Lupine Publishers Group
Lupine Publishers
Menu
Research Article(ISSN: 2770-5447) 
A Study of Coronary Collateral Circulation in Coronary Artery Disease Volume 3 - Issue 4
Sanjeev Asotra1, Kavita Negi2, Rajesh Sharma1, P.C Negi1 and K S Sood3
- 1Department of cardiology, I.G.M.C Shimla, H.P India
- 2Department of Anatomy, I.G.M.C Shimla, H.P India
- 33Department of Anatomy, I.G.M.C Shimla, H.P India
Received:April 23, 2021; Published: May 3, 2021
Corresponding author: Dr Sanjeev Asotra, Department of Cardiology, I.G.M.C Shimla. H.P India
DOI: 10.32474/ACR.2021.03.000166
Abstract
Coronary artery disease is an important global cause of morbidity and mortality and high prevalence is found in the Indian population. Collaterals developed in coronary arteries help in the protection of the myocardium from infarction, preservation of ventricular functions, and thus reducing cardiovascular events. The objective of this study is to assess the prevalence, clinical predictors of coronary collaterals, relationship with severity of coronary artery disease, regional wall motion abnormality, and left ventricular global ejection fraction.
Methods: 302 consecutive coronary angiograms of patients of clinical diagnosis of coronary artery disease were analyzed. Focused clinical history, demographic profile, and risk factors were analyzed. Medical history focused on chronic stable angina, past myocardial infarction unstable angina and acute myocardial infarction was taken. Collateral vessels were analyzed according to Rentrop classification.
Results: Prevalence of coronary collaterals was seen in 74% of patients with luminal diameter stenosis of >50%. Grade 1 collaterals were observed in 26.5%, Grade 2 in 27.8%, and Grade 3 in 19.8%. 51.7 % of patients had intracoronary, 23.3 % had intracoronary and 25% of patients had both inter and intracoronary collaterals.
Conclusions: The prevalence of coronary collaterals is high in obstructive coronary artery disease. There was no association of collaterals with age, sex, chronic stable angina, unstable angina, and Myocardial infarction. The severity of coronary artery disease had an independent significant association with the presence of collaterals. There was a significant correlation of grade of collaterals with regional wall motion abnormality and with left ventricular global ejection fraction.
Keywords: Coronary collaterals; Coronary artery disease; Coronary angiography; LAD; LCxA; RCA; BMI; EF; RWMA
Introduction
Nature is full of paradoxes and one of the most intriguing is the blood supply to the heart. Although the coronary arteries are treated as end arteries even in a normal human heart, the network of tiny anastomotic branches interconnect the major coronary arteries and are the precursor for the development of collateral circulation [1]. The coronary collateral pathways are seen in significant obstructive coronary artery disease but it is still debatable whether blood flow through them is sufficient to meet the myocardial flow [2]. Atherosclerotic coronary artery disease is now the leading cause of morbidity and mortality worldwide [3]. In Indian it has reached an epidemic proportion, epidemiological studies have predicted that there are more than 30 million cases of CAD in India . The increasing burden in India is due to rapid urbanization and an alarming rise in the prevalence of coronary risk factors like Diabetes, hypertension, smoking, dyslipidemia, central obesity, and physical inactivity [4]. The obstructive coronary artery disease causing recurrent ischemia may be the trigger for the development of collaterals [5]. Complete occlusion of the vessel may lead to a reduction in post stenotic pressure and leading to the redistribution of flow, causing increased shear forces in preexisting arterioles[6-8]. The subsequent angiogenesis and arteriogenesis in the form of growth, expansion, and remodeling of these arterioles to mature[9,10]. Various studies have been done to find the association of atherosclerotic risk factors with collaterals with conflicting evidence [11-15]. In the present study, we aimed to study the relation of the clinical determinants, atherosclerotic risk factors, and relationship of collaterals with regional wall abnormalities and global left ventricular ejection fraction.
