Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1373
Research ArticleOpen Access
Risk Factors for Severe Hemorrhage Requiring Blood Transfusion Associated With Percutaneous Nephrolithotomy: A Systematic Review and Meta-Analysis Volume 2 - Issue 5
Kaisheng Yuan, Ruiqi Zeng, Yongxi Tang, Biao Weng, Pengteng Deng, Huiqian Liu, Ning Wang, Hang Liu*
- Department of Urology, The First Affiliated Hospital of Chongqing Medical Universitya, People’s Republic of China
Received:June 17, 2021; Published:June 24, 2021
Corresponding author:Hang Liu, Department of Urology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, 400016, People’s Republic of China
DOI: 10.32474/LOJPCR.2021.02.000146
Abstract
Purpose: The aim of this meta-analysis was to systematically assess the risk factors for severe hemorrhage requiring blood transfusion associated with percutaneous nephrolithotomy, so that the urologist can prevent the occurrence of severe bleeding as soon as possible.
Materials and Methods: PubMed, Embase and The Cochrane Library were searched to collect the case-control studies on risk factors for severe hemorrhage requiring blood transfusion associated with percutaneous nephrolithotomy (PCNL) through Nov. 9, 2020. Eligible data was screened, extracted, and the risk of bias assessed independently by two qualified investigators. We then calculated the odds risks (ORs) and corresponding 95% confidence intervals (CIs) to assess the relationships between risk factors and severe hemorrhage requiring blood transfusion associated with PCNL.
Results: Eight case-control studies involving 5,974 patients were screened. In this meta-analysis, the risk factors were extracted as follow: gender, hypertension, diabetes mellitus, multiple tracts, staghorn calculi, previous PCNL, grade of hydronephrosis (moderate and severe), calyx of puncture (lower, middle, upper, multiple calices). Among them, diabetes mellitus (95% CI: 1.13 – 3.22, OR = 1.90, P = .016), multiple tracts (95% CI: 2.28 – 7.02, OR = 4.00, P = .000), staghorn calculi (95% CI: 1.34 - 4.08, OR = 2.34, P = .003), upper calyx (calyx of puncture) (95% CI: 0.40 - 0.86, OR = 0.59, P = .006), multiple calices (calyx of puncture) (95% CI: 1.79 - 3.20, OR = 2.39, P = .006) were statistically significant (all P < 0.05).
Conclusions: Our meta-analysis showed that diabetes mellitus, multiple tracts, staghorn calculi, multiple calices (calyx of puncture) are risk factors for severe hemorrhage requiring blood transfusion associated with PCNL, so we should focus on their prevention. Moreover, upper calyx (calyx of puncture) is a protective factor, the urologist may choose upper pole access as percutaneous nephrolithotomy tract to minimize intraoperative and postoperative blood loss
Keywords: Risk Factors; Blood Transfusion; Percutaneous Nephrolithotomy (PCNL); Meta-Analysis
Introduction
All over the world, urolithiasis is a highly prevalent and common urological disease. About 11 percent of men and 7 percent of women suffer from diseases such as urolithiasis in their lifetime, placing a huge financial burden on the global health system [1,2]. Since Fernstrom and Johansson introduced PCNL for the first time in 1976, PCNL has been widely used in the treatment of large renal stones because PCNL greatly improves the stone-free rate and reduces the number of readmission [3]. At present, the EAU guidelines and other guidelines recommend that the usual indications for PCNL are stones larger than 20 mm in diameter, staghorn, partial staghorn calculi staghorn calculi and 1-2cm stones in the lower pole [4-6]. Even with experienced surgeons, up to 7% of cases have major complications. Severe bleeding is the most common complication of PCNL, and blood transfusion rate vary from 1% to 10%. If conservative treatment is in-effective, vascular embolization or even nephrectomy is needed to stop bleeding [7,8]. At present, Li et al. published a meta-analysis about risk factors for hemorrhage requiring embolization after percutaneous nephrolithotomy. They have found that urinary tract infection, diabetes mellitus, staghorn stone, and multiple tracts were risk factors for severe bleeding after PCNL requiring embolization [9]. However, only 0.6% - 2.6% of PCNL patients complicated with severe bleeding need vascular embolization. In addition, most PCNL patients complicated with severe bleeding can be cured only by conservative treatments such as blood transfusion, so it is also essential to identify the overall risk factors for severe hemorrhage requiring blood transfusion associated with PCNL [8]. Now more and more doctors from home and abroad are studying the prevention and treatment of intraoperative and postoperative hemorrhage in PCNL. At the same time, there are few high-quality retrospective analysis of risk factors for severe hemorrhage requiring blood transfusion associated with PCNL. And the conclusions of many studies are also unrepresentative. Therefore, a metal - analysis is needed to review systematically and analyze the risk factors for severe hemorrhage requiring blood transfusion associated with PCNL, which can provide a theoretical basis for urologists to evaluate the risk factors for severe hemorrhage requiring blood transfusion associated with PCNL.
