Lupine Publishers Group
Lupine Publishers
Menu
Research Article(ISSN: 2770-5447)
Retrograde Recanalization of Chronic Coronary Occlusions Volume 1 - Issue 3
Furkalo SN*
- Department of Endovascular and Angiography, National Institute of Surgery and Transplantology AMS Ukraine, Heart Center of the Ministry of Health of Ukraine, Ukraine
Received: July 10, 2018; Published: July 26, 2018
Corresponding author: Furkalo SN, Department of Cardiology, Heart Center of the Ministry of Health of Ukraine, Ukraine
DOI: 10.32474/ACR.2018.01.000111
Abstract
Chronic coronary occlusion (CTO) is fixed at 1 in 5 patients who underwent cardiac catheterization. Recanalization of chronic coronary occlusions is one of the most difficult for the technical performance of interventional procedures. Successful recanalization CTO associated with better survival compared to patients where the procedure of recanalization of occlusion was not successful. Thus, potential candidates for retrograde recanalization of chronic occlusions of coronary arteries may be: patients after a failed attempt of recanalization with clear indications and motivated to implement PCI; refractory angina with CTO of native coronary arteries after CABG; single-vessel coronary artery disease - RCA or the LAD with preserved left ventricular function and preserved kidney; patients with multivessel disease and related comorbidity, which does not allow to perform coronary artery bypass surgery. From 2007 to the present time we have carried out 125 of retrograde recanalization of chronic occlusions of coronary arteries with a total efficiency of 66.4%. Our data suggest that CTO intervention most often used in LAD - 50% of the RCA - 41.7%, and LCx - in 8.3% of cases. It was succesfull method in CTO cases of RCA - in 86.6% of cases, LAD - in 66% of patients and occlusion and in case of Cx CTO recanalization was succesfull in only 2 patients. Septal collaterals with retrograde approach used in most cases- 101 patients, epicardial collaterals - in 19 cases, and in 4 cases of retrograde access served venous bypass and one mammary coronary bypass – to the LAD.
Keywords: Ischemic heart disease; Chronic coronary occlusion; Coronary stenting; Collateral circulation; Retrograde recanalization of coronary occlusions
Introduction
Chronic coronary occlusion (SRT) is recorded in 1 of 5 patients who underwent cardiac catheterization. Interventional interventions in patients with IHD with chronic coronary occlusions are among the most difficult for technical implementation of interventions [1-4]. The main obstacles for the introduction of SRT revascularization programs in the clinic are the issues of clinical feasibility (determining the viability of the myocardium in the zone of the perfused artery), the cost of the expendable material, the time of the operation, the need for additional access, etc. [2]. Analyzing data from the National Cardiovascular Data Registry (NCDR), the US indicates that the recanalization of SRT was only 4% of all procedures (22,365 of 594,510). And the success of SRT interventions was 59%, whereas in the traditional angioplasty/ stenting group this indicator reached 96%, accompanied by an increased number of complications (1.6% vs. 0.8%) [2,3]. Successful SRT revascularization is associated with a better long-term survival in comparison with cases where the procedure for recanalization of occlusion was not successful [4,5]. The authors also indicate a lower hospital lethality with a successful recanalization of SRT compared to an unsuccessful attempt (0% vs. 1.1%). In modern clinical practice, the operation of recanalization of chronic coronary occlusion involves the operator’s familiarity with the technique of retrograde access. In the event that the “antegrade” approach was unsuccessful, a “retrograde approach” or “retrograde access” to the recanalization of coronary occlusions represents another opportunity for successful myocardial revascularization [6].
However, the retrograde recanalization of the artery takes considerable time and involves several stages. Careful control of operating time is very important to ensure the safety of the procedure. It is advisable to switch to retrograde access no later than 60 minutes after an unsuccessful antegrade attempt, or after 30 minutes of unsuccessful work with a coronary guidewire. The modern concept of the retrograde approach was proposed in 2005 by the outstanding Japanese cardiologist Dr. Osamu Kato [7,8].
