders. Mol Immunol 84: 84-106.
- Bekassy Z, Lopatko Fagerström I, Bader M, Karpman D (2022) Crosstalk between the renin-angiotensin, complement and kallikrein-kinin systems in inflammation. Nat Rev Immunol 22(7): 411-428.
- Derive M, Boufenzer A, Bouazza Y, Groubatch F, Alauzet C, et al. (2013) Effects of a TREM-like transcript 1-derived peptide during hypodynamic septic shock in pigs. Shock 39(2): 176-182.
- Weiler H (2014) Inflammation-associated activation of coagulation and immune regulation by the protein C pathway. Thromb Res 133(1): 32-34.
- Rajendran P, Rengarajan Th, Thangavel J, Nishigaki Y, Sakthisekaran D, et al. (2013) The Vascular Endothelium and Human Diseases. Int J Biol Sci 9(10): 1057-1069.
- Godo S, Shimokawa H (2017) Endothelial Functions. Arterioscler Thromb Vasc Biol 37(9): e108-e114.
- Clements TW, Tolonen M, Ball CG, Kirkpatrick AW (2021) Secondary Peritonitis and Intra-Abdominal Sepsis: An Increasingly Global Disease in Search of Better Systemic Therapies. Scand J Surg 110(2): 139-149.
- Longstaff C, Kolev K (2015) Basic mechanisms and regulation of fibrinolysis. J Thromb Haemost 13(1): 98-105.
- Li X, Ma X (2017) The role of heparin in sepsis: much more than just an anticoagulant. Br J Haematol 179(3): 389-398.
- Bhattacharya S, Ploplis VA, Castellino FJ (2012) Bacterial plasminogen receptors utilize host plasminogen system for effective invasion and dissemination. J Biomed Biotechnol 2012: 482096.
- Gebbink MF (2011) Tissue-type plasminogen activator-mediated plasminogen activation and contact activation, implications in and beyond haemostasis. J Thromb Haemost 9(1): 174-181.
- McDonald B, Davis RP, Kim SJ, Tse M, Esmon CT, et al. (2017) Platelets and neutrophil extracellular traps collaborate to promote intravascular coagulation during sepsis in mice. Blood 129(10): 1357-1367.
- Iba T, Levy JH (2020) Sepsis-induced Coagulopathy and Disseminated Intravascular Coagulation. Anesthesiology 2020 132(5): 1238-1245.
- Iba T, Levi M, Thachil J, Levy JH (2022) Disseminated Intravascular Coagulation: The Past, Present, and Future Considerations. Semin Thromb Hemost 48(8): 978-987.
- Grynchuk FV, Grynchuk AF, Maksimiuk VV (2017) Comparative characteristic of fibrinolytic activity in case of experimental peritonitis and underlying diabetes mellitus. Int J Endocrinol (Ukraine) 13(8): 618-623.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...