Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5787
Research Article(ISSN: 2637-4692) 
Role of Colposcopy to Detect Genital Infection in Women in Goma City, Democratic Republic of Congo Volume 1 - Issue 3
Roger Paluku Hamuli1 and Mateus Kambale Sahani2*
- 1Department of Research and Diseases Prevention, Centre Medical Hope Goma city, Democratic Republic of Congo
- 2Department of Global Health and Development Faculty of Public Health and Policy, London School of Hygiene & Tropical Medicine, United Kingdom
Received:July 16, 2023; Published:July 21, 2023
Corresponding author: Mateus Kambale Sahani, Department of Global Health and Development Faculty of Public Health and Policy, London School of Hygiene & Tropical Medicine, United Kingdom
Abstract
Colposcopy has gone through multiple transformation from static to dynamic status to serve not only for cervical cancer screening and prevention, but also for other purposes such as STI infection diagnosis and follow-up. It is documented that colposcopy is a better option to diagnose HPV infection than HPV testing which has poor specificity and positive predictive value. There are insufficient studies conducted in Africa showing the value of colposcopy in detecting genital infections in women and particularly in Democratic Republic of Congo (DRC). Colposcopy service is not yet developed in DRC and only a few points of access are available. This study was retrospective and documentary. Data were collected through patients’ files from women attending colposcopy clinic from January 2014 to December 2021 and data were collected from January to May 2022. Analysis was conducted using SPSS v28.0 with both univariate and bivariate analysis. One-Sample p-value and Chi-Square tests were used in the analysis. This study has shown that colposcopy has contributed to detection of genital infection in 42.67% of women who attended the clinic and 29.33% women had asymptomatic infection.
The prevalence of Cervical Intraepithelial Neoplasia (CIN) in Goma city was high (24%) which is close to the country prevalence but far higher than the global average (6.4%) documented in Globo can report of March 2021. The most prevalent micro-organisms are Chlamydia trachomatis followed by Neisseria gonorrhoeae. Age group and marital status do not have influence on genital infection occurrence, but other behavioral factors are to be considered. There is an association between genital infections and the presence of CIN. This is possibly due to co-infection with high-risk HPV genotype that was not explored in this study. In conclusion, colposcopy has added value in detection of genital infection including STI. Colposcopy clinic must be considered as entry point for women that may be included in STI management program and should integrated in the genito-urinary screening for routine check. Partnership with colposcopy clinic is a suggested mechanism to implement STI management project.
Keywords: Colposcopy; genital infection; screening; women
Introduction
Colposcopy was created many decades ago in 1925 in Germany and went through a lot of transformations to reach the modern shape of its use today in gynecology [1,2]. Its use was initially restricted to specialists dealing with cervical pathology to detect cervical cancer. However, the domain has been modernized to the point that it has reached the revolution of being accessible to many healthcare professionals who got training in using the device which was progressively reduced in size. Furthermore, it has reached a dynamic phase making it a mobile medical technique by reducing the size to a portable device. This has allowed colposcopy use to be extended to other purposes than only cervical cancer detection and prevention [3]. It is documented that colposcopy is a good mechanism to detect genital infection in women, and even, for special circumstances in men. This is the case for Human Papillomavirus (HPV) detection for which colposcopy was found the best method compared to HPV testing which has mediocre specificity and positive predictive value. Therefore, improvement to colposcopy accuracy has been suggested [4].
HPV being the most prevalent and persistent sexually transmitted infection (STI) worldwide, a study has shown that colposcopy has contributed to detection of at least one high risk HPV genotype at 87% of women who attended to the clinic with an association with other STI at 17.5% in Italy [5]. It was shown that colposcopy plays a role in detecting, not only genital HPV infection, but also oral and anal genotypes [6]. There is evidence that the high-risk HPV genotypes found at the cervix level correlate with the ones found in the anal canal. A study conducted in England by Stuart Lanham and colleagues has shown the role of colposcopy as a channel to detection of both HPV (high and low risk) and other infections such as Neisseria gonorrhoeae, Chlamydia trachomatis, Epstein-Barr, cytomegalovirus, human herpesvirus. The study has concluded that apart from high-risk HPV genotypes, other detected infections in women attending the colposcopy clinic are not associated with cervical cancer. However, it was found that high grade CIN are frequently associated with mixed infection of moderate risk of HPV and human herpesvirus rather than the highrisk HPV alone.