Potential Candidates for a Retrograde Approach
Retrograde approach to the recanalization of SRT is a relatively new and constantly improving technique. In comparison with standard antegrade access, additional possibilities for opening an artery are determined by a combination of ante and retrograde access. Traditionally, a complex angiographic pattern for antegrade recanalization (stump with branching off at the occlusion site, intravascular collaterals in the form of the jellyfish head, long> 20mm occlusion, calcification of the occluded segment) is no longer a contraindication for intervention in the case of retrograde access, the number of patients where antegrade recanalization was previously unsuccessful can be successfully operated using a retrograde approach. Thus, potential candidates for the retrograde recanalization of chronic occlusion of the coronary arteries can be:
a) Patients after an unsuccessful attempt at recanalization with obvious indications and motivated to perform PCI refractory angina with SRT of native coronary arteries after CABG.
b) single-vessel coronary artery disease - right coronary artery (PCA) or anterior interventricular artery (LAD) with preserved left ventricular myocardial function and preserved renal function.
c) Patients with multivessel lesions and concomitant comorbidity, which does not allow coronary bypass surgery [9].
Types and Classification of the Retrograde Approach
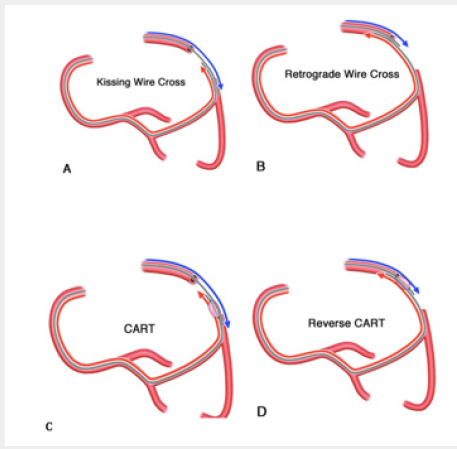
There is a conditional classification of approaches to the retrograde recanalization of the coronary arteries. (Figure 1).
Figure 1: Schematic classification of variants of retrograde recanalization of SRT [7].
A. The technique of kissing wires (kissing wire cross).
B. Direct retrograde wire crossing (retrograde wire crossing).
C and D. Controlled ante-retrograde subintimal recanalization (CART & Reverse CART).
Direct retrograde reanalization by the conductor (Direct retrograde crossing)
a) Can be considered the simplest and most gentle method of retrograde recanalization of chronic coronary occlusion. According to available data, this option of recanalization is possible in approximately 30% of cases, being the most “comfortable” and non-traumatic for the artery. In this case, the retrograde conductor passes through the lumen of the vessel, without causing a dissection and a subintimal motion.
b) After conducting the collaterals guide to the distal part of the occluded artery, with the support of the microcatheter, the conductor passes through the occlusion and enters the proximal part of the occluded artery (Figure 2).
c) Then the procedure of externalization (see below) is performed and the balloon catheter is recanalized by retrograde conductor. Installation of the stent is carried out in a similar way and as a rule does not cause significant problems.
The technique of kissing wires (Kissing wire crossing)
In this case, an antegrade stage of reanalysis is carried out with conducting a conductor to the site of occlusion of the artery in combination with retrograde advance of the conductor with the support of a microcatheter for collaterals with a distal “cup” of occlusion. Further with the use of specialized recanalization conductors (Giai, filder XT, Ultimate Bros 3, Conquest Pro) occlusion is recanalized either by antegrade conductor or retrograde. If the antegrade conductor successfully moves into occlusion, the retrograde conductor is used as a reference point. If the retrograde conductor is more “successful”, the antegrade is used as a label, the procedure of externalization, angioplasty and subsequent stenting is performed (Figure 3).
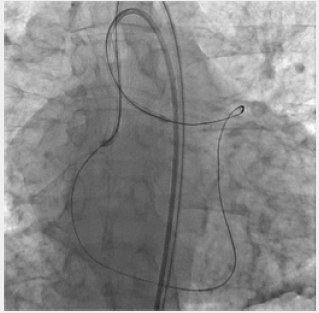
Figure 2: Reocclusion of PKA in a previously implanted stent. The technique of direct retrograde recanalization (direct retrograde crossing).
1. Visualization of the distal parts of the PCA through the system of septal collaterals. 2. Microcatheter “Corsair” allows selective filling of “interventional collaterals”. 3. Conductor and microcatheter in the distal parts of the PCA. 4. Successful conducting of the conductor through occlusion to the antegrade directional catheter. 5. Carrying out the microcatheter into the guide catheter, implementing the “trap” technique and manipulating “externalization”. 6. Stenting and final result.