Material and Methods
302 consecutive patients who underwent coronary angiography for suspected coronary artery disease were enrolled. Standard selective coronary angiography with at least four views of the left coronary system and two views of the right coronary artery was performed using the Judkins technique. These coronary angiograms were examined by two experienced interventional cardiologists. The following clinical and demographic parameters were recorded; age, sex, hypertension (known hypertension treated with antihypertensive drugs, two or more BP recordings greater than 140/90mmHg.), diabetes (known case being treated with diet, antidiabetic drugs, insulin, or both, HbA1c value more than 6.5%, Fasting blood sugar more than 126mg/dl or random sugar more than 200 mg/dl with symptoms of hyperglycemia), current smoker or tobacco user, family history of CAD. Focused medical history of chronic stable angina, previous myocardial infarction, unstable angina, or acute myocardial infarction was taken. Anthropometric measurement of Waist circumference and Body mass index was calculated. Collateral grading was assessed using Cohen –Rentrop method. Collateral grades were defined as Grade 0: no filling of any collateral vessel, Grade 1: Filling of side branches of the artery to be perfused by collateral vessel, Grade 2; Partial filling of the epicardial artery by collateral vessel, and Grade 3 as complete filling of the epicardial artery by collateral vessel. The severity of diameter stenosis was calculated by QCA. The severity of the coronary artery was assessed by giving a score according to the site of involvement of the coronary artery. Regional wall motion abnormality was assessed by analyzing the contractility of five segments of the left ventricle i.e. anterobasal, anterolateral wall, mid inferior, the basal inferior wall in an LV angiographic study done in RAO 30 degree projection. Left ventricular global ejection fraction was estimated by measuring end-diastolic volume, end-systolic volumes 0-3 grading scale was used to assess the regional wall motion, Grade 0 normal, Grade 1 hypokinesia, Grade 2 akinesia, and Grade 3 as dyskinesia. The summation of all scores given to each segment was taken as regional wall motion abnormality scores.
Statistical Analysis
Data were analyzed using SPSS window version 16.0. Continuous variables were expressed as mean ± standard deviation and categorical variables as percentages. The significance of the difference in the mean values of a continuous variable in coronary artery disease patients with or without collaterals was tested by Student’s T-test and categorical variables were tested by C=chi square test. We conducted a Univariate and Multivariate regression analysis of angiographic variables i.e. severity of the disease, regional motion abnormality score, and left ventricular global ejection fraction with grades of coronary collaterals and calculated regression and /or correlation coefficient. P-value of <0.05 was taken as statistically significant.
Results
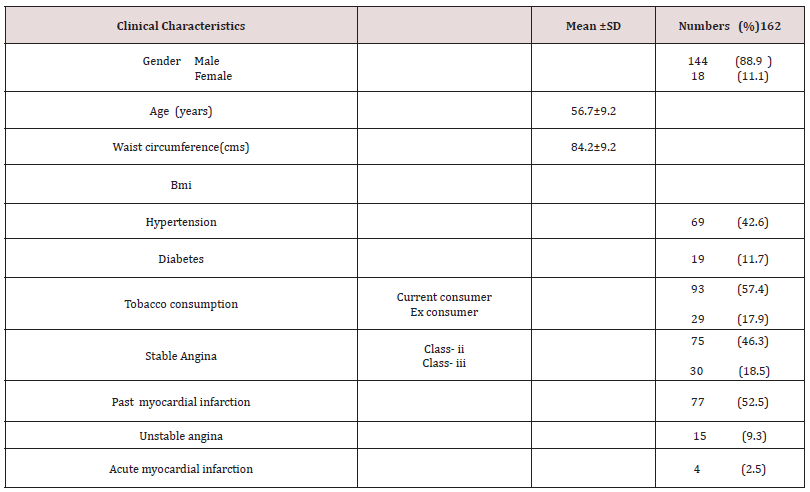
Out of 302 patients, 81% had right dominant circulation, 15% had left dominance and 4% had co-dominant circulation. Ninety-six (32%) patients out of 302 did not show any evidence of atherosclerotic vascular disease. 44 (14.5%) patients had CAD with coronary stenosis <50% and 162 (53.5%) had stenosis >50%. We analyzed the data of 162 patients who had coronary stenosis of >50%. Mean age of patients was 56.7 ± 9.2 years. There was a predominance of males 88.9% in the study population.42.6% of patients were having hypertension,11.7% were diabetics and 57.4% patients were current smokers or were consuming tobacco. The mean waist circumference was 84.2 ± 9.2 and Body mass index was 22.4 ± 3.7. 46.3% patients had chronic stable angina and 52.5 % of patients had a history of myocardial infarction in the past. Table 1 shows the baseline characteristics of the162 patients with coronary stenosis >50%.120 patients out of 162 (74%) had evidence of coronary collaterals. 62 patients (51.7%) patients had intracoronary collaterals ,28 (23.3%) had intracoronary and remaining 30 (25%) had both inter and intracoronary collaterals. We compared the qualitative and quantitative clinical characteristics and risk factors of 162 patients with coronary stenosis >50% with and without coronary collaterals mentioned in Table 2 and Table 3 There was a significant difference in age, sex, BMI, Waist circumference, hypertension, DM, smoking and/ or tobacco consumption, history of chronic stable angina and myocardial infarction. There was a significant inverse relationship of regional wall motion abnormality with the presence of collaterals (p- value>-0.05).
