Lupine Publishers Group
Lupine Publishers
Menu
Review Article(ISSN: 2770-5447)
Acute Myocardial Infarction” (IMA)” Volume 3 - Issue 2
Lázara Eloisa Rodríguez García* and Juan Guiteras Gener
- Faculty of Medical Sciences, Universidad de Ciencias Médicas, Matanzas, Cuba
Received: August 17, 2020; Published: August 31, 2020
Corresponding author: Lázara Eloisa Rodríguez García, Faculty of Medical Sciences, Universidad de Ciencias Médicas, Matanzas, Cuba
DOI: 10.32474/ACR.2020.03.000156
Introduction
Myocardial infarction is the most common presentation of ischemic heart disease. WHO estimated that in 2002 12.6% of deaths worldwide were due to ischemic heart disease, which is the leading cause of death in developed countries and the third leading cause of death in developing countries, post-AIDS and low respiratory infections. In developed countries such as the United States, deaths from heart disease are more numerous than cancer mortality. Coronary pathies cause one in five deaths in the United States and where more than one million people suffer a coronary attack each year, 40% of which will die as a result of a heart attack. So an American will die every minute of a coronary pathological event. They also occur in the patient who does not care for a gastritis that has been charged for a certain time and in the patient who is under constant stress. In our daily action for different causes, we are subjected to permanent stress, adding to them, the risk factors of this entity. That is why we were motivated by the revision of the issue in question.
Objectives
1) Mention the etiology of Acute Myocardial Infarction.
2) Describe the clinical picture of Acute Myocardial
Infarction.
3) Name the clinical research to be carried out to verify your
diagnosis.
4) Cite the treatment to be used in Acute Myocardial
Infarction.
Development
Acute myocardial infarction
The term acute myocardial infarction (acute means sudden, my
muscle and cardio heart), often abbreviated as IAM or MAOI and known in colloquial language as heart attack, heart attack or heart
attack, reflects the death of heart cells caused by ischemia resulting
from the imbalance between demand and the supply of blood
supply through coronary circulation.
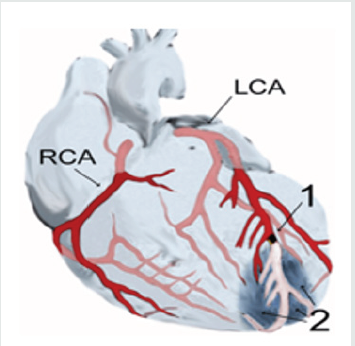
(Diagram of a myocardial infarction (2) at the tip of the anterior
wall of the heart (an apical infarction) following the occlusion (1) of
one of the branches of the left coronary artery (ACL), right coronary
artery (RCA).
Development
Etiology
Acute myocardial infarction occurs in patients with ischemic heart disease, either in those who already knew they were suffering from and treated for this disease, or as an initial episode of the pathology. It is often preceded by a history of unstable angina, a name given to episodes of chest pain that become more frequent, more durable, that appear with lesser effort than in previous evolution or that do not give in with the usual medication. The myocardial (the heart muscle) suffers a heart attack when advanced coronary heart disease exists. This usually occurs when an ateroma plaque inside a coronary artery is ulcerated or ruptured, causing an acute blockage of that vessel. The crown of blood vessels that carry oxygen and nutrients to the heart muscle itself (coronary arteries) may develop athema plaques, which involves to a greater or lesser degree the flow of oxygen and nutrients to the heart itself, with effects ranging from an angina (when interruption of blood flow to the heart is temporary), to a myocardial infarction (when permanent and irreversible).
Thrombus and plunger
The presence of arteriosclerosis in a blood vessel causes narrowing in the vessel and more easily developing a thrombus in the vessel: a platelet clot, clotting proteins and cellular waste that ends up plugging the vessel. A plunger is a thrombus that has traveled through blood to a small glass where it is interlocked like a plunger.
Risk Factors
Risk factors for the onset of a myocardial infarction are closely
related to risk factors for arteriosclerosis and include, but are not
limited to: High blood pressure; (High or higher blood pressure
than set parameters). High cholesterol; smoking; is more common
in men than in women. Hypercholesterolemia or, more specifically,
hyperlipoproteinemia, in particular elevated levels of low-density
lipoprotein (LDL) and low levels of high-density lipoprotein (HDL);
homozysteinemia, i.e. an elevation in the blood of homocysteine
concentration, a toxic amino acid that rises with low or insufficient
levels in the intake of vitamin B2, B6, B12 and folic acid; diabetes
mellitus (with or without insulin resistance); obesity, which is
defined through the body mass index (an index greater than 30 kg/
m2), abdominal circumference or waist/hip index; stress.
