
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Case ReportOpen Access 
Foreign Body Liver Abscess: Case Report and Literature Review Volume 5 - Issue 3
Caroline Mignha Aben Athar Fernades1, Camila Maria Rosas Lago1, Eron Santos de Almeida1, Ana Patrícia Feio Antunes1, Louise Paiva Ferraz1, Gabriel Silva Novais2, Maria Victória Souza da Silva Conde3 and Simone Regina Souza da Silva Conde1*
- 1João de Barros Barreto University Hospital, Federal University of Pará, Brazil
- 2Physician graduated from the Federal University of Pará, Brazil
- 3Medicine student from University of São Paulo, Brazil
Received: April 18, 2023 Published: April 27, 2023
Corresponding author: Simone Regina Souza da Silva Conde, João de Barros Barreto University Hospital, Federal University of Pará, Belém 66073-000, PA, Brazil
DOI: 10.32474/JCCM.2023.05.000211
Abstract
Liver abscess is an intra-abdominal infection, generally bacterial, which presents a decrease in mortality rates in the last years due to the systematic use of broad-spectrum antibiotics and advances in diagnostic medicine. However, there are rare cases, such as in biliary abscesses caused by foreign bodies, in which the suspicion comes after refractivity to conservative treatment, and the definitive diagnosis is obtained only during surgery. This report describes a clinical case based on a middle-aged male patient with pyogenic liver abscess, who had, during the surgical procedure, a finding of a foreign body firmly adhered to the liver. Consistent with the literature, the beginning of clinical improvement occurred from the identification of the foreign body and its removal during exploratory laparotomy.
Keywords: Pyogenic Liver Abscess; Foreign Body; Sepsis with Abdominal Focus
Introduction
Liver abscess is an intra-abdominal infection, generally bacterial, sometimes, parasitic, or, very rarely, fungal, with a greater incidence between the fifth and sixth decades of life, presenting decreasing mortality in last year’s due to the systematic use of antibiotics of broad spectrum and advances in diagnostic medicine. The main symptoms are fever, pain on palpation of the right hypochondrium, hepatomegaly and, rarely, jaundice [1,2]. The diagnosis can be defined by ultrasonography or computerized tomography of the abdomen, for the morphological characterization of the lesion, which may be single or multiple, depending on the causal agent. Laboratory tests may evidence leukocytosis with neutrophilia, discrete to moderate alterations in aminotransferases, gammaglutamyl transferase, alkaline phosphatase and acute inflammatory evidences [2]. Abscesses in general can be included in 3 subgroups, type i abscess (small <3cm), type ii abscess (large >3cm, unilocular) and type iii abscess (large >3 cm, multilocular complex). According to the classification, antibiotic therapy exclusive or associated with cutaneous or surgical drainage is opted [3]. Most liver abscesses can be classified as pyogenic or amoebial. Among amoebal abscesses, the main etiological agent is entamoeba histolytic, while pyogenic abscesses are more commonly polymicrobial, with a higher incidence of E. coli, klebsiella, streptococcus, staphylococcus and anaerobic bacteria [4]. Biliary abscesses caused by foreign bodies configure rare cases, often suspected only in view of refractory to conservative treatment of pyogenic liver abscess [1,2,5,6]. Since patients do not commonly remember the ingestion of the foreign body, these elements are commonly found only during surgery. This report describes a clinical case based on a middle-aged male patient with pyogenic liver abscess, refractory to antibiotic therapy, along with acute inflammatory abdomen, who had as a finding, during the surgical procedure; a foreign body firmly adhered to the liver.
Case Report
53-year-old male patient admitted with a history of nausea, twisting abdominal pain in the upper quadrants, high daily fever, jaundice and coluria. There was a history of drinking with large quantities of fermented beverages, without other combi ties. On physical examination, he presented in regular general condition, tachycardia, hypo colored, jaundred, hypo hydrated, with flaccid abdomen, with pain on deep palpation of upper quadrants, without peritoneal defense, masses or visceromegalies. In laboratory examinations, there was anemia, signal elevation of transaminases, hyperbilirubinemia and no leukocytosis, as seen in Table 1.
In view of the clinical and laboratory framework, diagnostic hypotheses corresponding to abdominal pain syndrome, such as cholangitis, cholecystitis and liver abscess have been advised. At first, the antimicrobial scheme was maintained with ceftriaxone 2g/day and metronidazole 500 mg 8/8h, which was started three days before the transfer to this institution. On the day following the admission, he evolved with tachypnea, hypotension, drowness and peritoneal defense on the physical examination of the abdomen, being opened a protocol for sepsis, staging antibiotics for piperacillin with tazobactam and metronidazole. A place in an intensive care unit was requested and assessment by the general surgical team was required. On the same day, the patient underwent ultrasonography of the whole abdomen, evidenciating a liver of preserved dimensions, with homogeneous echotexture, without signs of dilations of intra or extrahepatic biliary tract, with a nodule in the left hepatic lobe with hypoechoic septations with gross septations measuring 10 x 9.0 x 9.0 cm, suggestive of a liver abscess, as shown in Figure 1.