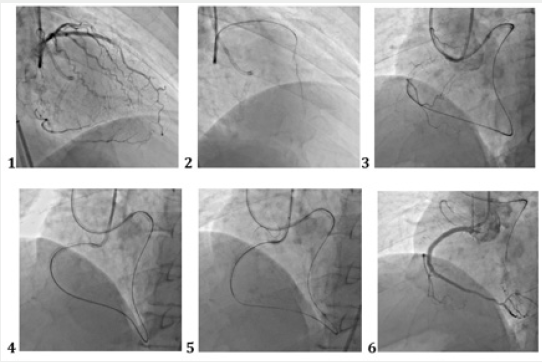
Figure 3: Retrograde recanalization of service stations. The technique of kissing wires (kissing wire crossing). Occlusion LIV. Bifemoral cannulation. From the PCA system, through the septal collaterals, a conductor “Sion” and a microcatheter “Corsair” were conducted. The microcatheter “Finecross” and the conductor “filder Fc” are antegradeally applied.
The CART and Reverse CART methodology
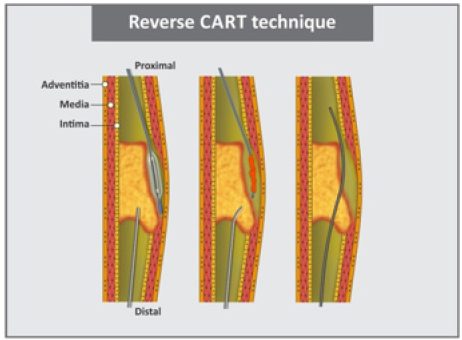
Controlled ante-retrograde subintimal recanalization. When the microcatheter and the conductor through the collaterals are carried to the distal fibrous plate, in most cases the tip of the conductor “migrates” to the sub-sinimal space. In this position, the conductor can move quite easily, not feeling much resistance. To perform the procedure, the antegrade conductor at this time also advances in the subintimal space until the conductors are in the same plane [10]. Once the conductors are in the same plane, however, as a rule in different sub-sinimal spaces, balloon angioplasty is performed. The lumen formed by the balloon-catheter, in the optimum case, should connect the two conductors in the same space and facilitate the conductor into the true lumen (Figure 4).
The balloon-catheter and angioplasty can be performed both on a retrograde conductor, and then the CART technique will be performed, or on the antegrade conductor. In this case, the Reverse CART technique is used. In the case of applying the CART technique, the “antegrade” conductor advances into the space created by the “retrograde” balloon. If a more modern Reverse CART technique is used, the “retrograde” conductor advances into the space created by the “antegrade” balloon (Figure 5). The CART method provided for balloon dilatation of collaterals and a balloon catheter of adequate size for the colaterals, subintimal with subsequent angioplasty. This can combine both conductors in one space and allow the “antegrade” conductor to enter the true lumen of the artery and perform stenting of the coronary artery. With the introduction into clinical practice of the microcatetre “Corsair”, the so-called collateral dilator, the Reverse CART technique almost completely supplanted the CART technique. First of all, in view of the simpler and safer implementation and the absence of the need for dilatation of collaterals. It is necessary to say a few words about the limitation of the technique: if antegrade angioplasty is performed with a balloon catheter, the introduction of contrast into the antegrade catheter should be either extremely limited or completely eliminated until the stent is delivered. Otherwise, the accented introduction of a contrast medium into the dilated segment of the artery can cause the emergence of a spiral dyspnea or hematoma [11].
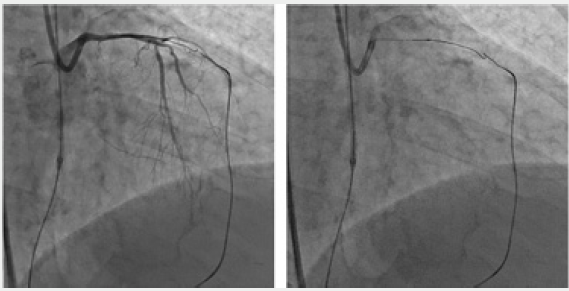
Figure 5: Retrograde reclamation of OSLKA in a patient after CABG. Method Reverse Cart. The balloon-catheter is positioned antegradeally. Retrograde, a microcatheter Corsair and a conductor “Gaia 3” were carried through the shunt to the OB of the LCA.