The main cause is coronary artery disease with insufficient
blood supply, which causes tissue damage to a part of the heart
caused by obstruction in one of the coronary arteries, often by
rupture of a vulnerable ateroma plaque. Ischemia or poor oxygen
supply resulting from such a blockage results in angina, which if
rechanneled early, does not cause death of heart tissue, while if
anoxia (lack of oxygen in a tissue) or hypoxia (decreased oxygen
supply) is maintained, the heart injury occurs and eventually
necrosis, i.e. infarction.
It is the most common, but not the only, cause of sudden cardiac
death, through the arrhythmias. The picture is of cardiac arrest.
However, in most cases there is electrical activity in the heart, the unemployment of which can be reversed with early defibrillation.
Clinical table
About half of heart attack patients have warning symptoms prior to the incident. The onset of symptoms of a myocardial infarction usually occurs gradually over the course of several minutes, and rarely occurs instantly. Any number of symptoms consistent with a sudden interruption of blood flow to the heart are grouped within acute coronary syndrome.
Chest pain
Sudden chest pain is the most common symptom of a heart attack, is usually prolonged and is perceived as intense pressure, which can spread or spread to the arms and shoulders, especially on the left side, back, neck, and even the teeth and jaw. Chest pain due to ischemia or a lack of blood supply to the heart is known as angina or angina, although painless heart attacks, or with atypical pains that do not coincide with what described herein, are not uncommon.
That is why it is said that the diagnosis is always clinical, electrocardiographic and laboratory, since only these three elements together will allow an accurate diagnosis. When typical, pain is described as a huge fist that twists the heart. It corresponds to angina but prolonged over time and does not respond to the administration of the medicines with which it was previously relieved (e.g. sublingual nitroglycerin) nor does it give way with rest. Pain is sometimes perceived differently, or does not follow any fixed patterns, especially in the elderly and people with diabetes. In heart attacks that affect the lower or diaphragmatic face of the heart it may also be perceived as prolonged pain in the upper abdomen that the individual could mistakenly attribute to indigestion or heartburn. Levine’s sign has been categorized as a classic and predictive sign of a heart attack, in which the affected person locates chest pain by strongly grasping his chest at the breastbone level.
Breathing difficulty
Dyspnoea or shortness of breath occurs when heart damage reduces heart output from the left ventricle, causing left ventricular insufficiency and, as a result, pulmonary edema. Other signs include diaphoresis or excessive sweating, weakness, dizziness (in 10 percent of cases it is the only symptom), palpitations, nausea of unknown origin, vomiting and fainting. The onset of these latter symptoms is likely to result from a massive release of catecholamines from the sympathetic nervous system, a natural response to pain, and hemodynamic abnormalities resulting from heart dysfunction.
Serious signs
More serious signs include loss of consciousness due to inadequate brain infusion, cardiogenic shock, and even sudden death, usually due to ventricular fibrillation.
In women
Women tend to experience symptoms markedly different from those of men. The most common symptoms in women are dyspnoea, weakness, fatigue and even drowsiness, which manifest up to a month before the clinical onset of ischemic infarction. In women, chest pain may be less predictive of coronary ischemia than in men.
Heart Attacks Without Pain or Without Other Symptoms
About a quarter of myocardial infarctions are silent, meaning they appear without chest pain and without other symptoms. These infarctions are usually discovered some time later during subsequent electrocardiograms or during an autopsy with no history of heart attack-related symptoms. This silent course is most common in the elderly, in patients with diabetes and after a heart transplant, probably because a donated heart is not connected to the nerves of the host patient. In patients with diabetes, differences in the threshold of pain, autonomic neuropathy and other physiological factors are possible explanations of the absence of symptomatology during a heart attack.
Diagnosis (clinical investigations)
Diagnosis of a myocardial infarction should be made by integrating clinical aspects of the individual’s current disease and a physical examination, including an electrocardiogram and laboratory tests indicating the presence or absence of cell damage of muscle fibers. For this reason, the semiology that the clinician must apply in the presence of precordial pain (by its characteristics and duration) should compel him to propose the diagnosis of acute myocardial infarction (AMI) with sufficient haste, since the delay in the approach results in the loss of a valuable time necessary to institute the available re-infusion method with the idea of recovering the greatest extent of myocardium since, as is well known, there is an inverse relationship between the time elapsed to start the procedure and the amount of muscle “saved”.