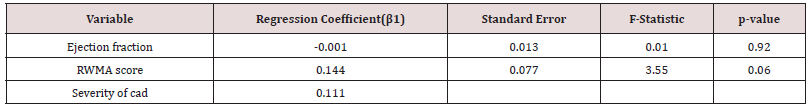
On univariate regression analysis of quantitative clinical variables. age, BMI, waist circumference, stable angina class II & III did not have any significant association with the grade of coronary collaterals (p-<001). Ejection fraction, regional wall motion abnormality score, and severity of disease were significantly associated with the grade of collaterals (p-value,0.001) Table 4. Multivariate regression analysis was done to assess the independent predictive value of clinical variables that were found to be significant on univariate regression analysis. Only severity of disease score was significantly associated with the grade of coronary collateral circulation Table 5.
Table 2: Comparison of qualitative clinical characteristics of patients of coronary artery disease with and without coronary collaterals.
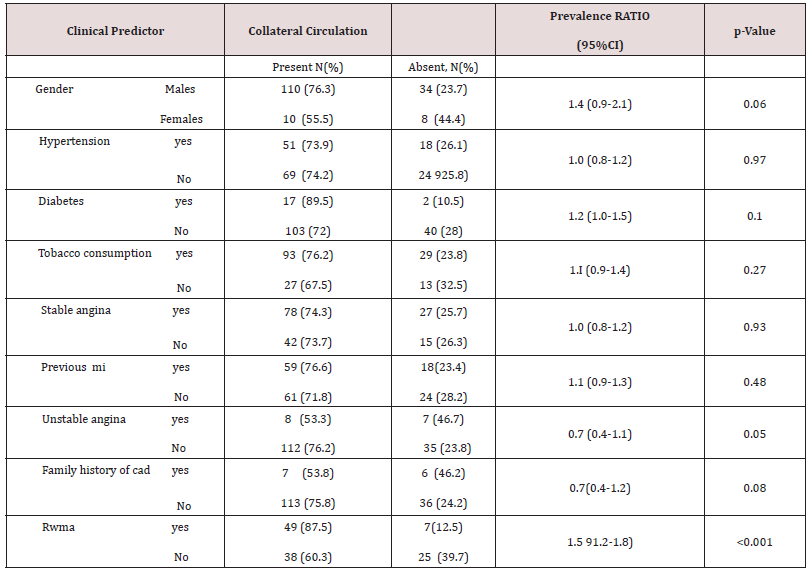
Abbreviations; RWMA regional wall motion abnormality
Table 3: Comparison of qualitative clinical characteristics of patients of coronary artery disease with and without coronary collaterals.
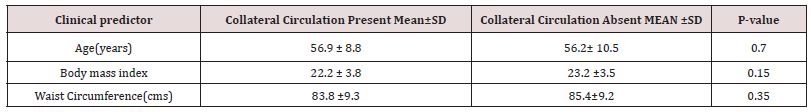
Table 4: Univariate linear regression analysis of grades of collaterals on quantitative clinical variables.
