Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Review Article(ISSN: 2641-1687) 
A Rare Case of Penile Schwannomatosis Presenting with Painful Nocturnal Penile Tumescence Volume 3 - Issue 2
Chan Ming Tow1*, Jonathan Tang2, Chan Ming Chun3 and Joe Lee King Chien1
- 1Department of Urology, National University Hospital, Singapore
- 2Department of Pathology, National University Hospital, Singapore
- 3Department of Urology, Tan Tock Seng Hospital, Singapore
Received: October 23, 2021; Published: November 19, 2021
Corresponding author: Chan Ming Tow, Department of Urology, National University Hospital, Singapore
DOI: 10.32474/JUNS.2021.03.000160
Abstract
Background: Penile schwannoma is a rare tumor. They commonly present as an asymptomatic, painless and slow growing
mass. Other presentations include sexual dysfunction, most commonly dyspareunia, followed by erectile dysfunction, abnormal
penile curvature or pain with ejaculation.
Case presentation: A 26-year-old male presented atypically with painful nocturnal penile tumescence, along with multiple
nodules over the dorsal penis. Excision of multiple penile tumors under general anaesthesia was performed and histopathologic
examination revealed benign schwannoma.
Conclusion: Our hypothesis is that the schwannoma lies along the axis of the dorsal penile nerve, and compression of this nerve
occurs during his erection causing pain. However, there are limited presentations of painful erections in penile schwannomas, and
we hope that future studies can help confirm this theory.
Keywords: Penile; schwannoma; painful tumescence; sexual dysfunction
Background
Schwannomas are a form of peripheral nerve tumors made up of neoplastic Schwann cells that typically occur as solitary, encapsulated masses. They can occur throughout the body, but more commonly arise on the head, neck, or flexor surfaces of limbs [1,2]. The tumors are sporadically associated with genetic syndromes such as schwannomatosis and neurofibromatosis or may be the result of therapeutic irradiation [3]. Schwannomas have a low annual incidence of 0.6 per 100,000 people [4]. These are rare and only 27 cases have been reported in literature since it was first described in 1968 [5]. Penile schwannomas are typically asymptomatic, painless and slow growing. Possible presentations include sexual dysfunction, most commonly dyspareunia, followed by erectile dysfunction, abnormal penile curvature, or pain with ejaculation. Our patient presented with painful nocturnal penile tumescence, which is not a well-known presentation of penile schwannomas. There is limited published literature on such cases and hence little is known about this condition (Figures 1&2).
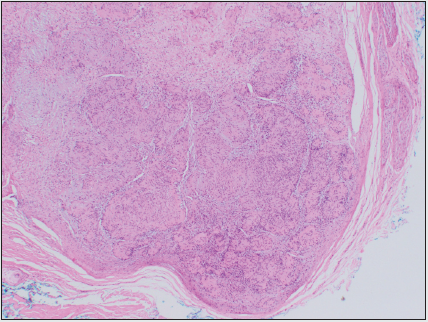
Figure 1: Ultrasound image (longitudinal view) of the penis demonstrates three well-circumscribed, hypoechoic nodules adjacent to the dorsal aspect of the corpus cavernosa.
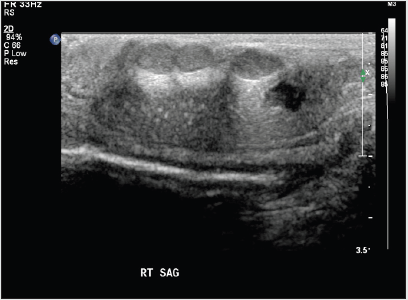
Figure 2: Ultrasound image with power doppler interrogation reveals the presence of internal vascularity within the nodule.
