Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Research Article(ISSN: 2637-6636) 
Qualitative Study of Parental Preferences in Difficult Child Behavior Scenarios Volume 7 - Issue 1
Grisham EA1, Wells MH2*, Kocak M3, De Schepper E4, Woods MA5 and Fernandez J6
1Associate Pediatric Dentist in Private Practice, Alabama Pediatric Dental Associates and Orthodontics, Huntsville, AL, USA
2Professor and Director of Graduate Pediatric Dentistry Program, Department of Pediatric Dentistry and Community Health, College of Dentistry, University of Tennessee Health Science Center, USA
3Professor and Associate Dean, Department of Preventive Medicine, College of Medicine, University of Tennessee Health Science Center, USA
4Associate Dean for Academic Affairs, College of Dentistry, University of Tennessee Health Science Center, USA
5Professor and Director of Division of Oral Diagnosis, Department of Diagnostic Sciences, College of Dentistry, University of Tennessee Health Science Center, USA
6Assistant Professor, Department of Pediatric Dentistry and Community Health, College of Dentistry, University of Tennessee Health Science Center, USA
Received:October 21, 2021; Published: November 01, 2021
*Corresponding author: Wells MH, Professor and Director of Graduate Pediatric Dentistry Program, Department of Pediatric Dentistry and Community Health, College of Dentistry, University of Tennessee Health Science Center, USA
DOI: 10.32474/IPDOAJ.2021.07.000252
Introduction
In pediatric dentistry, parents often face challenging scenarios and are required to consider multiple factors in making treatment decisions for their child. When a child is cooperative and the dentist can provide a durable, esthetic restoration, parents’ choice of treatment is relatively simple. However, when advanced behavior guidance techniques are required, factors that parents value most are unknown. In the era of “shared decision making”, pediatric dentists benefit from learning about the parental decision-making process [1]. The purpose of this study was to determine patient decision factors in order to develop a follow-up discrete choice experiment. This type of experiment is used to elicit preferences without asking directly for those preferences from participants. Patients state preferences based upon hypothetical scenarios that contain multiple variables, or attributes. The extent to which these individual attributes vary may be referred to as levels [2]. Attributes, that have been studied in the literature include restorative materials and durability [3-5], cost of treatment [3,6,7], esthetics [3,5,8-11], and risks and benefits of behavioral techniques [7,12,13]. However, these qualitative studies often study these as independent factors or a pair of variables. Few qualitative studies examine complex treatment planning factors concurrently. Other factors may influence the decision-making process: parental socioeconomic status, confidence in the dental provider, previous dental experiences of the patient and parent [14], parental presence or absence, and established fear or anxiety. Few attributes have been assigned levels, meaningful cut-off points at which different choices might be preferred. For example, cost may determine the amount a parent will pay for an esthetic restoration before a less esthetic option is preferable. The purpose of this qualitative study is two-fold:
a)Exploration and description of various aspects of treatment and child behavior that influence parents to choose one treatment modality over another: and
b)Identify attributes and levels parents use to make treatment decisions. A qualitative study design allows participants to independently define attributes and levels considered during the shared decision-making process, rather than providing a set of pre-determined choices as in a typical discrete choice experiment [2].
Materials and Methods
Participants were recruited from three private pediatric dental practices and the University of Tennessee Health Science Center Graduate Pediatric Dentistry Clinic, Memphis, TN. Participants included legal guardians who spoke English and accompanied the child to the appointment. The study was approved by the IRB Review Committee (18-06173-XP), and consent was obtained from each participant. A forty-four open-ended question oral interview survey instrument was used. It consisted of queries regarding various dental treatment options. Sociodemographic information including age, gender, ethnicity, insurance type, education level, and income was collected (Table 1). Participants were asked how many years a child needed his front teeth and back teeth and were asked their knowledge of the safety or risks of sedation and general anesthesia for dentistry. Participants were presented with 2 clinical scenarios using clinical photos as visual aids. The first scenario involved a three-year-old with caries on anterior teeth, and the second scenario involved a very apprehensive five-year-old with eight posterior occlusal carious lesions. Parents were asked to choose from a list of treatment options they would consider. A script was utilized which described different treatment options (along with clinical photographs), behavior guidance techniques, and risks and benefits of each option. Treatment options included Silver Diamine Fluoride (SDF), Interim Therapeutic Restorations (ITR), Stainless Steel Crowns (SSC), Pre-veneered Esthetic Stainless-Steel Crowns, and Zirconia crowns. In scenario 1, behavior technique options, based on the type of treatment, included protective stabilization or moderate sedation, and in scenario 2, sedation or general anesthesia (Table 2). Respondents were asked to explain why they chose a particular treatment and behavior option and how certain they were (scale of 1-10) of their choice. If participants did not discuss attributes that might play a role in the decisionmaking process such as cost, the number of appointments, the site of the treatment, or what treatment the dentist recommended, then pre-determined supplemental, open-ended questions were asked to probe these variables. The survey instrument was piloted prior to administration.