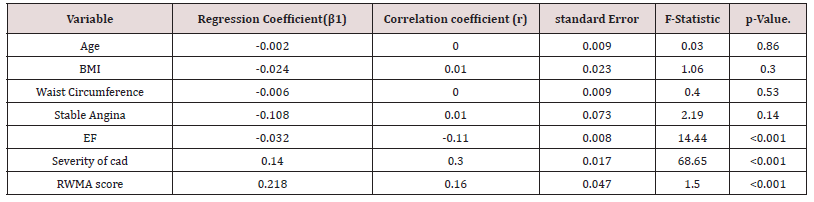
Table 5: Multivariate Linear regression analysis of grades of collateral circulation on clinical variables with p-value <0.001 on Univariate linear regression analysis.
Discussion
302 consecutive patients were prospectively studied and an attempt was made to assess the association of presence or absence of coronary collateral circulation with cardiovascular risk factors, the severity of coronary artery disease, left ventricular global ejection fraction, and regional wall motion abnormality.162 coronary angiographic studies of patients with luminal diameter stenosis >50% were analyzed for coronary collateral circulation. 74% of these patients showed evidence of collaterals. Gensini and Bruto described collaterals in 37 of 100 coronary angiograms with coronary obstruction >50% [16, 17]. Our study showed no relation of clinical variables like age, sex, hypertension, diabetes, tobacco consumption, obesity, history of chronic stable angina, unstable angina, and myocardial infarction.
Definitive data on the effects of aging on collaterals in humans are very limited. Advancing age is considered an important factor for impaired collateral formation. Nakae et al have reported that the extent of collateral growth is influenced by the age of patients and it was significantly lower in the elderly age group [18]. Animal data shows collateral rarefaction with increasing age [19]. Aging induced eNOS dysfunction, increasing oxidative stress, impaired mobilization and progenitor cell functions leading to impaired ischemia-induced angiogenesis and reduced myocardial capillary density [14], [20-23]. Our study found no relation between aging with collaterals.
Systemic hypertension is a major cardiovascular risk factor and its association with the development of coronary collaterals is controversial [11] [24-26]. An increase in myocardial oxygen demand in chronic hypertension induces angiogenic responses leading to increased recruitment of capillary network [11].Nitric oxide plays an important role in the regulation of blood pressure. Animal studies showing abnormal bio area activity of nitric oxide are associated with impaired angiogenesis. It has been shown that the association of poor angiogenic response to hypertension is mediated by nitric oxide rather than elevated blood pressure [27, 28]. Our study did not find the association of diabetes mellitus with the presence or absence of coronary collaterals. Meliodonis et al had reported more extensive collaterals in patients with diabetes [29]. The majority of studies had shown poor collateral formation with diabetes [30-33].The poor development of collateral may be due to activation of signal transduction pathways resulting in VEGF resistance and downregulation of cellular pathways necessary in arteriogenesis [32] [34,35]. Zibeden et al. and Bhat et al also found no association of collaterals with diabetes [14] [32].
Smoking is a major risk factor for the development of atherosclerotic vascular disease. Animal model studies have demonstrated the inhibitory role of smoking extracts on angiogenesis [36]. Nicotine has pro-angiogenic effects by increasing the NO synthetase and causing proliferation of endothelial cells thus increasing capillary network [37,38]. Koerselman et al. and Bhatt et al showed that smoking was associated with the presence of coronary collaterals [12] [32]. Our study showed no correlation between smoking with coronary collaterals.