Case Presentation
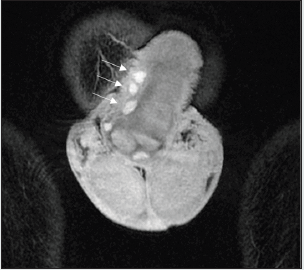
A 26-year-old man with a history of ankylosing spondylitis (HLA B27 gene) and previous circumcision first presented with a oneyear history of recurrent painful nocturnal erections. He had prior consultations with various urologists and did not respond to oral analgesia. The frequency of painful nocturnal erections increased from once per week, to thrice per week over the past year. Each episode of painful nocturnal tumescence lasted approximately five minutes and the patient was often awaken from sleep by the severe pain, which affected his sleep and quality of life (Figure 3). There was no history of priapism, sexual transmitted disease, or genital trauma. There were no persons with known neurofibromatosis in his family. On examination, four lumps could be palpated over the dorsum of the stretched penis. Two were superficial nodules on the distal shaft, with one deep nodule each at the mid shaft and base of the penis. The nodules were 0.5cm or less in diameter and firm in nature. The mid shaft nodule was tender on palpation and correlated with the site of painful nocturnal erections. The penis was otherwise unremarkable and there was neither penile curvature on erection nor any palpable lymph nodes in the femoral or inguinal areas. Nodules or café-au-lait spots were not present in the rest of the body (Figure 4). Over a five-year follow-up, patient developed worsening symptoms with the painful erections occurring twice every night from one episode a week. Physical examination and interval ultrasound imaging demonstrated an increase in the number of nodules from four to five with further growth of the existing nodules. Most noticeably, the right intracavernosal nodule increased from 4 mm to 7 mm in diameter. The patient decided for surgical excision of multiple penile nodules (Figures 5&6).
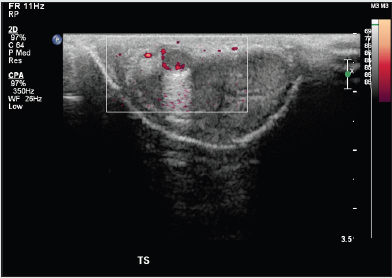
Figure 3: Coronal T2-weighted MR image shows three well-defined T2W hyperintense nodules (arrows) within the penis. These are superficial to the tunica albuginea (arrowhead).
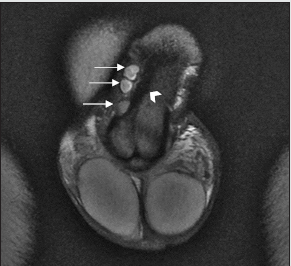
Figure 4: Another T2-weighted hyperintense nodule (arrow) is seen within the right corpus cavernosa.
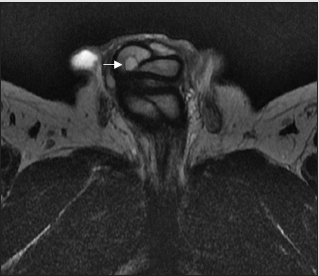
Figure 6: Penile nodules showing low signal intensity with homogenous and avid post contrast enhancement on coronal T1 – weighted MRI.
Investigations
Laboratory findings included normal blood cell counts, chemistries and urinalysis. Initial ultrasound penis showed multiple rounded heterogeneously echogenic nodules in the subcutaneous region of the dorsal penile shaft. The nodules show minimal central and peripheral vascularity. A small cystic lesion with internal echoes is also noted in the corpus cavernosum. The patient initially declined surgical intervention and opted for annual ultrasound imaging (Figure 7). Magnetic resonance imaging (MRI) of the penis performed prior to surgery showed multiple enhancing sub-centimetre nodules in the penile shaft, most of which were superficial. There was a nodule in the right corpus cavernosum, and another in the dorsal midline which disrupts the wall of both corpora cavernosa.
Treatment
Patient underwent excision of multiple penile tumors under general anaesthesia. A circumferential incision was made at the previous circumcision site. The penis was then degloved to its base and the layers dissected down to Buck’s fascia. There were five superficial tumors adherent to the tunica albuginea (two at right distal shaft, two at midshaft, one at base of penis). A deep-seated tumor was located at the right corporal mid shaft. The tumors measured approximately 1-1.5cm in diameter (Figure 8). The cut surface of the tumors was homogenously yellowish with noted feeding vessels. All tumors were excised, and histology was sent from all locations.