The interview was audio recorded and transcribed into a document (Microsoft Word, Redmond, WA, USA). Transcribed data were categorized and recorded into a spreadsheet (Microsoft Excel, Redmond, WA, USA). Data were analyzed using Statistical Analysis System software (SAS Institute Inc, Cary, NC, USA). Frequencies and percentage statistics were obtained for all categorical variables, including the mean and standard deviation. Categorical variables were utilized to identify attributes and levels. Categorical variables were compared between the two clinical settings, as well as crosstabulations between participant characteristics of interest, utilizing Fisher’s exact test or Wilcoxon-Mann-Whitney test depending on the type of variable.
Results
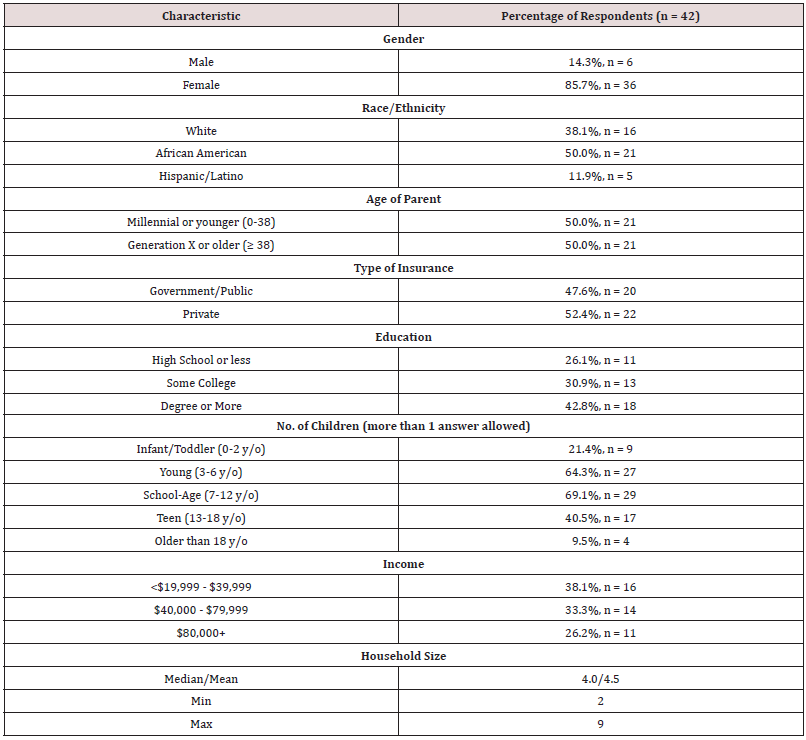
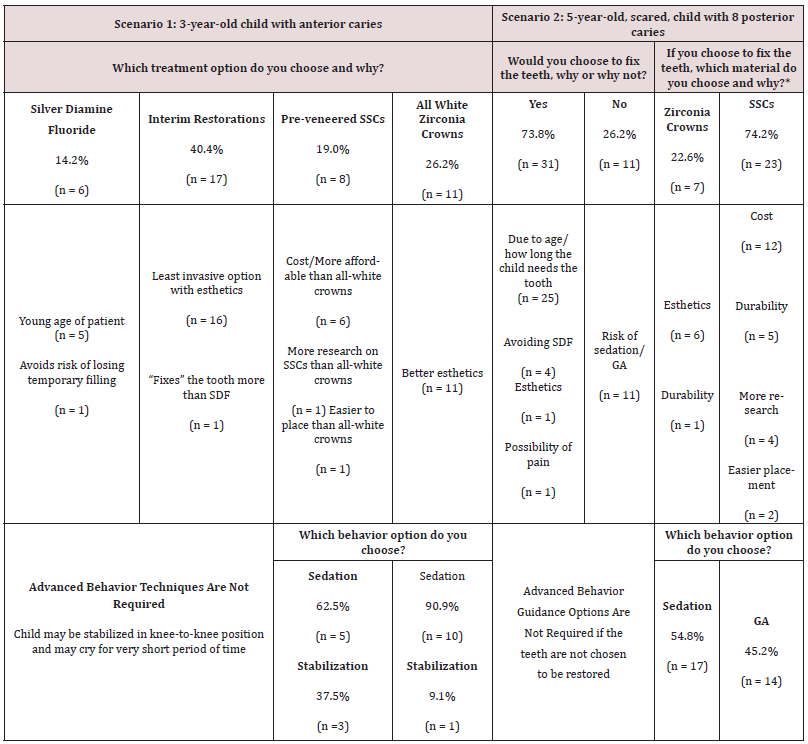
Forty-five individuals were recruited; three declined to participate. Table 1 depicts demographic information of 42 participants. At least 73.7% of respondents had attended some form of higher education. African Americans comprised 50% of the study participants, and over 60% reported having a child three to twelve years of age. The mean household size was 4.5 individuals. Respondents thought a child needed front and back teeth for a mean of 5.5 years and 9.1 years, respectively. Fifty percent of participants (n=21) reported not knowing of any risks of moderate sedation (MS) compared to 38% (n=16) reporting