Figure 1: Ultrasonography of the whole abdomen evidence of a hypoechoic nodule in the left hepatic lobe with coarse septations measuring 10 x 9.0 x 9.0 cm, suggestive of a liver abscess.
Quickly, exploratory laparotomy was prompt, having the intraoperative findings:
a. Large amount of free abdominal fluid, non-purulent.
b. Integrated purulent liver collections in segments ivb and
iii. c. Gastric background firmly adhered to the liver near the abscess region and presence of a foreign body (fish her berry) approximately 5cm in length, as observed in Figure 2.
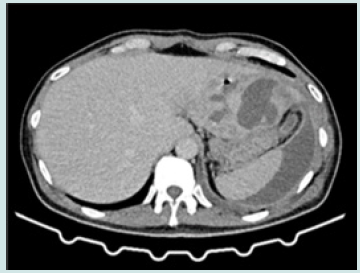
Abdominal cavity wash and methylene blue tests were done via nasogastric tube, without evidence of extravasation through the gastric wall. Two weeks later, tomography of the total abdomen with contrast showed evidence of residual collection in the left hepatic lobe, evidenced in Figure 3. Due to the good postoperative clinical evolution, the patient was discharged from hospital with prescription of ciprofloxacin and metronidazole oral and indication outpatient via at the hospital.
Figure 3: Upper abdomen CT scan with contrast portal phase, ten days after laparotomy and removal of the foreign body.
Discussion
Most foreign bodies in the gastrointestinal tract are impacted in the cricopharyngeal region and more than 90% pass through the digestive tract without causing any type of injury [1,7]. The presence of a foreign body in the liver as a cause of pyogenic liver abscess is one of the less considered etiologies in studies regarding the disease [1,5,6]. The consequences of a hepatic foreign body vary from small injuries to acute abdomen. The combination of findings from clinical history, physical examination and image are of fundamental importance in the formation of the hypothesis of pyogenic liver abscess by foreign body. Ultrasonography of the abdomen helps to identify collections in the liver parenchyma, defining focus, septation and measurements [1]. However, computerized tomography of the abdomen proves to be more sensitive in the sense of greater precision in delimiting the extent and locating the focus, as well as the identification of the foreign body; however, many foreign bodies can be interpreted as surgical clips or even imaging artifacts. In this context, the exploration of the cavity via laparoscopic or laparotomy allows the direct detection of the intruding corpus [6]. As to the nature of the hepatic foreign body, the literature records a greater prevalence of fish backbone (44%), chicken bones (8%) and toothpicks (7%) [6,7]. In these studies, the main comorbidities of patients with the condition were diabetes, cancer, cirrhosis and diverse forms of immunosuppression [6], which, at principle, would not have correlation with this etiology. In the reviewed case series, in the absence of identification of the hepatic foreign body, all attempts at conservative treatment with antibiotic therapy were failed. On the other hand, once the elements were found and the surgical treatment has been proceeded, the patients evolved with improvement in the clinical condition. The patient of this report was admitted in failure of conservative therapy for abdominal infection, having liver abscess as one of the diagnostic hypotheses. He progressed rapidly with systemic complications and was submitted to total abdomen ultrasonography examination, more readily available compared to computerized tomography at the time of evolution to instability. Consistent with the literature, the beginning of clinical improvement occurred from the identification of the foreign body and its removal during exploratory laparotomy. After the surgery, the antibiotic therapy, initiated at the opening of the sepsis protocol, was maintained. The patient evolved satisfactorily, with hospital discharge and outpatient follow-up.
References
- Melo HMI (2019) Liver Abscess Due to Fishbone: Case Report. Revista Eletrônica Acervo Saúde 19(1): E265-E265.
- Bittencourt PL, Zollinger CC, Lopes EPDA (2017) Manual De Cuidados Intensivos Em Hepatologia. Editora Malole, Sociedade Brasileira De Hepatologia, 2°Edição, Barueri-Sp, 2017. Disponivel Em 15(1): 09-10.
- Hope WW, Vrochides DV, Newcomb WL, Mayo Smith WW, Iannitti DA (2008) Optimal Treatment of Hepatic Abscess. Am Surg 74(2): 178-182.
- Akhondi H, Sabih De (2022) Liver Abscess. [Updated 2022 Jul 4]. In: Stat pearls [Internet]. Treasure Island (Fl): Statpearls Publishing, Southern US.
- Waisberg J, Aráuz SNZE, Altieri LG (2002) Pyogenic Liver Abscess Due to Foreign Body. Magazine of the Brazilian College of Surgeons 29(1): 240-241.
- Laggieri N, Marques Vidal P, Cerwenka H, Denys A, Dorta G, et al. (2010) Migrated foreign body liver abscess: illustrative case report, systematic review, and proposed diagnostic algorithm. Medicine 89(2): 85-95.
- Glick WA, Simo KA, Swan RZ, Sindram D, Iannitti DA, et al. (2011) Pyogenic hepatic abscess secondary to endolumenal perforation of an ingested foreign body. Journal of Gastrointestinal Surgery 16(4): 885-887.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...