Outcome and Follow-Up
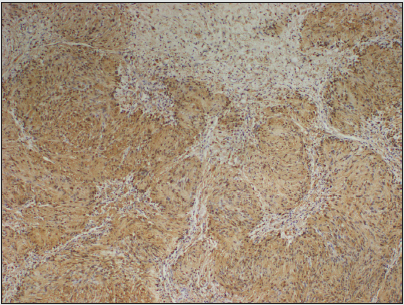
All specimens show similar morphology. The circumscribed and thinly encapsulated nodules were made up of Schwann cells arranged as a mixture of more cellular Antoni A and less cellular Antoni B areas. The more cellular Antoni A areas consists of Schwann cells arranged as short fascicles or parallel rows of nuclear pallisading (Verocay bodies). The less cellular Antoni B areas show a looser myxoid stroma. The nodules are associated with thickened and oedematous nerve fibres, and occasional more plexiform Schwannian areas are seen involving the nerve fibres (Figures 9&10). No high-grade nuclear atypia, increased mitosis or tumour necrosis is seen. On immunostaining, the lesion shows diffuse staining with S-100, which is indicative of Schwannoma. In the follow up consultations over a year after surgery, there was no further nightly painful erections and patient was able to sleep well. On examination there is a small nodularity at mid shaft which is likely due to scar tissue formation. However, the patient did experience difficulty maintaining erection due to discomfort over the surgical site. This was managed well with Viagra 25mg, with an improvement in International Index of Erectile Function score from 8/25 to 19/25. Patient declined genetic testing as he was not keen on childbearing.
Figure 9: Cellular Antoni A areas with short fascicles of Schwann cells and less cellular Antoni B areas with myxoid stroma (H&E stain, 40x magnification).
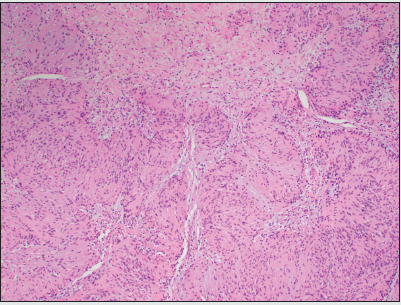
Figure 10: Diffuse and strong S100 expression in the tumour cells (S100 IHC stain, 20x magnification).
Discussion
Schwannomas rarely present with penile pain. There have been postulations made regarding the correlation of symptoms to neuroanatomy. A literature review done by Huang et al. concluded that patients with penile root schwannomas are more prone to symptoms with discomfort or sexual dysfunction (4 of 6) compared with patients with penile shaft schwannoma (7 of 16) or glans schwannoma (2 of 7) [6]. Based on anatomy, penile schwannomas at the mid shaft or glans should originate from the dorsal nerve of the penis, which is the deepest division of the pudendal nerve. The pudendal nerve does pass through the penile root, but there is no clear branching or tracking of the nerve origin of the tumor [7]. Pain may occur in the region of the tumor and any nerve the tumor originates from, but pain may not be specific enough to discern the particular involved nerve. Neurologic deficits of sensory and motor function correspond to the nerve in which the tumor originates or which it is compressing, and as such will often be most useful in localizing the tumor [8,9]. This patient presented with painful nocturnal erections corresponding to the mid shaft schwannoma. Our hypothesis is that the mid shaft schwannoma lies along the axis of the dorsal penile nerve and pain could arise when the nerve is compressed by the schwannoma during full erection. During nocturnal tumescence, the cavernosus arteries dilate, leading to engorgement of the corpora cavernosa and increase of intracorporal pressure. This pushes the schwannoma towards the dorsal penile nerve leading to nerve irritation, compression and pain. Penile schwannomas normally occur at the dorsal penile shaft. However, there have been documented cases where the tumor has infiltrated the glans and prepuce [10]. In such cases, we have to consider other possible diagnoses including benign soft-tissue lesions such as lipoma, fibroma, leiomyoma, Peyronie’s disease, injection-related fibrosis, and rarely malignant sarcomas. Clinical history taking and clinical examination are important, but imaging can aid in narrowing the differentials by locating the plane of the lesion and delineating the mass. Ultrasound examination can demonstrate hypoechoic lesions, and doppler ultrasound can detect hypervascularity. CT scan is rarely used, and mostly performed to exclude metastasis. Schwannomas demonstrate typical MRI features of T1 isointensity to hypointensity, T2 hyperintensity, and postcontrast enhancement. Heterogeneous signal intensity and postcontrast enhancement are suggestive of internal hemorrhage and myxoid/cystic changes [11]. Otherwise, excision biopsy of the tumor would be the gold standard for final diagnosis. Treatment of penile schwannomas is symptomatic, focused primarily on pain management. Complete surgical excision is the recommended treatment for penile schwannomas, with low recurrence rates [1- 10]. This patient recovered well with no signs of recurrence one year postoperatively. Schwannomas of the penis are usually benign, but four malignant variants have been reported in literature. No cases of benign penile schwannoma have been reported to be associated with hereditary diseases [12]. Schwannomatosis is the third major form of neurofibromatosis, and is characterized by a predisposition for schwannomas, in the absence of schwannomas on both vestibular nerves. Its diagnosis is based on a criterion [13]. Most patients present in adulthood with multiple schwannomas and pain, and approximately 20 percent of patients have a family history of schwannomas or schwannomatosis [14]. So far, there have been no confirmed causes of penile schwannoma with schwannomatosis. There is no strong evidence about the correlation between schwannoma and erectile dysfunction [15]. This patient’s postoperative erectile dysfunction is likely due to pain surrounding the surgical wound site. Also, there were no surgical complications other than possible scar tissue formation on the penile shaft.