Obesity predisposes to the development of diabetes, hypertension, dyslipidemia, and OSA. All these have a strong association with CAD. Animal models have shown a reduced number of circulating endothelial progenitor cells thus suppressing angiogenesis [39]. Studies have shown an increased risk of impaired collateral formation with increased BMI. Yilmaz et al showed that BMI > 30 was associated with poor coronary collateral in patients with CAD [40]. Bhatt et al also showed increasing BMI was associated with the absence of coronary collaterals [32]. Visceral adipose tissue is metabolically an active organ and an excess level of visceral adipose tissue regardless of BMI is considered an independent risk factor for diabetes and atherosclerosis. Visceral fat has a strong association with coronary heart disease than BMI. Visceral fat index may be a novel predictor for poor coronary collateral circulation [41]. Our study did not found an association of BMI with collaterals. Tatli et al also found no association of obesity with collaterals [42]. The reason for the lack of association could be due to the lack of obesity in our study population. The mean BMI was just 22.4 ± 3.7 in our subjects.
Hansen et al and Arzu et al reported patients with collaterals were associated with a higher incidence of chronic stable angina and history of previous myocardial infarction [43-45]. Piek et al showed the duration of angina, coronary artery severity, and proximal lesion location were positively associated with coronary collaterals [46]. Fujista et al showed the presence of pre infarction angina occurring more than one week before acute myocardial infarction was strongly associated with the development of coronary collaterals [44]. The surviving ischemic myocardium may stimulate the formation of collaterals.
Univariate linear regression analysis of grades of coronary collaterals with age, BMI, waist circumference and functional class of angina did not reveal any significant correlation. However, there was a significant positive correlation of collaterals with the severity of CAD and regional motion abnormality. Multivariate linear regression found no association of grades of collaterals with regional wall motion score There is no doubt that the most potent stimulus for collateral growth is triggered by an obstructive lesion in the coronary artery. Zoll et al demonstrated the incremental stenosis on collateral growth in the autopsy series.[15] Collaterals were seen in 63% of patients in severe obstruction and 95 % of patients with complete coronary stenosis in this study. Studies by Piek et al and Pohl et al showed the relationship of collateral growth with coronary stenosis[46,47] . The observed a higher prevalence of collateral circulation with a more high regional wall motion score in our study may indicate the presence of more severe coronary artery disease and Regional wall motion abnormality could be the result of stunned myocardium or irreversible myocardial damage. Further assessment of myocardial viability by other tests might have given a clear answer. Tandonen et al also showed grade 3 collaterals had the highest wall motion score, the grade of coronary collaterals had an inverse relationship with left ventricular functions. and collaterals had no preventive effect on ventricular functions The authors concluded that this may be related to severe CAD in these patients [48].
References
- Popma JJ, Bittl J (2001) Coronary Angiography and intravascular Ultrasonography.In: Braunwald E, Zipes DP, Libby P. eds, Heart Disease: A textbook of cardiovascular medicine., Philadelphia: W.B.Saunders Company 387-418.
- Levin DC (1974) Pathways and functional significance of Coronary Collateral Circulation. Circulation. 50(4): 831-837.
- Roth GA, Abate D, Abate KH, et al. (2018) Global, regional, and national age-sex specific mortality for 82 causes of death in 195 countries and territories,1980-2017:a systematic analysis for the global burden of disease study 2017. Lancet 392(10159): 1736-1788.
- India State-Level Disease Burden Initiative CVD Collaborators (2018) The changing patterns of cardiovascular diseases and their risk factors in the states of India: the global burden of disease study1990-2016-Lancet Glob Health 6: e1339-e1351.
- Oliver MF (1986) Prevention of coronary heart disease-propaganda, promises, problems, and prospects. Circulation 73(1): 1-9.
- Sasayama S, Fujita M (1992) Recents insights into coronary collateral circulation. Circulation 85(3): 1197-1204.
- Van Royenn, Piek Jj, Buschmann I, , M Voskuil, W Schaper Et Al. (2001) Stimulation Of Arteriogenesis: A New Concept For The Treatment Of Arterial Occlusive Disease. Cardiovasc Res 49(3): 507-521.
- Heil M, Schaper W (2007) (2000) Insights into pathways of arteriogenesis Curr Pharm Biotechnol 8(1): 35-42.
- Carmeliet P (200) Mechanism of angiogenesis and astrogenesis. Nat Med 6(4): 389-395.
- Schaper W, Ito WD. Res (1996) Molecular mechanisms of coronary collateral vessel growth. Circ 79(5): 911-919.