Diagnostic criteria
World Health Organization (WHO) criteria are those that
are classically used in the diagnosis of a myocardial infarction. A
patient is likely diagnosed with a heart attack if he or she has two
of the following criteria, and the diagnosis will be definitive if he or
she has the three Medical History of Ischemic Chest Pain that lasts
longer than 30 minutes; electrocardiographic changes in a series of strokes, and increase or fall of serum biomarkers, such as creatine
kinase type MB and troponin.
These WHO criteria were redefined in 2000 to give
predominance to cardiac markers. According to the new provisions,
an increase in cardiac troponin, accompanied by typical symptoms,
of pathological Q-waves, elevation or depression of the ST segment
or coronary intervention, is sufficient to diagnose a myocardial
infarction.
The clinical diagnosis of IAM should then be based on the
conjunction of the following three data: characteristic pain,
suggestive electrocardiographic changes and elevation of enzymes,
and it should be borne in mind that the latter may not be presented
in a timely manner, so the first two changes should be taken into
account to initiate infusion as soon as possible.
Physical exam
The overall appearance of patients with myocardial infarction varies according to symptoms. Comfortable patients or agitated patients with an increased respiratory rate may be seen. It is common to see a pale skin color, suggesting vasoconstriction. Some patients may have a mild fever (38–39 C), high blood pressure, or in some cases decreased blood pressure and the pulse may become irregular.
If heart failure occurs, high jugular venous pressure, hepatoyugular reflux, or swelling of the legs due to peripheral oedema may be found on the physical examination. Several abnormalities can be heard during auscultation, such as a third and fourth cardiac noise, pericardial rubbing, paradoxical unfolding of the second noise, and crackling on the lung.
Ecg. If a person has symptoms that are compatible with a heart attack, they will have an ECG (electrocardiogram) immediately, even in the ambulance that moves them. In fact, you will be attached to an ECG monitor for as long as you are in the Hospital, at least if you enter the room dedicated to the seriously ill heart or coronary unit. More than one ECG should be performed within a few hours since, in the first few hours, the result may be normal, even in the presence of a heart attack.
Cardiac markers
Cardiac enzymes are proteins from heart tissue that are released
into the bloodstream as a result of heart damage, as is the case in
a myocardial infarction. Until the 1980s, the enzymes apparatus
aminotransferase and lactate dehydrogenase were routinely used
for the assessment of heart damage. The disproportionate elevation
of the MB subtype of the enzyme creatine kinase (CK) was then
discovered specifically as a result of myocardial damage. Current
regulations tend to favor troponin I and T units, which are specific to the heart muscle; it is even thought to begin to rise before muscle
damage occurs. Elevated troponin in a patient with chest pain
can correctly predict the likelihood of a myocardial infarction in
the near future. A recent cardiac marker is the ISO enzyme BB of
glycogen phosphorylase.
When heart damage occurs, levels of heart markers rise over
time, so it’s customary to take blood samples and analyze levels of
these enzyme markers over a 24-hour period. Because these heart
enzymes don’t always increase immediately after a heart attack,
those patients with chest pain tend to be treated assuming they
have a heart attack until it is possible to evaluate them for a more
accurate diagnosis.
It is very important to determine the extent of myocardial damage and based on this to make a prediction of the level of recovery of cardiac function that could be expected. Today, techniques are used that combine the use of markers such as troponin 1 with the advantages of cardiovascular MAGNETIC resonance imaging. For example, identification or mapping of troponin 1 (T1) by noncontrast magnetic resonance imaging allows for early identification of the severity of tissue damage in acute myocardial infarction. That is, if significant increases in T1 values are found through the use of magnetic resonance imaging, the likelihood of tissue recovery at six months of evolution decreases.
Angiography
In the most complicated cases or in situations where an
intervention to restore blood flow is warranted, an angiogram of the
coronaries may be performed. A catheter is inserted into an artery,
usually the femoral artery, and pushed to the arteries that supply
the heart. A radio-opaque contrast is then given and a sequence of
x-rays (fluoroscopy) is taken. Clogged or narrowed arteries can be
identified with this procedure but should only be performed by a
qualified specialist.
Isotopic studies or cardiac catheterization (coronary spelling).
As a diagnostic element, they arise when the acute phase has
already passed. However, consideration may be to perform
a kinegiocoronariography by cardiac catheterization, for the
purposes of determining the clogged vessel(s) and to propose a
disobstruction in acute, percutaneous angioplasty with or without
stenting or, more rarely by endarterectomy.
Differential Diagnosis
Differential diagnosis includes other sudden causes of chest pain, such as pulmonary embolism thrombus, aortic dissection, pericardial effusion that causes cardiac tampering, tension pneumothorax, and esophageal tear
Treatment
A heart attack is a medical emergency, so it demands immediate attention. The main goal in the acute phase is to save as much myocardium as possible and prevent additional complications. As time goes on, the risk of damage to the heart muscle increases, so any time that is lost is tissue that has also been lost. When experiencing symptoms of a heart attack, it is preferable to ask for help and seek immediate medical attention. It is not advisable to try to drive yourself to a hospital.