Materials And Methods
Literature search
A comprehensive literature retrieval was guided by combining MeSH terms and free terms independently by two investigators in PubMed, Embase and The Cochrane Library with a cutoff date of Nov.9, 2020. Any disagreement was verified with a third investigator to resolve the dispute. Besides, the special literature was supplemented by literature tracing and manual retrieval.
The retrieval strategy is as follows (in PubMed):
a) percutaneous nephrolithotomy [Title/Abstract]
b) PCNL [Title/Abstract]
c) Nephrolithotomies, Percutaneous [Title/Abstract]
d) Percutaneous Nephrolithotomies [Title/Abstract]
e) Percutaneous Nephrolithotomy [Title/Abstract]
f) #1 or #2 or #3 or #4 or #5
g) hemorrhage [Title/Abstract]
h) hemorrhages [Title/Abstract]
i) bleeding [Title/Abstract]
j) #7 or #8 or #9
k) factor [Title/Abstract]
l) factors [Title/Abstract]
m) risk [Title/Abstract]
n) risks [Title/Abstract]
o) #11 or #12 or #13 or #14
p) #6 and #10 and #15
Inclusion and exclusion criteria:
Studies meeting the predetermined criteria were included:
a) The included literature was the analysis of risk factors for severe hemorrhage requiring blood transfusion associated with PCNL, and the original data was reported.
b) The design type of the literature was case-controlled.
c) In each study, risk factors were defined and quantified in roughly the same way.
d) The language of literature was English.
Exclusion criteria included:
(1) The risk factors in the studies did not include the risk factors that we needed.
(2) The studies were non-case-control studies, systematic reviews, case reports, and repeated cases.
(3) The literature lacks original data and cannot be converted into ORs, SD value and 95%CIs.
(4) NOS score < 6.
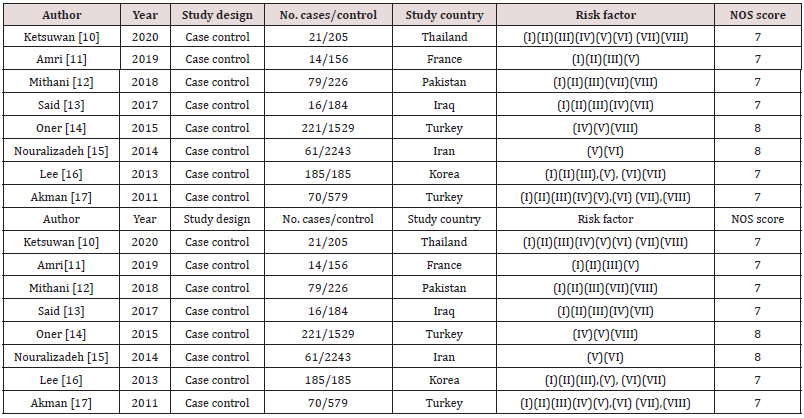
Data extraction and methodological quality assessment:
According to the inclusion and exclusion criteria, we screened out all the literatures that met the criteria. Two investigators took a same standardized information collection table to extract the required data from the eligible literature. Any disagreement was verified with a third investigator to resolve the dispute. The following data were extracted from all eligible studies: first author’s name, publication year, study design, number of cases/control, country, risk factors. During the process of data extraction, if there is any missing data, contact its author for more comprehensive data. The Newcastle - Ottawa Scale (NOS) was used for assessing the methodological quality of the included studies. This tool comprises three broad categories (selection of controls and cases, comparability and exposure), and scores of 0 - 4, 0 - 2, and 0 - 3 are assigned for these three categories, respectively. NOS scores ranged from 0 to 9 stars, with 6 - 9 stars, 4 - 5 stars, and 1 - 3 stars corresponding to high, medium, and low quality, respectively. Our included studies is larger than 6 stars generally. References with less than 6 stars will be excluded. The main characteristics of the included studies [10-17] and the final results of the methodological quality are shown in Table 1.
Risk factors: (I) gender; (II) hypertension; (III) diabetes mellitus; (IV) multiple tracts; (V)staghorn calculi; (VI) previous PCNL; (VII) grade of hydronephrosis (moderate and severe); (VIII) Calyx of puncture (lower, middle, upper, multiple calices).
Statistical Analysis
All statistical analyses were performed using Stata15.1 software, and the ORs and 95%CIs of the included risk factors were combined quantitatively to determine the statistical correlation between the risk factors and severe hemorrhage requiring blood transfusion associated with percutaneous nephrolithotomy. The x 2 and the I 2 test were used to assess the heterogeneity among studies. When I 2 < 50% or P > 0.05, the results showed that there was no homogeneity among studies and a fixed - effects model was used. For significant heterogeneity among studies ( I 2 ≥ 50% or P ≤ 0.05), the random - effects model was applied. The stability of the results was assessed with the sensitivity analysis.