knowing no risks of general anesthesia (GA); the most commonly noted concern for GA was fear of the child not recovering from GA. When knowledge of risks of either MS and GA was cross-tabulated against education, parents with some college education or higher, reported more knowledge of risks for MS and GA compared to participants with less education. However, these findings were not statistically significant (p=0.07 for MS and p=0.78 for GA). Respondents’ preferences of treatment and behavior guidance options are reported in Table 2. For scenario 1, over 40% of participants elected for ITR as a compromise between less invasiveness and esthetics. Over one quarter (26.2%) of respondents selected zirconia crowns for esthetics (despite higher cost), and most chose sedation to obtain the esthetic result (90.9%). Few respondents opted for protective stabilization. When asked on a scale of 1-10 how certain the respondent was of their choice (10 being absolutely certain), the mean response was 8.86.
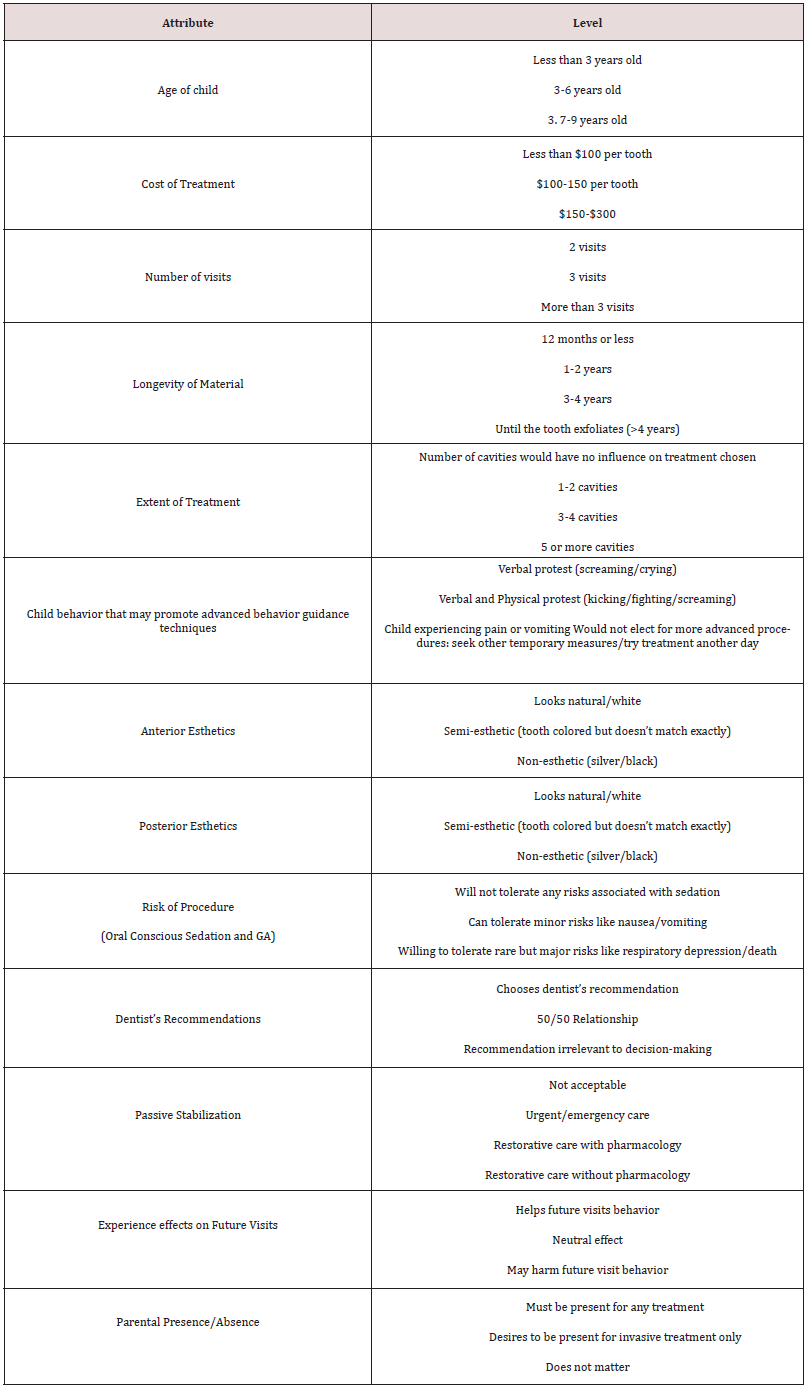
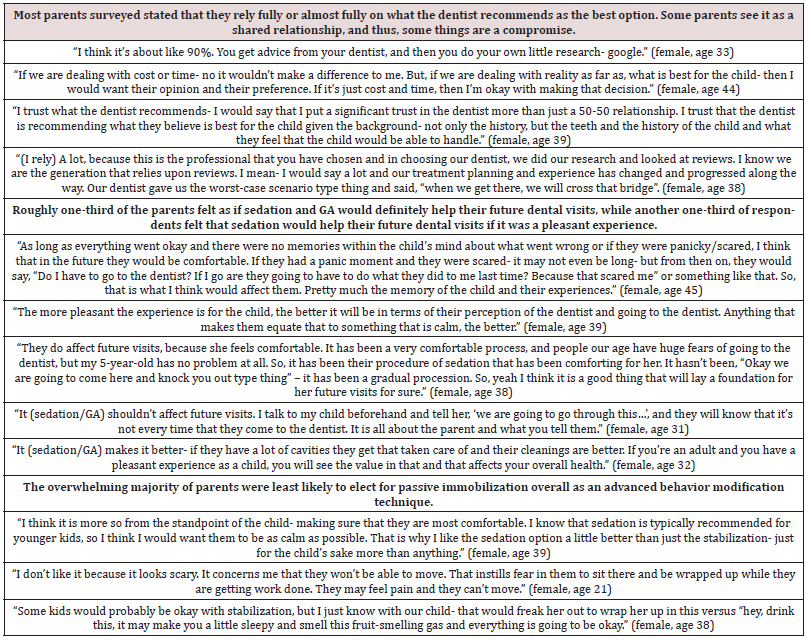
In scenario 2, 73.8% (n=31) of parents chose to restore the posterior teeth considering age of the patient and how long the patient would need his primary molars, while 11 individuals stated they would not restore teeth if MS or GA were required. Those who chose to restore posterior teeth, nearly 75% (n=23), opted for SSCs due to cost, anticipated durability, scientific evidence, and easier placement of SSCs. Regarding behavior, in Scenario 2, individuals that chose MS (54.8%), reported wanting to avoid the perceived risk of GA, while the majority of participants that selected GA wanted to limit treatment to one visit. When asked how certain the respondents were of their choices, with 10 being absolutely certain, the mean response was 8.89. When asked how much a respondent valued the dentist’s recommendation for treatment, 69.1% stated they fully relied on the dentist’s opinion. Table 3 lists all attributes and levels identified through the survey instrument. The levels were determined based on the respondents’ answers to the points at which a different choice might be selected. For example, when asked about behavior that may lead a parent to a pharma logic technique, crying with screaming was the threshold for some while for others it was when the child was physically combative like kicking with crying. Others stated they would not choose pharmacologic techniques regardless of the extent of challenging behavior. Those factors parents reported as not influencing their decision included: need for local anesthetic, dental materials containing plastics or mercury, and fluoride in SDF. Table 4 offers examples of some responses of parents to probing about shared decision-making, beliefs about the effects of MS or GA on future visits, and views on passive stabilization.