Collateral Channels
The first and important step in retrograde access is the identification of a suitable collateral pathway. Collaterals are often very thin and convoluted, which makes them easily damaged. When analyzing coronary angiography, preference is given to septal collaterals for the advancement of equipment, the use of epicardial collaterals is also possible, but in the case of epicardial collaterals, the patient will likely have a pericardial tamponade. When choosing a coronary conductor, preference is given to conductors with a low load on the tip of the conductor or so-called “soft” conductors. In most cases, this is Sion, Sion Blue, Filder Fc, (Asahi), Pilot 50 (Abbott). The conductor is promoted with the support of a microcatheter, which not only provides support for the conductor, but can provide contrast medication through the tip of the catheter for visualization or “collateral channel isolation.” Intensive introduction of contrast material into the collateral can lead to damage to the collateral channel, therefore, before visualization it is necessary to obtain “reverse blood flow” through the microcatheter, creating a negative pressure in the syringe attached to the microcatheter. With very thin and non-visualizable collaterals, it is possible to use the Typed Filder XT or Filder XT-R conductor (version with less load on the tip). It should be taken into account that the shape of the tip of the conductor, suitable for entering the collateral, differs from the shape necessary for advancing along the collateral (Figure 6). One of the conductors for easier entry into the collateral can be Filder FC, and then Sion or Sion Black. The latter conductor is characterized by a polymer coating for easier intravascular advancement.
Figure 6: Retrograde recanalization of service stations. The procedure of externalization. Occlusion of PKA. Through the septal collaterals, a conductor and a microcatheter were conducted to the distal part of the PCA, then through the occluded segment to the antegrade operating catheter.
For advancement on collaterals the preference today is given to microcatheters “Corsair” of company Asahi Intecc or “Finecross” of company Terumo. Microcatheter “Tornus” (Asahi Intecc) is used more often as a dilating device than a standard microcatheter. The presence of spiral notches on the tip of the catheter allows him to “twist” into the occluded segment. This property is hardly acceptable when passing collaterals. Previously, when specialized microcatheters were not available, OTW small-diameter balloon catheters were used, but they are less slippery, prone to kink in the crimped sections of the artery, do not have a mark at the tip of the catheter, which creates problems for accurate positioning in vessel occlusion.
The manipulation of the conductor in the collateral channel is different from the progress of the conductor in the occluded segment. The conductor is not force-applied and progressive advancement is made by “soft” rotation, reducing friction and the risk of perforation. If the resistance is felt or the conductor is stopped in the collateral channel, the anatomy of the vessel can be controlled by introducing a contrast into the microcatheter in different projections. Septal, the most commonly used collaterals, are better visualized in the right oblique with cranial or caudal deviation projections, lateral projection.
The Main Materials for the Recanalization of SRT
Guides
There are several differences in the conductors used in the case of chronic coronary occlusions.
a) Polymer coating: it is a plastic “sleeve” made of flexible but hard material that covers the core and covers the tip of the conductor. Based on the presence or absence of the polymer, all conductors are divided into 2 main categories: conductors with a polymeric sheath (by default with a hydrophilic coating) and conductors with a wire coating (with or without hydrophilic properties).
b) Hydrophilic or hydrophobic coating of the conductor, affecting the penetrating ability of moisture / blood.
c) The shape of the tip of the conductor: standard or cone (timer). The latter is successfully used in specialized recanalization conductors, such as filder XT, Conquest Pro, Gaia (all Asahi Intec - Japan), some types of conductors Progress - Abbott - USA.
d) Rigidity of the tip of the conductor, currently measured in grams and determined by the load necessary to bend the tip of the conductor. The softer versions are characterized by a load on the tip in the range of 0.5 to 1 gram. The most rigid, recanalizing conductors are characterized by a load of 12 and even 20 grams.
Microcatheters
With the advent of the microcatheter “Corsair” of Asahi company, the technique of performing the retrograde recanalization of chronic occlusions of coronary arteries has significantly changed and simplified. The ability to safely move the microcatheter to both septal and epicardial collaterals has greatly simplified and expanded the possibilities of the technique. An important feature of Corsair is the exceptional flexibility of the tip of the microcatheter, allowing for progressive advancement through collaterals. Instead of a more complex CART technique, the Reverse CART technique, which does not require the balloon catheter through collaterals to the distal segment of the occluded artery, has become a clinical practice. With the use of the microcatheter “Corsair”, the need for balloon angioplasty of collaterals has disappeared. Previously used OTW cylinders are inferior in comparison with microcatheters. The latter are more flexible, provide greater maneuverability of the conductor in view of greater internal lumen and hydrophilic coating. In addition, the tip of the catheter is well contrasted, which allows it to be visualized in occlusion.