Results
Literature retrieval
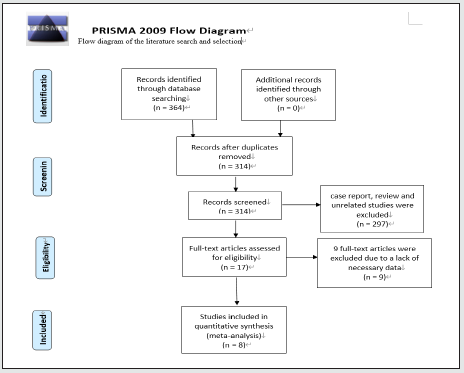
A total of 364 literatures were preliminarily included through searching. After the exclusion of repeated literatures, case reports, reviews, irrelevant literatures and other literatures, there were 17 studies remained. Finally, 8 studies were included while the other 9 studies were excluded after further review because of a lack of important data. The literature screening process and results are shown in the Figure 1 [18].
Characteristics of included literature
Eight of the included articles published during 2011 - 2020 included a total of 5,974 patients with PCNL, among which 667 required blood transfusion, and 5,307 didn’t require blood transfusion. The risk factors that were finally included were gender, hypertension, diabetes mellitus, multiple tracts, staghorn calculi, previous PCNL, hydronephrosis (moderate and severe), calyx of puncture (lower calyx, middle calyx, upper calyx, multiple calices).
Analysis of results
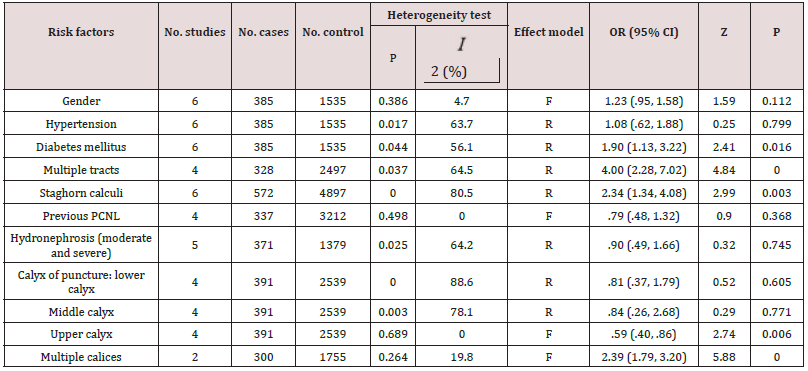
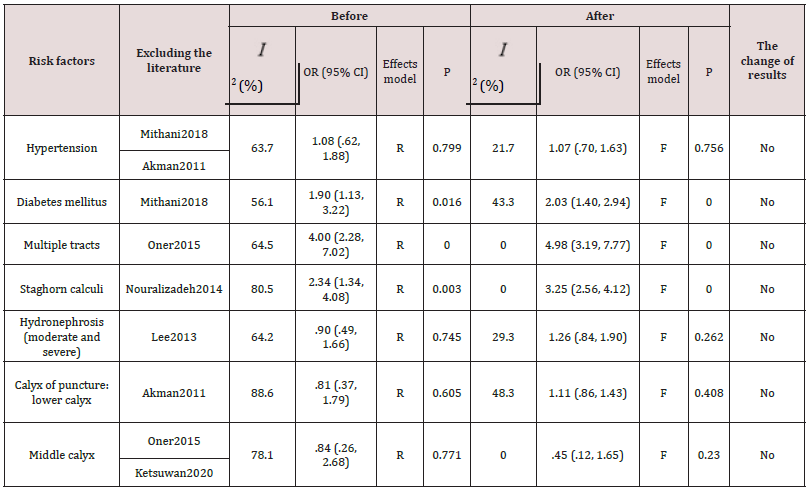
Of the 11 included risk factors, the results showed that 5 of them were related to severe hemorrhage requiring blood transfusion associated with PCNL, with statistically significant differences (P < 0.05). After using the heterogeneity test, only gender, previous PCNL, and calyx of puncture (upper calyx, multiple calices) were found no heterogeneity among the 11 risk factors ( I 2 < 50% or P > 0.05). Therefore, a fixed - effects model was selected for meta - analysis. It was found that all the 7 factors such as hypertension, diabetes mellitus, multiple tracts, staghorn calculi, hydronephrosis (moderate and severe), calyx of puncture (lower calyx, middle calyx) had heterogeneity ( I 2 ≥ 50% or P ≤ 0.05), so the random - effects model was selected. The overall results are shown in the Table 2. Sensitivity analysis was conducted for risk factors with heterogeneity, and statistical analysis was performed again after excluding the sources of heterogeneity. There was no significant change compared with the previous merger results, indicating that the included studies were stable, and the results were reliable, as shown in the Table 3.