Conclusion
Schwannomas of the penis are extremely rare and typically present as a solitary, asymptomatic, painless and slow-growing tumor. The rarity in this case is that our patient presented with painful nighttime erections. Based on the penile neuroanatomy, penile schwannomas at the mid shaft should originate from the dorsal nerve of the penis. Our hypothesis is that the schwannoma lies along the axis of the dorsal penile nerve and compression of this nerve occurs during his erection causing pain. However, there are limited presentations of painful erections in penile schwannomas, and we hope that future studies can help confirm this theory.
Declaration
Ethics approval and consent to participate: Not applicable.
Consent for publication: Patient consent for publication has been
obtained.
Availability of data and materials: Not applicable.
Competing interests: The authors declare that they have no
competing interests.
Funding: Not applicable.
Authors’ contributions: All authors have made substantial
contributions in either conception and design, acquisition of
images, analysis and drafting of manuscript.
Acknowledgements
Acknowledgements: Not applicable.
Authors’ information
Authors’ information: Not applicable.
References
- Loeser A, Katzenberger T, Meuller JG, Riedmiller H, Gerharz EW (2007) Solitary schwannoma of the glans penis. Urology 70 (5): 1007.e5-6.
- Marshall J, Lin E, Dogra V, Davis R (2007) Schwannoma of the penis: Preservation of the neurovascular bundle. Urology 70(2): 373e1–373.
- Schulz A, Büttner R, Hagel C, Baader S, Kluwe L, et al. (2016) The importance of nerve microenvironment for schwannoma development. Acta Neuropathologica 132(2): 289-307.
- Hanemann C, Evans D (2006) News on the genetics, epidemiology, medical care and translational research of Schwannomas. Journal of Neurology 253(12): 1533-1541.
- Parra CA (1968) Salitary neurinomas of the glans penis. Dermatologica 137(3): 150-155.
- Huang L, Wang H, Chu Y, Ng K, Chuang C (2020) Clinicopathological Presentation and Management of Penile Schwannoma. Sexual Medicine Reviews 8(4): 615-621.
- Alan J. Wein LRK, Novick AC, Partin AW (2016) Physiology of penile erection and pathophysiology of erectile dysfunction. Lue TF (Ed.) Campbell-walsh Urology 11 ed, 1: 617-618.
- Donner TR, Voorhies RM, Kline DG (1994) Neural sheath tumors of major nerves. J Neurosurg 81(3): 362-373.
- Bhattacharyya AK, Perrin R, Guha A (2004) Peripheral nerve tumors: management strategies and molecular insights. J Neurooncol 69: 335-349.
- Yeh CJ, Chuang WY, Huang ST, Jung SM (2007) Schwannoma of the penis: A report of two cases. Chang Gung Med J 30(6): 555-559.
- Crist J, Hodge JR, Frick M (2017) Magnetic resonance imaging appearance of schwannomas from head to toe: a pictorial review. J Clin Imaging Sci 7: 38.
- Sato D, Kase T, Tajima M, (2001) Penile schwannoma. Int J Urol 8: 87-89.
- Baser ME, Friedman JM, Evans DG (2006) Increasing the specificity of diagnostic criteria for schwannomatosis. Neurology 66(5): 730-732.
- Antinheimo J, Sankila R, Carpén O (2000) Population-based analysis of sporadic and type 2 neurofibromatosis-associated meningiomas and schwannomas. Neurology 54(1): 71-76.
- Algaba F, Chivite A, Rodriguez Villalba R (2003) Schwannoma of the penis. J Androl 24: 651-652.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...