Colposcopy was found valuable to detect Herpes Simplex Virus 1 and 2 (HSV) in women attending a clinic for cervical cancer screening in Brazil [7]. Samples collected during the colposcopy procedure allowed further investigations and enabled checking of association with the changes in colposcopy findings. The procedure has contributed in detecting HSV-1 for 16% of pregnant women and 30% of non- pregnant women and the HSV-2 detected for 12.3% of pregnant women and 15.5% of non-pregnant women. It was found that only HVS-2 was associated with change in colposcopy results for cervical cancer screening. Another study done in Rome (Italy) has found that colposcopy was a valuable channel to detect genital infections in women by, not only providing the consent of women for detection, but also to collect specimens for PCR testing for micro-organisms responsible for the infections. The study has found no correlation with colposcopy findings. However, multiple infections were detected in different groups with mycoplasma being the predominant organism responsible for infection [8]. It is important to note that colposcopy has brought added value to not only detection of infection, but also to infection treatment and follow-up. A study conducted in England has shown that organisms such as Chlamydia were predominant and have created cervical dysplastic change with high prevalence.
The treatment was monitored by a colposcopy procedure which has shown cytological improvement after the treatment is complete. Another study conducted in England has shown evidence that colposcopy is a valuable mechanism in detecting cervical abnormalities due to infection such genital warts and dysplasia. It increases the confidence and compliance of patients for follow-up and reinforces the patient-doctor relationship. The procedure was shown as an important technique that needs to be integrated in the genito-urinary screening at the first visit as primary colposcopy screening [9]. Despite the value of colposcopy in detecting genital infection and cervical pathologies, there are few studies generated in the African continent in general and particularly in the Democratic Republic of Congo (DRC). It is important to note that colposcopy services are almost not existent in DRC with just a few points of access. Moreover, even where the service can be found, it is likely to be at an earlier stage with few services available to the concerned target [10]. Cervical cancer is a major public health issue worldwide and particularly in D.R. Congo where it is the leading cause of death by cancer. The report from GLOBOCAN of March 2021 shows a prevalence of 28.6% of cervical cancer in DRC, which is much higher than worldwide rate of 6.4% [11,12].
There is evidence that women are not aware of cervical cancer being among the major public health issue in the country. Hence, they are not willing to attend the colposcopy clinic without a prior sensitization campaign. The aim of this study is to inform stakeholders, donors/funders, policy makers, health professionals and women in general of the value of the colposcopy procedure in detecting genito-urinary tract infections in Goma city and the possible partnership that may result from it in planning STI programmes or follow-up. Considering the above aim, our research questions are as follows. First, to what extent has colposcopy contributed in detecting genito-urinary tract infection in Goma city, DRC? Second, has colposcopy added value in detecting symptomatic and asymptomatic infection in women in Goma city, DRC? Third, was there association between the presence of CIN (and other general characteristics) and infections found in women during colposcopy procedure in Goma city, DRC? Our study has focused on women attending the colposcopy clinic at Hope Medical Centre in Goma city.
Methods
Study setting
This study was conducted in Goma city, the capital city of North Kivu province in Democratic Republic of Congo. The city is located between the Kivu Lake in the South and Nyiragongo volcanic mountain in the North. There are up to two million people living in Goma city [13] among them the proportion of women of childbearing age is not known. The city is divided into two health zones, Goma health zone and Karisimbi health zone. The study was conducted at Hope Medical Centre which is in Karisimbi health zone receiving women from all over the city for colposcopy. Hope Medical Centre is the only one colposcopy clinic in the region. It is still a young colposcopy clinic and does not have the full service for cancer diagnosis. Services such pathology and biopsy are not available in the whole North Kivu province. Hence, the clinic uses the “see and treat” principle to apply the Single Visit Approach using the LEEP machine. This allows to save time for both patient and clinician and at the meantime, allows the clinician to avoid loss-to-follow up patients. The clinic proceeds to systematic genital infection screening before the colposcopy process as part of the procedure, with the consent of patients. This allows the clinician to proceed to the treatment of the precancer lesion directly when it is detected for patients without infection. For those who have infection, they have to be healed from their infection before the LEEP procedure.
Study design, data collection, and ethical considerations
This is a retrospective study, documentary and descriptive. Data were collected from patients’ files at the colposcopy clinic of Hope Medical Centre in Goma city. We considered files for participants who came for routine cervical cancer screening from January 2014 to December 2021 and who had urine and/or vaginal swab tests done to systematically search GUTI (Genito-Urinary Tract Infection). The files that did not have record of GUTI were excluded from the study. This study did not include live participants, data was collected only from files. The study was approved by the local IRB and the administration of Hope Medical Centre to access the hospital’s data and archive. Data was collected from January 2022 to May 2022.