Risk factors affecting severe hemorrhage of PCNL Gender
Female served as the case group and male as the control group. Six studies [10-13,16,17] described the correlation between gender and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is low [P = .386, I 2 (%) = 4.7]. There was no statistically significant difference between gender and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: .95 - 1.58, OR = 1.23, P = .112).
Hypertension
Six studies [10-13,16,17] described the correlation between hypertension and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is high [P = .017, I 2 (%) = 63.7], and no statistically significant difference was found between hypertension and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: .62 - 1.88, OR = 1.08, P = .799). The sensitivity analysis showed that heterogeneity existed in Mithani2018 and Akman2011. After excluding them, the heterogeneity was significantly reduced [ I 2 (%) = 21.7], and the results were still not significantly changed (95% CI: .70 - 1.63, OR = 1.07, P = .756).
Diabetes mellitus
Six studies [10-13,16,17] described the correlation between diabetes mellitus and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is high [P = .044, I 2 (%) = 56.1], and statistically significant difference was found between diabetes mellitus and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: 1.13 - 3.22, OR = 1.90, P = .016). As shown in the Figure 2. The sensitivity analysis showed that heterogeneity existed in Mithani2018. After excluding it, the heterogeneity was significantly reduced [ I 2 (%) = 43.3], and the results were still not significantly changed (95% CI: 1.40 - 2.94, OR = 2.03, P = .000). As shown in the Figure 3.
Figure 2: Forest plot: effect of diabetes mellitus for severe hemorrhage requiring blood transfusion associated with PCNL.
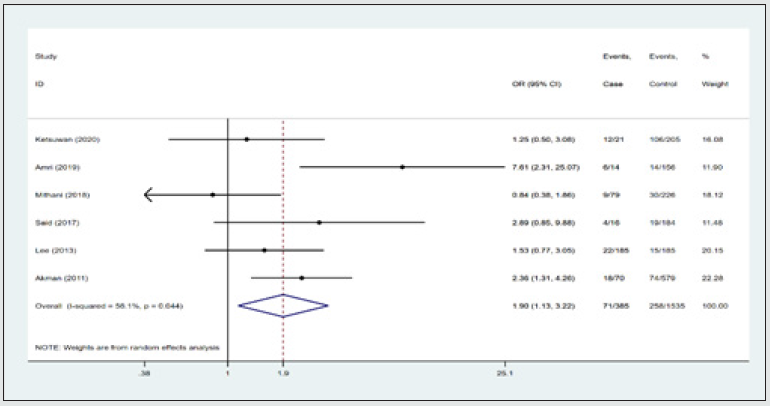
Figure 3: Forest plot: effect of diabetes mellitus for severe hemorrhage requiring blood transfusion associated with PCNL.
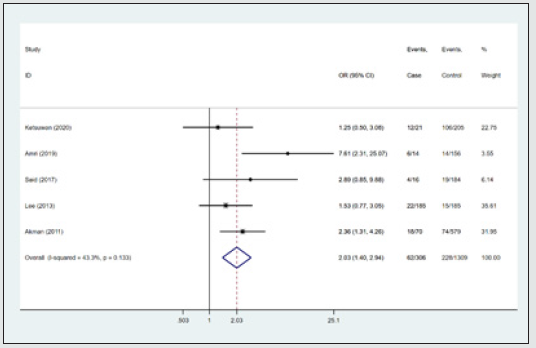
Multiple tracts
Four studies [10,13,14,17] described the correlation between multiple tracts and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is high [P = .037, I 2 (%) = 64.5], and statistically significant difference was found between multiple tracts and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: 2.28 - 7.02, OR = 4.00, P = .000). As shown in the Figure 4. The sensitivity analysis showed that heterogeneity existed in Oner2015. After excluding it, the heterogeneity was significantly reduced [ I 2 (%) = .0], and the results were still not significantly changed (95% CI: 3.19 - 7.77, OR = 4.98, P = .000). As shown in the Figure 5.
Figure 4: Forest plot: effect of multiple tracts for severe hemorrhage requiring blood transfusion associated with PCNL.
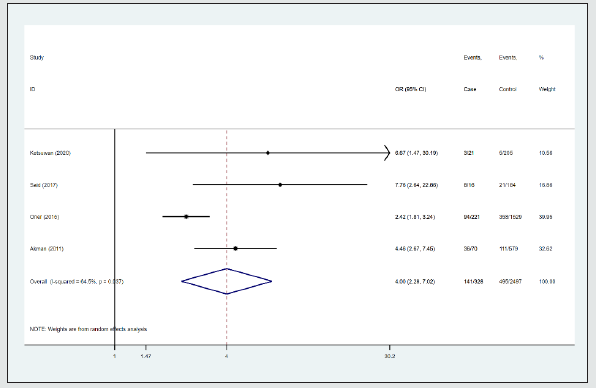
Figure 5: Forest plot: effect of multiple tracts for severe hemorrhage requiring blood transfusion associated with PCNL.