The design of the microcatheter provides a woven base, which is not available for a balloon catheter. This property prevents the kink of the microcatheter in the twisted channel. On the other hand, the microcatheter is more expensive and has no dilatory abilities. Another frequently used microcatheter is Finumross produced by Terumo with lengths of 130 and 150cm, but with the implantation in the clinical practice of the Corsair microcatheter, the frequency of application of Finecross with retrograde access is significantly reduced. However, the hydrophilic coating of the microcatheter, the conical shape and the very low profile may have an advantage in some cases Asahi Intecc, a low-profile microcaratter “Caravel”, with a profile of 1.9F and the preferred application in thin epicardial collateral channels [11], in cases where the advancement of the microcatheter “Corsair” is difficult due to the larger profile, became the next product of Asahi Intecc. A number of other microcatematers “Tornus”, “Venture TM”, “Crusade”, “Twin Pass” can also be used for recanalization of chronic occlusions of coronary arteries, but their use is significantly limited.
The Use of Intravascular Ultrasound (IVUS)
The possibility of visualizing the boundary between media and adventitia, i.e. external elastic membrane is especially important for invasive interventions in SRT. This allows you to visualize the position of the coronary conductor in the occluded segment. Thus, both intralights and subintimal advances in the conductor can be well distinguished, which is critical for both antegrade and retrograde access. In addition, IVUS can help locate the entrance to occlusion in cases where there is no stump of the artery and the presence of a lateral branch. In addition, this study helps to determine the true diameter of the occluded artery, the optimization of stent implantation, etc.
Retrograde Wire Externalization
In the event that the SRT was able to be recanalized by the retrograde conductor and the conductor is in the true lumen, the procedure of externalization is performed. With this specific technique, the retrograde conductor is guided into the antegrade guide catheter. Using the “trap” technique, when a conductor is fixed in the guide catheter using a balloon (2.5mm for 7 and 8F), a retrograde microcatheter is wound in the guide catheter much more quickly and easily. The balloon is blown off and removed, and the conductor changes to a special conductor RG 3 by 300 cm. The special feature of this conductor is its size of 0.10”, which makes it easy to move along the microcatheter and complete the procedure of externalization. Upon completion of this manipulation, a loop is created that closes the antegrade and retrograde catheter and creates very reliable coaxial support for the cylinders and stents.
Own data
The first attempt at retrograde recanalization of chronic coronary occlusion in our clinic was undertaken in 2007. From 2007 to the present, we have performed 125 retrograde approaches to the recanalization of chronic occlusions of the coronary arteries with a total efficiency of 66.4%. As a rule, operations of retrograde recanalization required more operating time, radiation load for both the doctor and the patient, contrast agent (Table 1). The expenditure of contrast medium and the radiation load during the recanalization of the coronary arteries. The introduction of the microcatheter “Corsair”, and later the “Caravel” of the company “Asahi Intecc” into the clinical practice, Japan, the retrograde recanalization has become much simpler. These micro catheaters allowed to expand the patient contingent, the possibility of using epicardial collaterals for equipment. Our data testify, that the efficiency of the operation was 36.3% before and 76.7% after the application of “Corsair”. For the sake of objectivity, it should be noted that lower rates of effectiveness of retrograde recanalization were recorded at earlier stages of implementation of the methodology and a set of experiences. Our data testify that most often we applied the technique for occlusion of LAD with LCA - 50% of cases, PCA - 41.7%, and OB of LCA in 8.3% of cases. It is worth noting that the success of retrograde access differed depending on the location of the SRT.
Table 1: The expenditure of contrast medium and the radiation load during the recanalization of the coronary arteries.
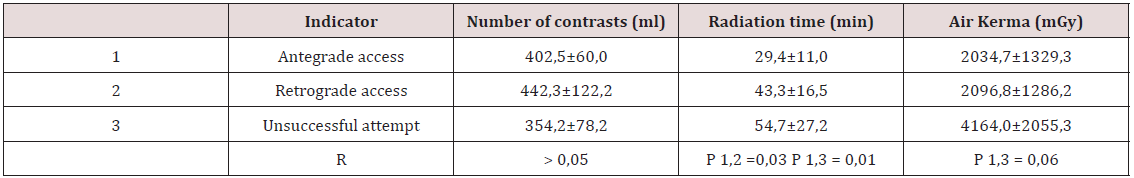
So, the most effective method was with the defeat of PKA - in 86.6% of cases, LAD of LAD - in 66% of patients and with occlusion of RV LC it was possible to achieve recanalization only in 2 patients. Septal collaterals with a retrograde approach were used in most cases - in 101 patients, epicardial collaterals - in 19 cases, in 4 cases, venous and in one case a mammary coronary shunt to LAD of LKA (6) served as retrograde access. The most “successful” for retrograde recanalization were the conductors Filder XT, Filder Fc and Conquest Pro / Conquest Pro 12. Recently, the Ultimate Bros 3 wire was used more often, as well as a new generation of conductors with the unique penetrating ability of the Gaia family from Asahi. Obviously, the success of retrograde recanalization in our series of patients was lower than that in the antegrade series of recanalization’s of chronic occlusions. The main reasons for the failures were:
a) Impossibility of conductor on collaterals.