Immediate care
When symptoms of a myocardial infarction appear, most patients wait on average for three hours, instead of proceeding as recommended: make a distress call right away. This prevents sustained damage to the heart, put in the way of expression: “lost time is lost muscle”. Certain positions allow the patient to rest while minimizing breathing difficulty, such as the half-seated position with the knees bent. Air oxygen access is improved if car windows are opened or the shirt collar button is released. If the individual is not allergic, an aspirin tablet may be given, however it has been shown that taking aspirin before calling an emergency medical service may be associated with unexpected delays. Aspirin has an antiplatelet effect and inhibits the formation of clots in the arteries. Soluble presentations are preferred, without enteric or chewable casings, to make their absorption by the body faster. If the patient cannot swallow, a sublingual presentation is recommended. A dose between 162 – 325 mg is generally recommended.
When you arrive at the emergency room, your doctor will likely give several of the following therapies:
a. Oxygen. It is usually given with nasal glasses at 2 or 3 liters. It may be the first step in the hospital or the ambulance itself.
b. Pain relievers (pain medications). If chest pain persists and is unbearable, morphine (1 milliliter-10 mg, or similar medications to relieve it (petidine-dolantine) is given.
c. Antiplatelet agents. They are medicines that prevent platelet aggregation in thrombus formation. The most used are aspirin in doses of 100-300 mg daily, and Clopidogrel.
d. Thrombolytics. These are medicines to dissolve the clot that prevents blood from flowing. Substances such as streptokinase or a “tissue plasminogen activator” are placed either in the vein or directly into the clot by means of a catheter (a long, flexible tube). This medication should be applied in the first six hours of initiating the pain, hence the importance of rapid care. Thrombolytics can only be administered in a specialized facility, usually an Intensive Care Unit, although extra hospital fibrinolysis has already begun by mobile emergency teams with Fibrinolytic TNKase® (tenecteplase) in order to initiate specific treatment as quickly as possible.
e. Nitrates. Nitroglycerin derivatives work by decreasing the heart’s work and therefore its oxygen needs. In angina they are taken in pills under the tongue or also in spray. They can also be taken in long-acting pills or put on slow-release patches on the skin. In the acute phase of a heart attack, they are often used venously (Solinithrin in intravenous infusion).
f. Beta blockers. They work by blocking many adrenaline effects on the body, in particular the stimulating effect on the heart. The result is that the heart beats slower and less strong, and therefore needs less oxygen. They also lower blood pressure.
g. Digital. Digital-derived drugs, such as digoxin, work by stimulating the heart to pump more blood. This is particularly important if the heart attack results in heart failure in the context of atrial fibrillation (quite common arrhythmia in the elderly) with rapid ventricular response.
h. Calcium antagonists or calcium channel blockers prevent calcium from entering myocardial cells. This decreases the tendency of the coronary arteries to narrow and further decreases the work of the heart and therefore its oxygen needs. They also lower blood pressure. They are not usually used in the acute phase of a heart attack, although they are used immediately afterwards.
Conclusion
After having carried out this thorough review we can conclude by expressing that as a highly deadly entity, in addition to the harmful damage that can be caused to humans, we must avoid the possible risk factors that may trigger such an event. Provide health promotion and prevention activities in the community in a clear and appropriate language that allows them to become aware of the danger they are subjected to by practicing inappropriate lifestyles and modes. As well as educating them in such a way that they can identify any symptoms or signs that make them suspect that they may be affected and therefore immediately go to their nearest doctor without self-medicating.
References
- ABDI, Abdikarim, Basgut, Bilgen (2016) An Evidence-Based Review of Pain Management in Acute Myocardial Infarction. Journal of Cardiology & Clinical Research 4(4): 1067.
- Thygesen, Kristian Alpert, Joseph S White, Harvey D Jaffe, Allan S Apple, Fred S Galvani, et al. (2007) Universal definition of myocardial infarction: Kristian Thygesen, Joseph S. Alpert and Harvey D. White on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction Eur Heard J 28 (20): 2525-2538.
- Erica Dall’Armellina, Stefan K Piechnik, Vanessa M Ferreira, Quant Le Si, Matthew D Robson, et al. (2012) Cardiovascular magnetic resonance by non-contrast T1 mapping allows assessment of severity of injury in acute myocardial infarction 14(1): 15.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...