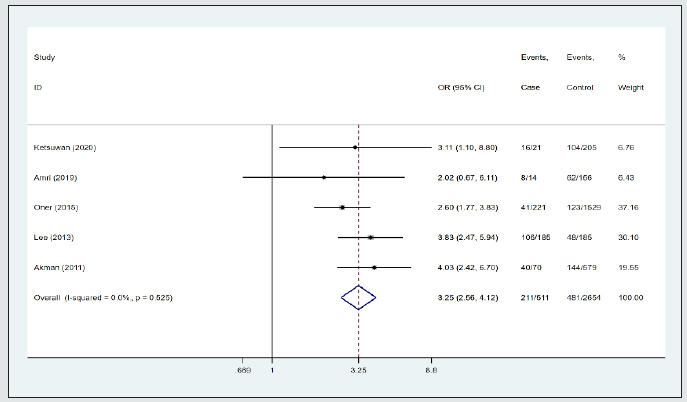
Staghorn calculi
Six studies [10,11,14-17] described the correlation between staghorn calculi and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is high [P = .000, I 2 (%) = 80.5], and statistically significant difference was found between staghorn calculi and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: 1.34 - 4.08, OR = 2.34, P = .003). As shown in the Figure 6. The sensitivity analysis showed that heterogeneity existed in Nouralizadeh2014. After excluding it, the heterogeneity was significantly reduced [ I 2 (%) = .0], and the results were still not significantly changed (95% CI: 2.56 - 4.12, OR = 3.25, P = .000). As shown in the Figure 7.
Figure 6: Forest plot: effect of staghorn calculi for severe hemorrhage requiring blood transfusion associated with PCNL.
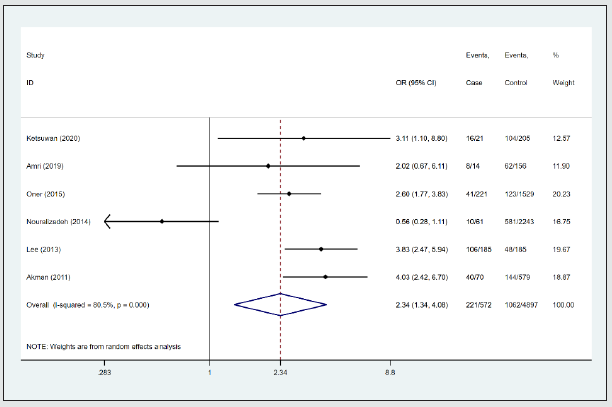
Figure 7: Forest plot: effect of staghorn calculi for severe hemorrhage requiring blood transfusion associated with PCNL.
Previous PCNL
Four studies [10,15-17] described the correlation between previous PCNL and P severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is low [P = .498, I 2 (%) = .0]. There was no statistically significant difference between previous PCNL and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: .48 - 1.32, OR = .79, P = .368).
Hydronephrosis (moderate and severe)
Five studies [10,12,13,16,17] described the correlation between hydronephrosis (moderate and severe) and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is high [P = .025, I 2 (%) = 64.2], and no statistically significant difference was found between hydronephrosis (moderate and severe) and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: .49 - 1.66, OR = .90, P = .745). The sensitivity analysis showed that heterogeneity existed in Lee2013. After excluding it, the heterogeneity was significantly reduced [ I 2 (%) = 29.3], and the results were still not significantly changed (95% CI: .84 - 1.90, OR = 1.26, P = .262).
Calyx of puncture (lower calyx)
Four studies [10,12,14,17] described the correlation between calyx of puncture (lower calyx) and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is high [P = .000, I 2 (%) = 88.6], and no statistically significant difference was found between hydronephrosis (moderate and severe) and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: .37 - 1.79, OR = .81, P = .605). The sensitivity analysis showed that heterogeneity existed in Akman2011. After excluding it, the heterogeneity was significantly reduced [ I 2 (%) = 48.3], and the results were still not significantly changed (95% CI: .86 - 1.43, OR = 1.11, P = .408).
Calyx of puncture (middle calyx)
Four studies [10,12,14,17] described the correlation between calyx of puncture (middle calyx) and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is high [P = .003, I 2 (%) = 78.1], and no statistically significant difference was found between calyx of puncture (middle calyx) and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: .26 – 2.68, OR = .84, P = .771). The sensitivity analysis showed that heterogeneity existed in Oner2015 and Ketsuwan2020. After excluding them, the heterogeneity was significantly reduced [ I 2 (%) = .0], and the results were still not significantly changed (95% CI: .12 – 1.65 OR = .45, P = .230).
