Lupine Publishers Group
Lupine Publishers
Menu
Research Article (ISSN: 2770-5447) 
Dynamics of Blood Pressure During the Development of Neuroleptic Cardiomyopathy Volume 1 - Issue 2
Volkov VP*
- Tver center of judicial examinations, Russia
Received: June 26, 2018; Published: July 13, 2018
Corresponding author: Volkov VP, Tver center of judicial examinations, 170008, Tver A Zavidov St, Russia
DOI: 10.32474/ACR.2018.01.000110
Summary
The study of various clinic aspects of Neuroleptic Cardiomyopathy (NCMP) associated with the side cardiotoxic effect of Antipsychotics (AP) is actual. With the purpose to track dynamics of the Blood Pressure (BP) in the process of development of NCMP data about 78 died patients with schizophrenia (men - 53, women - 25) in whom NCMP is found on autopsy were retrospectively analyzed. At the age of 50 years were 43 persons, 44 died in the first stage of the disease, 12 - in the second one, 22 - in the third one. The conducted research allows to draw the following conclusions:
a) Frequency of this or that option the AP in all stages of NCMP doesn’t depend on the age of patients.
b) In a latent stage significantly prevail hypo and a normotony.
c) In the developed stage steadily normal and labile BP with a tendency to moderate Arterial Hypertension (AH) are equally common.
d) In the terminal stage of NCMP at ¼ patients is observed moderate AH and at 13,6% of patients the expressed stable AH.
e) As a whole, according to own data, in the case of NCMP the frequency of AH is 37.2%.
f) Fluctuations of frequency of occurrence of this or level of BP are connected with various side effects of the AP used in the treatment of schizophrenia.
Keywords: Neuroleptic Cardiomyopathy; Clinical current; Blood pressure
Abbrevations: AH: Arterial Hypertension; NCMP: Neuroleptic cardiomyopathy; AP: Antipsychotics BP: Blood Pressure
Introduction
Neuroleptic cardiomyopathy (NCMP) is one of the most serious vitally dangerous complications of antipsychotic therapy [1-7], due to the side cardiotoxic effect of Antipsychotics (AP) [1,2,4,6- 9]. The disease belongs to the secondary specific toxic (metabolic) dilated cardiomyopathies [1,3,10,11]. Is characterized by diffuse myocardial lesions, a sharp decrease in its contractile function and, as a consequence, development of chronic heart failure [3-6,12]. In its development NCMP passes three clinical stages: I - latent, II - deployed (manifesting) and III - terminal [3,13]. Many aspects of the pathogenesis, morphology, clinic and diagnosis of NCMP are still almost completely unexplored. Among others, it is of practical interest to trace the dynamics of blood pressure (BP) during the development of NCMP. This issue is still without due attention. However, to date, BP is quite informative marker of the functional state of the cardiovascular system, its measurement is usually not difficult, it is a routine method of examination of patients. In order to fill the existing gap at least partially, the present study has been undertaken.
Material and Methods
The history and protocols of autopsies of the dead 78 schizophrenic patients (53 men, 25 women), whose autopsy discovered NCMP, are studied. At the age of 50 years were 43 persons, 44 died in the first stage of the disease, 12 - in the second one, 22 - in the third one. The lethal outcome in the first two stages either came from intercurrent diseases or there was sudden cardiac death of arrhythmogenic origin. In the terminal stage, the immediate cause of death was usually progressive chronic heart failure [3,14]. The dynamics of changes in depending of BP on the age of patients and stage NCMP was traced. The results of the study were processed statistically (computer program “Statistica 6,0”) with the level of significance of differences of 95% and more (p≤0,05).
Results
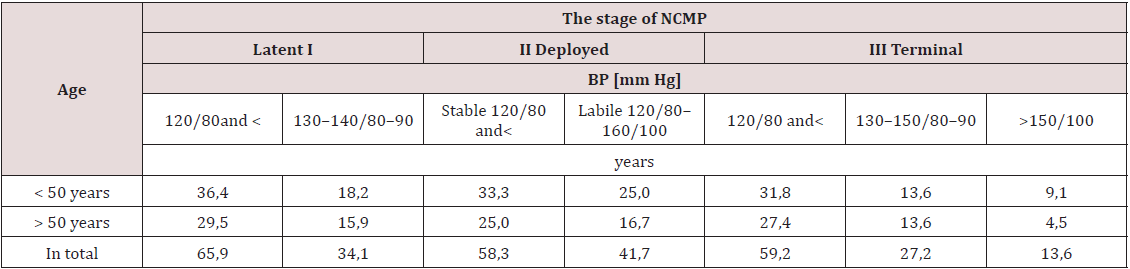
The generalized results on the dynamics of BP in patients with schizophrenia in combination with NCMP are given in the Table 1. It reflects the frequency of occurrence of a level of BP in percentage to the number of deaths in each stage of the disease. Analysis of the table data shows that the frequency of a particular variant of BP in all stages of NCMP doesn’t depend on the age of patients. The difference in rates in patients younger and older than 50 years is random. In the latent stage of NCMP normal BP and hypotension are dominated statistically significantly and substantially (by almost half). Insignificant Arterial Hypertension (AH) is observed only approximately in ⅓ cases. In the developed stage of disease is equally common as a stable normal (and even slightly reduced) BP, and labile with a tendency to moderate AH (the difference in the corresponding indicators is statistically insignificant). Finally, in the terminal stage almost 60% of patients have normal BP and hypotension, slightly more than ¼ - moderate AH, and BP is constantly more than 150/100 mm Hg in 13.6% of patients. There are no significant differences between the frequency of normal BP and of AH one.