- Koerselman J, deJaegre PP, Verhaar MC, van der Graaf Y, Grobee DE. SMART Study Group (2005) High blood pressure inversely related with the presence and extent of coronary collaterals. J Hum Hypertens 19(10): 809-817.
- Koerselman J, deJaegre PP, Verhaar MC, van der Graaf Y, Grobee DE, et al. (2007) Coronary collateral circulation: the effects of smoking and alcohol. Atherosclerosis 191(1): 191-198.
- Chen Yl, Chang C, Sun CK, Chiung-Jen Wu, Tzu-Hsien Tsai, et al. (2012) Impact of obesity on circulating levels of endothelial progenitor cells and angiogenesis in response to ischemic stimulation. J Translational Med 10: 86-88.
- Xing Z, Pei J, Tang L, Xinqun H (2018) Tradional cardiovascular risk factors and coronary collateral circulation. Medicine 97(17): e0417.
- Zoll PM, Wessler S, Schlesinger MJ (1951) Intraarterial coronary anastmosis in human heart ,with particular reference to anemia and relative cardiac anoxia. Circulation 4(6): 797-815.
- Zbinden R, Zibenden S, Billinger M, Windecker S, et al. (2005) Influence of diabetes mellitus on coronary collateral flow;an answer to an old controversy. Heart 91(10): 1289-1293.
- Gensini G, Bruto Da costa BC (1969) The coronary collateral circulation in living man. Am j Cardiol 24(3): 393-400.
- Nakae I, Fujita M, Miwa K, K Hasegawa, Y Kihara, et al. (2000) Age dependent impairment of coronary collateral development in humans. Heart vessels 15(4): 176-180.
- Sullivan JC, Loomis ED, Collins M, Imig JD, Inscho EW, et al. (2004) Age-related alterations in NOS and oxidative stress in mesenteric artery from male and female rats. J Appl Physiol 97(4): 1268-1274.
- Rivard A, Fabre JE, Silver M, Chen D, Mushohara T, et al. (1999) Age-dependent impairment of angiogenesis. Circulation 99(1): 111-120.
- Faber JE, Zhang H, Lassance-Soares RM, Prabhakar P, Najufi AH, et al. (2011) Aging causes collateral rarefaction and increased severity of ischaemic injury in multiple tissues. Arterio Thromb Vasc Biol 31(8): 1748-1756.
- Dai X, Faber JE (2010) ENOS deficiency causes collateral vessel rarefaction and impair activation of cell cycle gene network during arteriogenesis. Circ Res106: 1870-1881.
- Csiszar A, Ungvar Z, Edwards JG, Kaminski P, Wolin MS, et al. (2002) Aging induced phenotypic changes and oxidative stress impair coronary arteriolar function. Circ Res 90(11): 1159-1166.
- Kyriakides ZS, Kremastinos DT, Michelakakis NA, Mastakas EP, Demovelis T, et al. (1991) Coronary collateral circulation in coronary artery disease and systemic hypertension. Am J Cardiol 67(8): 687-690.
- Karpanaou EA, Vyssoulis GP, Skoumas JN, Zervopoulos GA, Moundaki VS, et al. (1988) Significance of arterial hypertension on coronary collateral circulation development and left ventricular function in coronary heart disease. J hypertens Suppl. 6(4): S151-S153.
- Hermann M, Flammer A, Luscher TF (2006) Nitric oxide in hypertension. J clin Hypertens 8(12): 17-29.
- Kiefer FN, Misteli H, Kalak N, Karin Tschudin, Jürgen Fingerle, et al. (2012) Inhibition of NO biosynthesis but not elevated blood pressure, reduces angiogenesis I rat models of secondary hypertension. Blood Press 11(2): 116-124.
- Kiefer FN, Neysari S, Humar R, Li W, Munk VC, et al. (2003) Hypertension and angiogenesis. Curr Pharm Res 9(21): 1733-1744.
- Melidonis A, Tournis S, Kouvaras G, S Hadanis, I Hajissavas, et al. (1999) Comparison of coronary collateral circulation in diabetic and non-diabetic patients suffering from coronary artery disease. Clin Cardiol 22(7): 465-471.