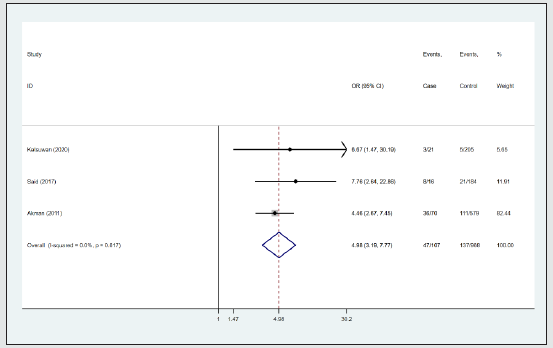
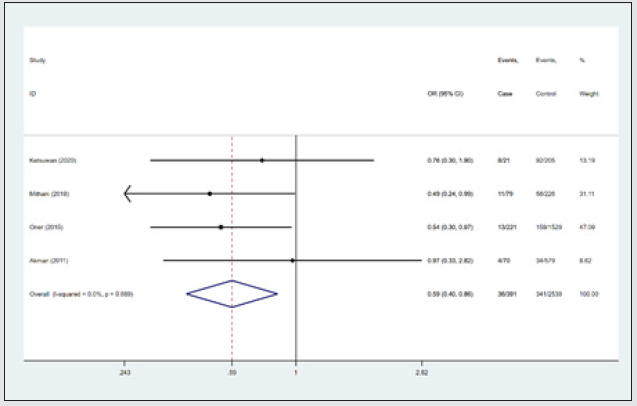
Calyx of puncture (upper calyx)
Four studies [10,12,14,17] described the correlation between calyx of puncture (upper calyx) and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is low [P = .689, I 2 (%) = .0]. There was statistically significant difference between calyx of puncture (upper calyx) and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: .40 – .86, OR = .59, P = .006). Calyx of puncture (upper calyx) is a protective factor for severe hemorrhage requiring blood transfusion associated with PCNL because of OR < 1. As shown in the Figure 8.
Figure 8: Forest plot: effect of calyx of puncture (upper calyx) for PCNL associated with severe hemorrhage.
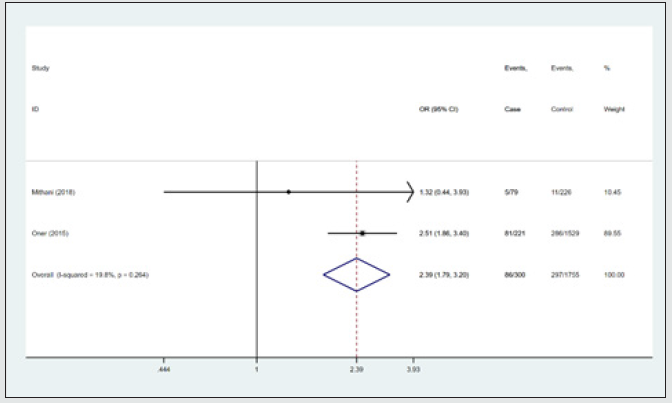
Calyx of puncture (multiple calices)
Two studies [12,14] described the correlation between calyx of puncture (multiple calices) and severe hemorrhage requiring blood transfusion associated with PCNL, heterogeneity is low [P = .264, I 2 (%) = 19.8]. There was statistically significant difference between calyx of puncture (multiple calices) and severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: 1.79 – 3.20, OR = 2.39, P = .000). As shown in the Figure 9.
Figure 9: Forest plot: effect of calyx of puncture (multiple calices) for PCNL associated with severe hemorrhage.
Discussion
PCNL is the preferred surgical method for complex kidney stones, but it may face a series of complications such as pain, fever, severe bleeding and infection during and after PCNL. Severe bleeding is the most common complication, it affects the prognosis of patients and may lose kidney. It is helpful for patients to discern correctly risk factors for severe hemorrhage requiring blood transfusion associated with PCNL. Because we can prevent risk factors as early as possible. A lot of the literature had shown that women, hypertension, diabetes mellitus, multiple tracts, staghorn calculi, previous PCNL, hydronephrosis (moderate and severe) and multiple calices puncture may be the risk factors for severe hemorrhage requiring blood transfusion associated with PCNL, but some scholars have different opinions on them. Eight case-control studies involving 597,4 patients were included. The NOS score of the included literature was 7 for 6 papers and 8 for the other two papers. The overall quality of the included literature is high, and it has certain reference value, ultimately showing that diabetes mellitus, multiple tracts, staghorn calculi, multiple calices (calyx of puncture) are found to be the risk factors for severe hemorrhage requiring blood transfusion associated with PCNL, while upper calyx is their protective factor.