Data analysis, statistics, and sample size
The database was created with SPSS software version 28.0 of 2021 and all the variables included in the analysis were categorical. The same software was used to analyse data. We have used both univariate and bivariate analysis. Univariate analysis was used for dependent variables which are those directly related to research questions such presence of infection during colposcopy, symptomatic or asymptomatic patients, presence of CIN. Bivariate analysis was used to link findings to the population characteristics such age group, marital status, and residency. For this study, Onesample p-value test was used for univariate analysis and Chi- Square test for the bivariate analysis. Findings from univariate analysis are represented in bar charts. Those from bivariate analysis are represented in tables. The sample size was calculated using g-power software version 3.1. The following characteristics were considered in calculation: large effect size of 0.5, the level of significance α=0.05, and actual power (level of confidence) of 0.95. The calculation was considered for both central and non-central distributions for Chi-square test with critical X2 of 11.0705. The “goodness-of-fit tests: contingency tables” was the statistical test category for the calculation and the type of power analysis was “A priori: computer required sample size-given α, power, and effect size”. The calculation led to a minimum of 80 participants for the study. However, the authors have decided to increase the sample to 150 participants for good representation. Referencing was managed using EndNote X9 software.
Study limitations
This study has limitations as it is a mini review. It does not consider all aspects of genital infections’ detection through colposcopy procedure. It considered only the presence of infection among women who attended the colposcopy clinic for routine cervix precancer screening. The results were those recorded in the patient’s file and some of the files did not have precise details about the micro-organism responsible for infections – these were recorded as “others” in this study. The clinic runs a simple routine test for infection detection. There is a need for further research to conduct a prospective clinical study with live participants to understand which micro-organisms are prevalent during colposcopy procedures. A big sample size would be preferable for such research. We have tried to explore the reasons why women spend long periods with undiagnosed genital infection, but this was not possible due to lack of such information systematically in the all the patients’ files. Further research is needed to include interviews with concerned women.
Results
Data from 150 women were analysed. The characteristics of the study participants are shown in Table 1. This section presents the main findings of the research: the presence of infection among women attending the colposcopy clinic; symptomatic and asymptomatic women for genital infection; presence of cervix precancer lesions; and types of lesions. The link between the presence of infection and some variables such as age group, marital status, and the presence of CIN is explored too.
General characteristics of study participants
The participants in the study were all women aged from 20 years old. During the study period, no woman between 18 and 19 years old attended the colposcopy clinic for cervical cancer screening. This is mainly due to the perception of women in the community thinking that cervical cancer is disease of old women and sometimes sign of curse and witchcraft. Among the selected participants for our study, 33.3% were married whereas 66.7% were not. Regarding the age groups, 32.7% of our participants were between 20-30 years old, 44.7% between 31-40 years old, 17.3% between 41-50 years old, and 5.3% were older than 50 years old. Regarding the residency, our participants were coming from different neigbourhoods of Goma city. Among them, 21.3% were living in Mabanga North, 24% in Mabanga South, 18.7 in Virunga, 10% in Katoyi, 12.7% in Himbi, 6% in Murara, and 7.3% in Majengo.
Presence of cervix precancer lesions (CIN: Cervical Intraepithelial Neoplasia)
This study showed that 24% of women who attended the colposcopy clinic had CIN against 76% who were negative at the screening. Figure 1 below illustrates this. This percentage is higher than the general cervical rate documented in the Globocan report which is 6.4% (11). It is slightly less than the country rate documented in the Globocan report of March 2021 showing a rate of cervical cancer in Democratic Republic of Congo of 28.6% (10).


This study showed that during the routine check for infection while attending the colposcopy clinic, 57.33% were not infected whereas 42.67% were infected. Suyndromic approach was considered here. The One-Sample p-value test shows no statistically significant difference between women who were infected and women who were not infected. This means the colposcopy has contributed to detecting infection for almost half of women who attended the clinic; p = 0.086 (Figure 2).
Presence of symptomatic and/or asymptomatic genital infection
The study showed that 42.67% of women are infected. Almost two thirds of these infections (in 29.33% of all women) were asymptomatic (i.e., displayed no signs of infection before attending the clinic) while 13.33% of women had symptomatic infections (i.e., had signs of infection before attending). The One-Sample test shows a significant difference between these categories; p < 0.001. This shows that there is sufficient number of infected women who remain ignorant (29.33%), and colposcopy contributes to the diagnosis (Figure 3).