- Abaci A, OguZhan A, Kahraman S, N K Eryol, S Unal, et al. (1999) Effect of diabetes mellitus on the formation of coronary collateral vessels. Circulation 99(17): 2239-2242.
- Yetkin E, Topal E, Erguzel N, Senen K, Heper G, et al. (2015) Diabetes mellitus and female gender are the strongest predictors of poor collateral vessel development in patients with severe coronary artery stenosis Angiogenesis 18(2): 201-207.
- Bhatt H, Kochar S, Htun WW, Julliard K, Fernaine G (2015) Coronary collateral circulation and cardiovascular risk factors: Is there a paradox? Angiology 66(6): 588-594.
- Werner GS, Richartz BM, Heinke S, Ferrari, Figulla HR (2003) Impaired acute collateral recruitment as a possible mechanism for increased cardiac adverse events in patients with diabetes mellitus. Eur Heart J 24(12): 1134-1142.
- Waltenberger J (2001) Impaired collateral vessel development in diabetes: potential cellular mechanisms and therapeutic implications. Cardiovasc Res 49(3): 554-560.
- Tchaikovski V, Olieslagers S, Bohmer FD, Waltenberger J (2000) Diabetes mellitus activates signal transduction pathways resulting in vascular endothelial growth factor resistance of human monocytes. Circulation 120(2): 150-159.
- Michaud SE, Menard C, Guy LG, Gennaro G, Rivard A (2003) Inhibition of hypoxia-induced agenesis by cigarette smoke exposure: impairment of HIF-1alpha/VEGF pathways. FASEBJ 17(9): 1150-1152.
- Avogro A, Fadini GP (2006) The jane face of nicotine angiogenesis. JACC 48(12): 2561-2563.
- Heeschen C, Weis M, Cooke J (2003) Nicotine promotes arteriogenesis. JACC 41(3): 489-496.
- Chen YL, Chang C, Sun CK, Chiung-Jen Wu, Tzu-Hsien Tsai, et al. (2012) Impact of obesity control on circulating levels of endothelial progenitor cells and angiogenesis in response to ischemic stimulation. J Translational Med 10: 86-89.
- Yilmaz MB, Biyikoglu SF, Akin Y, et al. (2003) Obesity is associated with impaired coronary collateral development. Int. J Obesity 27(12): 1541-1545.
- Sahinturk Y, Kucukseymen S, Avci, Aksaru A, Yolcular BO et al. (2020) Visceral fat index: A novel predictor for coronary collateral circulation.Arch Endocrinol Metab 64(2): 150-158.
- Tatli E, Yildaz M, Gul C, Birsin A, Karahasanoglu, et al. (2005) angiology 56(6): 657-661.
- Hansen JF (1989) Coronary collateral circulation: clinical significance and influence on survival in patients with coronary artery occlusion. Am Heart j 117(2): 290-294.
- Fujista M, Sassayamo S, Ohno A, Nakajima H, Asanoi H (1987) Importance of angina for development of coronary collateral. Br Heart J 57(2): 139-143.
- Arzu J, Rahman F, Haque KF, Siddique MA (2011) Study of coronary collaterals in patients with stable angina Univ Heart j 6(2): 61-64.
- Piek JJ, van Liebergen RAM, Koch KT, Peters RJG, David GK (1997) clinical, angiographic, and hemodynamic predictors of recruitable collateral flow assessed during Balloon angioplasty coronary occlusion. J Am Coll Cardiol 29(2): 275-282.
- Pohl, Seiler C, Billinger M, Wustmann K, Mehta H, et al. (2001) Frequency distribution of collateral flow and factors influencing collateral channel development. Functional collateral channel measurement in 450 patients of coronary artery disease. J Am Coll Cardiol 38(7): 1872-1878.
- Tandogan I, Altinok A, Aslan H, Sezgin AT, Barutcu, et al. (2002) Are the effects due to the existence of coronary collateral circulation on left ventricular function in patients with coronary artery disease? Anadolu Kardiyol Derg 2(2): 91-95.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...