Through the analysis of 6 studies [10-13,16,17], it was found that the probability of severe hemorrhage requiring blood transfusion associated with PCNL in diabetic patients was 2.03 times higher than the control group. Among them, only Akman2011 showed significant statistical difference between diabetes mellitus and severe hemorrhage requiring blood transfusion associated with PCNL (P < 0.05), and the results of other studies were negative. We think this is due to the small sample size. Long-term hyperglycemia will affect the whole vascular system and lead to microvascular lesions, which can easily lead to hemorrhage after renal trauma, providing a theoretical basis for severe hemorrhage requiring blood transfusion associated with PCNL in diabetic patients [19]. In the treatment of long-distance stones or staghorn stones, multiple tracts are often required for the treatment of stones due to the rigid nature of nephroscope. At the same time, it is easy to cause the damage of renal cortex and calyces, leading to intraoperative or postoperative severe bleeding [17]. In the four references [10,13,14,17], there were significant differences between multiple tracts and severe hemorrhage requiring blood transfusion associated with PCNL, and statistical analysis showed that severe hemorrhage requiring blood transfusion associated with PCNL was four times higher in patients with multiple tracts than the control group. Many studies have now shown that percutaneous nephrolithotomy combined with flexible ureteroscopic lithotripsy (FURS) for the treatment of complex kidney stones makes it possible to manage complex kidney stones through a single tract. Because it can reduce the risk of bleeding from multiple tracts, increase stone - free rate and shorten the hospital stay. In recent years, PCNL combined with FURS had been recognized and implemented by more and more urological surgeons [20].
Staghorn stones were named because they fill the renal pelvis and are shaped like staghorn. According to the condition of filling the pelvis and calyx, the calculi can be divided into complete staghorn calculi and partial staghorn calculi [21]. The American Urological Association suggests that PCNL should be the preferred treatment for staghorn calculi and large renal calculi [22]. Because of the nature of staghorn calculi, we need enlarge renal parenchyma operations to remove extensive stone debris, then it will increase the risk of renal hemorrhage [23]. Based on the combined effect of 6 literatures [10,11,14-17], it was found that the probability of severe hemorrhage requiring blood transfusion associated with PCNL in patients with staghorn calculi was 2.34 times higher than the control group. Staghorn calculi are time - consuming and carry a higher risk of bleeding and infection. There is no need to require high stone free rate deliberately, several lithotripsy should be selected to reduce the risk of bleeding. As for calyx of puncture, statistical analysis of 4 studies [10,12,14,17] found that there was no statistically significant difference between middle or lower calyx and severe hemorrhage requiring blood transfusion associated with PCNL, while upper calyx was a protective factor for severe hemorrhage requiring blood transfusion associated with PCNL (95% CI: .40 – 0.86, OR = .59, P = .006). Oner et al. [14] conducted a retrospective study of 175,0 PCNL patients showed that the risk of bleeding in upper calyx puncture is lower, because it is easier to choose the upper calyx as a puncture pathway. When the upper calyx was chosen to puncture, percutaneous nephroscope can more easily place in the ureter. Lower/middle calyx with UPJ angle is too small, so the thread easy to distort and it is not easy to puncture. Statistical analysis of the studies [12,14] showed that the probability of severe hemorrhage requiring blood transfusion associated with PCNL in multiple calices was 2.39 times higher than the control group. It is well known that multiple calices puncture is more likely to damage renal parenchyma and renal calices funnel than single calyx puncture, greatly increasing the chance of severe hemorrhage associated with PCNL. Clinically, lower calyx puncture is not necessary for PCNL. For some stones located in the upper calyx, upper calyx can be attempted to puncture. For large and complex stones, multi-stage single-calyx can be selected to puncture to minimize the risk of bleeding of multi-calices. We recognize certain limitations of this study. First, this review studied the risk factors of PCNL complicated with severe hemorrhage, but the included literature did not have a uniform standard for the definition of severe hemorrhage requiring blood transfusion, which may lead to inaccurate results of the combined effects. Second, some studies did not include the original data, and there may be some errors in the process of converting data through software. Third, all the included literature are in English, which may not be very comprehensive.
Conclusion
In summary, this meta-analysis was ultimately incorporated into the 8 literature. The results showed that diabetes mellitus, multiple tracts, staghorn calculi, multiple calices (calyx of puncture) are found to be the risk factors for severe hemorrhage requiring blood transfusion associated with PCNL, and upper calyx (calyx of puncture) is found to be their protective factor. In clinical practice, urologists should be on the alert anytime, pay attention to risk factors and intervene as early as possible.
References
- Scales CD, Smith AC, Hanley JM, Saigal CS (2012) Prevalence of Kidney Stones in the United States. Eur Urol 62(1): 160-165.