Predominant micro-organisms responsible for infection
We sought to identify the predominant micro-organisms responsible for infection, during the colposcopy procedure. Figure 4 below summarises the findings. It is seen that among the 42.67% women with infection, 14% were infected by Chlamydia trachomatis, 13% by Neisseria gonorrhoeae, 10% by other strains that were not specified in the patients’ files, and 5.33% by Trichomonas vaginalis. The One-Sample test shows a significant difference between these categories, p < 0.0001. This means that the most prevalent microorganism for women attending the colposcopy clinic is Chlamydia trachomatis followed by Neisseria gonorrhoeae. These are sexually transmitted infections and can be asymptomatic in women.


Link between genital infection and age group, marital status, and presence of CIN
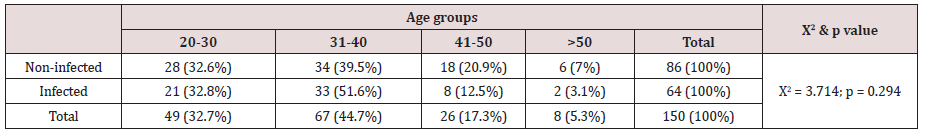
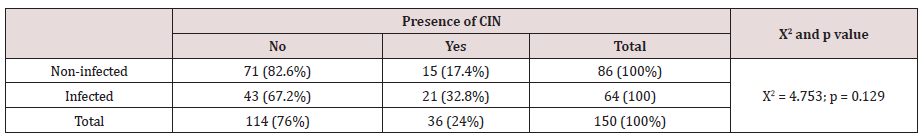
In this study, we explored the connection between the genital infection among women and the following 3 variables: age group, marital status, and presence of CIN. This Table 2 shows the proportion of infected and non-infected women by age group. The Chi-Square test shows no significant difference between these categories. This means that the age group has no influence on the occurrence of infection. The findings showing the link between marital status and infection are presented in Table 3 below. This table shows the proportion of infected and non-infected women by marital status. The Chi-Square test shows no significant difference infected and non-infected for married and non-married women; p = 0.129. This means the marital status (married or un-married) does not impact on the occurrence of infection. It was interesting to explore the link between infection and the presence of CIN as seen in the table below. Table 4 shows the proportions of infected and non-infected women by presence of cervix precancer lesions. The Chi-Square test shows a statistically significant difference; p = 0.029 indicating that infection is associated with the presence of cervical precancer lesions.
Discussion
The rate of cervix precancer in our study is high (24%) and close to what is documented in Globocan report of March 2021 for DRC, 28.6% which is far above the global average (of 6%) (10). Despite the fact that cervical cancer is fully preventable, it is still killing women in DRC and the tendency shows that the situation is far from being under control. This is due to two factors. First, most women are not aware that the disease can be prevented by simply attending colposcopy clinic. Second, policy makers and stakeholders are not making efforts to avail HPV vaccine to the population. This was reported by a local organization (Agir Ensemble) which works closely with the community and was supported by the Union for International Cancer Control (UICC) to implement an awareness project (10). Although it is known that cervical cancer is caused by HPV infection, the country does not still have a system to largely diagnose and control HPV infection. Diagnostic for HPV is not accessible to the wider population and HPV vaccine is not available in the country.
This study has shown that colposcopy has contributed to detecting 42.67% of infections in women attending the clinic and detected almost half of infected women who came for routine cervical cancer screening. We found that 29.33% women were infected with asymptomatic (or hidden) infections (representing almost two thirds of total infections identified), which colposcopy was able to detect. It is certain that these women did not plan to attend the clinic for infection checks and would not have been diagnosed if no colposcopy clinic was available. Studies conducted in Brazil and Italy have found similar findings by detecting STI through colposcopy procedure [5,7,8]. Colposcopy has shown value in detecting STI in Goma city. The most predominant micro organism in genital infection for women who attended the clinic was Chlamydia trachomatis followed by Neisseria gonorrhoeae. These are sexually transmitted infections and usually asymptomatic in women. There is a need to treat the women’s partner to avoid recontamination and interrupt the cycle of transmission.
This finding provides a clear message for stakeholders, actors involved in STI management, and policy makers that colposcopy clinic would be a good partner for detection, prevention, and management of STI. This service also provides an opportunity to detect what is not seen (asymptomatic infection). It is indeed a starting point for the community based STI management programme. A certain number of studies conducted in England has found similar results with Chlamydia trachomatis and Neisseria gonorrhoeae being the predominant micro-organism in women who attended the colposcopy clinic [2,3]. Exploring the connection between age groups and the occurrence of infection, this study has found no connection per se, p = 0.294. As most of the infections are sexually transmitted, there is a need to explore the sexual activity, level of protection during sexual intercourse, and number of partners. These elements were not found in the patients’ files and can be considered among our study limitations. It is important to consider conducting another study to understand this further. The same observations were found for marital status. Married and unmarried women were affected equally.