b) Impossibility of conducting a microcatheter or balloon on collaterals.
c) Impossibility of conducting a conductor through the occluded segment.
According to our data, and this is consistent with the literature data, the application of the retrograde recanalization technique of SRT is associated with a relatively large number of complications. The most frequent of those recorded were trauma of collateral canals, intravasal hematoma, limiting the possibility of retrograde advancement of equipment and reducing the likelihood of recanalization of the artery. One case of coronary artery III of type III was observed during stent implantation, which led to cardiogenic shock and death of the patient.
With the introduction of bioresorbent stents, we have gained some experience in the application of this technology in the event of the recanalization of SRT, including the retrograde approach. The main difficulty of using the above technology is to determine the adequate size of the stent in view of the empty and underfilled occluded coronary artery these cases of standard coronary angiography may not be enough. In such cases, we used methods of intravascular imaging - optical coherence tomography and intravascular ultrasound. In all cases of recanalization of chronic occlusions, we used stents with a drug coating.
Discussion
Recanalization of chronic coronary occlusions is the last frontier for the implementation of technically complete myocardial revascularization. Most patients with IHD, if there is a chronic occlusion, remain on drug therapy or undergo CABG. The introduction of the retrograde recanalization of chronic coronary occlusions into clinical practice made it possible to significantly increase the effectiveness of interventional interventions. In the hands of experienced experts - experts, the effectiveness of opening chronic occlusions reaches 85-90% and even more with a minimum number of complications. With the use of modern technologies and equipment, the efficiency of exclusively antegrade recanalization is 70-85%. Another 10-15% of efficiency can be “added” due to the qualified application of the retrograde approach.
In accordance with modern ideas, using high-tech equipment to begin recanalization of chronic occlusion, it is recommended to apply the antegrade approach. Moreover, if the strategy is changed to a retrograde approach, the antegrade equipment should already be introduced into arterial structures for the possible implementation of the Reverse CART technique. Primarily retrograde access may be justified in cases of wellhead lesions, long occlusions, repeated attempts at recanalization.
References
- Alhejily WA (2013) Retrograde approach to coronary chronic total occlusion via an occluded saphenous bypass graft: a case report. Clin Case Rep 1(2): 54-58.
- Brilakis ES (2011) Percutaneous coronary intervention in native arteries versus bypass grafts in prior coronary artery bypass grafting patients: a report from the National Cardiovascular Data Registry. JACC Cardiovasc Interv 4(8): 844-850.
- Brilakis ES (201) Retrograde recanalization of native coronary artery chronic occlusions via acutely occluded vein grafts. Catheter Cardiovasc Interv 75(1): 109-113.
- Hsu JT (2011) Impact of calcification length ratio on the intervention for chronic total occlusions. Int J Cardiol 150(2): 135-141.
- Joyal D (2010) Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J 160(1): 179-187.
- Michael TT (2012) Role of internal mammary artery bypass grafts in retrograde chronic total occlusion interventions. J Invasive Cardiol 24(7): 359-362.
- Surmely JF, Katoh O, Tsuchikane E, Nasu K, Suzuki T (2007) Coronary septal collaterals as an access for the retrograde approach in the percutaneous treatment of coronary chronic total occlusions. Catheter Cardiovasc Interv 69(6): 826-832.
- Rathore S, Katoh O, Matsuo H (2009) Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv 2(2): 124-132.
- Sianos G (2012) Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention 8(1): 139-145.
- Touma G (2015) Chronic total occlusions. Current techniques and future directions. IJC Heart & Vasculature 7(1): 28-39.
- L Azzalini, P Agostoni, S Benincasa (2017) Retrograde chronic total occlusion percutaneous coronary intervention through ipsilateral collateral channels. JACC: Cardiovascular Interventions 10(15): 1489- 1497.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...