Discussion
The acquired data provide the basis for some arguments and generalizations. It is known that one of the problems that often arise in the appointment of most AP is a marked decrease in BP [2]. The greatest practical interest is the orthostatic hypotension. This action of AP is associated with their side effect on the autonomic system regulating BP - inhibition of a significant part of the postsynaptic α1-adrenergic receptors of blood vessels, leading to vasodilatation. At the same time, BP decreases not only at rest, but also remains low under load. However, in the course of antipsychotic therapy in a number of mental patients with the development of NCMP can be observed directly opposite process - expressed in varying degrees of AH. In my opinion, this is due to cardiac remodeling and compensatory hypertrophy of some part of cardiomyocytes [14]. As a result, BP returns to normal values, remaining either stable at this level, or fluctuating sometimes to the values of 160/100 mm Hg. To the final of the diseases in some observations BP figures reaches 130-150/80-90 mm Hg and remaining stable, and sometimes exceeds 150/100 mm Hg. In general, according to own data, in the case of NCMP the frequency of AH is 37.2 %.
A similar combination of idiopathic dilated cardiomyopathy and systemic AH was shown by MS Kushakovskij [15], and earlier YuV Tirkel’taub [16] observed labile BP in patients with schizophrenia, receiving APT. It is also impossible to exclude the effect on the increase in BP with long-term use of AP, that is, in the terminal stage of the NCMP, the side effects of these drugs on the neuroendocrine and metabolic functions of the body [17]. These are the elements of the metabolic syndrome, one of which is AH [18-20]. Thus, according to own data, there is a strong correlation of the frequency of elevated BP with the degree of fatness of dead patients (ρ=0.84). At the same time, 70.6% of BP changes are associated with an increase in body weight, which is one of the cardinal signs of the metabolic syndrome [18-20].
Conclusion
Thus, the study of the dynamics of BP in case of development in the patients with schizophrenia NCMP allows us to draw the following conclusions:
a) The frequency of this or that option of BP in all stages of NCH doesn’t depend on the age of patients.
b) In the latent stage is essentially dominated by hypo - and normotony;
c) In the developed stage of NMMC stable normal and labile BP with a tendency to moderate AH are equally common.
d) In the terminal stage, slightly more than ¼ of patients have moderate AH, and 13.6% of patients have BP consistently exceeding 150/100 mm Hg.
e) In general, according to own data, in the case of NCMP the frequency of AH is 37.2 %.
f) Fluctuations in the frequency of this or that level of BP, revealed in the development of NCMP, associated with various side effects of AP used in the treatment of schizophrenia.
References
- Volkov VP (2018) Cardiotoxicity of neuroleptics: clinical aspects. Beau Bassin: LAP Lambert Academic Publ.
- Volkov VP (2010) Cardiotoxicity of phenothiazine neuroleptics (review of literature). Psichiat psychopharmacother 12(2): 41-45.
- Volkov VP (2013) Clinical characteristic of an antipsychotic cardiomyopathy. In: VP Volkov (eds.); Actual problems of therapeutic clinic: collective scientific monograph. Novosibirsk: Sib AС: 94-116.
- Volkov VP (2017) Comparative pathology of cardiomyopathy. Bean Bassin: LAP Lambert Academic Publ.
- Volkov VP (2012) Neuroleptic cardoimyopathy. In: Farmakoterapiya: Novye perspektivy i problemy: kollektivnaya nauchnaya monografiya / pod red. VP Volkova i RI Zaharova. Novosibirsk: SibAK Publ 3: 65-84.
- Volkov VP (2017) To problem of a neuroleptic cardiomyopathy. GJARM 4(5): 555649.
- Buckley NA, Sanders P (2000) Cardiovascular adverse effects of antipsychotic drugs. Drug Saf 23(3): 215-228.
- Drobizhev MYU (2004) Cardiological problems of tolerability and safety of neuroleptics. Psihiat psihofarmakoter 6(2): 13-17.
- Mackin P (2008) Cardiac side effects of psychiatric drugs. Hum Psychopharmacol 23(1): 3-14.
- Volkov VP (2018) Morphometric approach to the study of morphogenesis of a neuroleptic cardiomyopathy. GJARM 5(5): 555658.
- Tereshchenko SN, Jaiani NA (2001) Dilated cardiomyopathy today. Zhurn serdechnaya nedostatochnost 3(2): 58-60.
- Volkov VP (2011) To a question of a secondary phenothiazine cardiomyopathy. Klin med 5: 30-33.
- Volkov VP (2013) Neuroleptic cardiomyopathy: diagnostic approaches and criteria of diagnosis. Vrach 9: 69-71.
- Volkov VP (2012) Morphometric aspects of morphogenesis of neuroleptic cardiomyopathy. Ros kardiol zhurn 95(3): 68-73.
- Kushakovskij MS (1997) Chronic congestive heart failure. Idiopathic cardiomyopathies. SPb: Foliant Publ.
- Tirkel’taub YuA (1962) Changes in higher nervous activity, cardiovascular system and its reactivity in patients with paranoid schizophrenia during treatment with neuroleptics. In: Problemy shizofrenii / pod red. LL Rohlina. Moscow, pp. 332-341.
- Cygankov BD, Agasaryan EhT (2010) Analysis of efficacy and safety of modern and classical antipsychotic drugs. Zhurn nevrol psihiatr 106(9): 64-70.
- Volkov VP (2014) On the role of metabolic syndrome in the pathogenesis of neuroleptic cardiomyopathy. Vrach 4: 76-77.
- Mosolov SN, Kabanov SO (2003) Metabolic disorders in antipsychotic therapy. Soc klin psihiatriya 13(2): 162-71.
- ATP-III (2001) Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 285(19): 2486-2497.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...