As stated above, other factors are to be considered to understand the impact on occurrence of genital infections. Importantly, the study has shown that there is a link between the presence of CIN and the genital infections, p = 0.029. This shows that infected women are more likely to develop cervical precancer lesions than those without infection. As most of the infections are asymptomatic, there is a risk of the infection persisting and stay untreated for long period leading to other medical consequences. Again, here comes the value of colposcopy that will not only detect the infection, but also the CIN giving the woman a chance to be fully treated and healed. It is important to know the limitation for our study as no HPV test was done for any of the women who attended the clinic. There is a possibility of co-infection with HPV that was not explored in this study. A study conducted in Italy has shown that colposcopy has allowed detection of HPV infection combined with other STI which may have been responsible cervical intraepithelial neoplasia [5]. Another study conducted in England found similar results with co-infection high-risk HPV and other infections [3].
Conclusion
This study has shown the clear importance of colposcopy in detecting genital infection, associated with cervical precancer lesions, in women in Goma city. Almost two thirds of the infections identified by colposcopy were asymptomatic meaning those women would have had no plan for medical checks and their infections would have remained undiagnosed. There is a pressing need to make colposcopy programme a priority in the Democratic Republic of Congo, because of its potential for CIN detection for prevention of cervical cancer which is exceptionally high in DRC, as well as its added value for detecting and monitoring STI and other genital infections. This gives a special message to donors and funders to consider prioritizing projects that enhance colposcopy use for the management of STI and CIN as joint efforts to save women’s lives. Stakeholders and health authorities should consider colposcopy clinics as the best partners to implement their programmes of STI management. Community-based projects to make women aware of the value of colposcopy clinic are needed too. This will stimulate women attending colposcopy clinic more frequently.
Acknowledgements
Special acknowledgement is addressed to the Hope Medical Center Research Team for making available all the needed file for data collection: Jonas P. Kalunga, Neema Mandelene, Anna Kanyere A special thanks to Professor Susannah Mayhew from the London School of Hygiene & Tropical Medicine (LSHTM) for big support and contribution to the editing and comments on the draft. This was non-funded research and has not received any external funding.
References
- Dexeus S, Cararach M, Dexeus D (2002) The role of colposcopy in modern gynecology. Eur J Gynaecol Oncol 23(4): 269-277.
- Dunlop EMC, Garner A, Darougar S, Treharne JD, Woodland RM (1989) Colposcopy, biopsy, and cytology results in women with chlamydial cervicitis. Genitourinary Medicine 65(1): 22-31.
- Lanham S, Herbert A, Basarab A, Watt P (2001) Detection of cervical infections in colposcopy clinic patients. J Clin Microbiol 39(8): 2946-2950.
- Jeronimo J, Schiffman M (2006) Colposcopy at a crossroads. Am J Obstet Gynecol 195(2): 349-353.
- Martinelli M, Musumeci R, Sechi I, Sotgiu G, Piana A, et al. (2019) Prevalence of Human Papillomavirus (HPV) and Other Sexually Transmitted Infections (STIs) among Italian Women Referred for a Colposcopy. Int J Environ Res Public Health 16(24): 5000.
- Nasioutziki M, Chatzistamatiou K, Loufopoulos PD, Vavoulidis E, Tsampazis N, et al. (2020) Cervical, anal and oral HPV detection and HPV type concordance among women referred for colposcopy. Infect Agent Cancer 15: 22.
- Miranda CA, Lima EG, de Lima DB, Cobucci RN, Cornetta Mda C, et al. (2014) Genital infection with herpes simplex virus types 1 and 2 in women from natal, Brazil. ISRN Obstet Gynecol 2014: 323657.
- Pisani S, Gallinelli C, Seganti L, Lukic A, Nobili F, et al. (1999) Detection of viral and bacterial infections in women with normal and abnormal colposcopy. Eur J Gynaecol Oncol 20(1): 69-73.
- Nathan P M, Moss T R (1991) Screening colposcopy in genitourinary medicine. Int J STD AIDS 2(5): 342-345.
- Sahani MK (2011) Cervical Cancer Prevention Campaign Project Final Report-Agir Ensemble (AE). AE Report.
- WHO-IARC (2020) Cancer statistics in Democratic Republic of Congo: WHO-IARC factsheet. Globocan.
- UICC GLOBOCAN 2020 (2020) New Global Cancer Data. UICC News.
- Wembonyama SO, Tsongo ZK, Mukuku O, Murabazi J, Bahire CM, et al. (2022) Determinants of knowledge, attitudes, and preventive practices for COVID-19 infection in Goma, DRC. Advances in Health and Behavior 6(1): 242-252.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...