- Raheem OA, Khandwala YS, Sur RL, Ghani KR, Denstedt JD (2017) Burden of Urolithiasis: Trends in Prevalence, Treatments, and Costs. Eur Urol Focus 3(1): 18-26.
- Fernström I, Johansson B (1976) Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol 10(3): 257-259.
- Kim BS (2015) Recent advancement or less invasive treatment of percutaneous nephrolithotomy. Korean J Urol 56(9): 614-623.
- Kallidonis P, Ntasiotis P, Somani B, Constantinos Adamou, Esteban Emiliani, et al. (2020) Systematic Review and Meta-Analysis Comparing Percutaneous Nephrolithotomy, Retrograde Intrarenal Surgery and Shock Wave Lithotripsy for Lower Pole Renal Stones Less Than 2 cm in Maximum Diameter. J Urol 204(3): 427-433.
- Türk C, Petřík A, Sarica K, Christian Seitz, Andreas Skolarikos, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol 69(3): 475-82.
- Taori R, Chawla A, Kapadia A, Zeeshan BM (2020) Post percutaneous nephrolithotomy bleeding requiring angiographic renal angioembolisation. Is lower pole puncture really safe? Indian Journal of Urology 36(5): S50.
- Seitz C, Desai M, Häcker A, Oliver W Hakenberg, Evangelos Liatsikos, et al. (2012) Incidence, prevention, and management of complications following percutaneous nephrolitholapaxy. Eur Urol 61(1): 146-158.
- Li Z, Wu A, Liu J, Shuitong H, Guangming C, et al. (2020) Risk factors for hemorrhage requiring embolization after percutaneous nephrolithotomy: a meta-analysis. Translational andrology and urology 9(2): 210-217.
- Ketsuwan C, Pimpanit N, Phengsalae Y, Leenanupunth C, Kongchareonsombat W, et al. (2020) Peri-Operative Factors Affecting Blood Transfusion Requirements During PCNL: A Retrospective Non-Randomized Study. Res Rep Urol 12: 279-285.
- Amri M, Naouar S, Khalifa BB, Hmidi N, Salem B, et al. (2019) Predictive factors of bleeding and fever after percutaneous nephrolithotomy. Tunis Medi 97(5): 667-674.
- Mithani MH, Khan SA, Khalid SE, Majeed I, Awan AS, et al. (2018) Predictive Factors for Intraoperative Blood Loss during Percutaneous Nephrolithotomy. J Coll Physicians Surg Pak 28(8): 623-627.
- Said SH, Al Kadum Hassan MA, Ali RH, Aghaways I, Kakamad FH, et al. (2017) Percutaneous nephrolithotomy; alarming variables for postoperative bleeding. Arab J Urol 15(1): 24-29.
- Oner S, Okumus MM, Demirbas M, et al. (2015) Factors Influencing Complications of Percutaneous Nephrolithotomy: A Single-Center Study. Urol J 12(5): 2317-2323.
- Nouralizadeh A, Ziaee SAM, Hosseini Sharifi SH, et al. (2014) Delayed postpercutaneous nephrolithotomy hemorrhage: Prevalence, predictive factors and management. Scand J Urol 48(1): 110-115.
- Lee JK, Kim BS, Park YK (2013) Predictive factors for bleeding during percutaneous nephrolithotomy. Korean journal of urology 54(7): 448-453.
- Akman T, Binbay M, Sari E, Yuruk E, Tepeler A, et al. (2011) Factors affecting bleeding during percutaneous nephrolithotomy: single surgeon experience. J Endourol 25(2):327-333.
- Liberati A, Altman DG, Tetzlaff J, Cynthia Mulrow, Peter C Gøtzsche, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339: b2700.
- Tefekli A, Kurtoglu H, Tepeler K, Karadag MA, Kandirali E, et al. (2008) Does the metabolic syndrome or its components affect the outcome of percutaneous nephrolithotomy? J Endourol 22(1): 35-40.
- Chen YC, Chen HW, Juan YS, Ing-Shiang Lo, Ming Chen Paul Shih, et al. (2019) Management of Large Proximal Ureteral Calculi: A Three-year Multicenter Experience of Simultaneous Supine Percutaneous Nephrolithotomy and Retrograde Ureterolithotripsy. Urol J 16(5): 433-438.
- Mishra S, Bhattu AS, Sabnis RB, Desai MR (2014) Staghorn classification: Platform for morphometry assessment. Indian J Urol 30(1): 80-83.
- Assimos D, Krambeck A, Miller NL, Monga M,Murad MH, et al. (2016) Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART I. J Urol 196(4): 1153-1160.
- Srivastava A, Singh KJ, Suri A, Dubey D, Kumar A, et al. (2005) Vascular complications after percutaneous nephrolithotomy: are there any predictive factors? Urology 66(1): 38-40.