Discussion
Parental demand for esthetics has increased over time, but many pediatric esthetic options are more technique sensitive than SSCs and may require advanced behavior techniques to provide the restorations [15]. Recent studies have shown parents as more tolerant of a less esthetic result if it meant avoiding advanced behavior techniques.8 In the current study, respondents were most concerned with esthetics in the anterior region; the majority of parents elected advanced techniques if restorations were desired. Participants who wished to avoid advanced behavior techniques accepted decreased esthetics such as SDF or ITR until the child tolerated treatment without pharmacologic methods. Respondents were more willing to compromise esthetics in the posterior quadrants in order to avoid pharmacologic techniques. In their qualitative study, Maciel et al. found that while children were highly satisfied with posterior SSCs, parents were more likely to choose glass ionomer or composite resin due to these restorations appearing “normal”.11 In the current study there was a high selection (74.2%) of posterior SSCs despite an increase in the demand for overall esthetics. The script did describe each restoration type and included SSCs had long-term scientific evidence showing effectiveness and durability which may have swayed parental opinion. Bell et al. found that most parents were not concerned about SSCs’ appearance in the posterior and were satisfied with SSCs, as they believed the child’s tooth was protected.5 Similarly, respondents in this study reported a desire for durability and long-term success. Passive stabilization was the least favored option of the advanced behavior guidance techniques, a finding similar to previous literature which indicates an increase in parental acceptance of pharmacologic techniques and decreased acceptance of passive immobilization [6].
Individuals who favored restoration did so in both scenarios, indicating that parents who prefer sedation for a young child would tolerate it for a slightly older child. Similarly, nearly all of the participants who selected SDF for Scenario 2 selected the less invasive ITR for Scenario 1. For scenario 2, parents were almost equally divided between MS and GA as a behavior technique. This is the second study for this region of the country that suggests parents readily accept MS and express little concern about adverse events related to in-office MS [12].Parental perceptions in other regions of the country may vary. Parental confidence levels in their choices were high overall for both scenarios, indicating that parents were confident in their treatment selections when given the provider’s input. Limitations to this study include a small sample size due to the nature of a qualitative study. The findings do not consider an array of cultural differences as respondents were regional, native English speakers, of primarily two ethnicities. However, the study population was well distributed in regard to age, education level, income, and type of insurance. This qualitative study displayed hypothetical scenarios; therefore, there is a possibility for response or reporting bias, and social desirability bias. Social desirability bias may have been induced due to parents feeling compelled to select a specific treatment option out of a desire to please the survey administrator or avoid judgment based upon social norms.16 Despite limitations, this study adds to the knowledge base of complex treatment decision-making in pediatric dentistry and lays the foundation for future discrete choice experiments as the authors identified 13 attributes and at least 3 levels with each attribute.
Conclusion
Parents value esthetics in the anterior region, even if achieved through advanced behavior techniques, while passive stabilization is rarely preferred. Parents who wish to avoid advanced techniques will accept fewer esthetic options such as SDF or ITR; overall, parents feel confident in their treatment decisions. This study identified characteristics (attributes) differentiated by values (levels) parents consider when choosing treatment options.
References
- Lipstein EA, Brinkman WB, Britto MT (2012) What is known about parents' treatment decisions? A narrative review of pediatric decision making. Med Decis Making 32(2): 246-258.
- Zickafoose JS, DeCamp LR, Prosser LA (2015) Parents' preferences for enhanced access in the pediatric medical home: a discrete choice experiment. JAMA Pediatr 169(4): 358-364.
- Zimmerman JA, Feigal RJ, Till MJ, Hodges JS (2009) Parental attitudes on restorative materials as factors influencing current use in pediatric dentistry. Pediatr Dent 31(1): 63-70.
- Seale NS, Randall R (2015) The use of stainless-steel crowns: a systematic literature review. Pediatr Dent 37(2): 145-160.
- Bell SJ, Morgan AG, Marshman Z, Rodd HD (2010) Child and parental acceptance of preformed metal crowns. Eur Arch Paediatr Dent 11(5): 218-224.
- Patel M, McTigue DJ, Thikkurissy S, Fields HW (2016) Parental Attitudes Toward Advanced Behavior Guidance Techniques Used in Pediatric Dentistry. Pediatr Dent 38(1): 30-36.
- Kupietzky A (2004) Strap him down or knock him out: Is conscious sedation with restraint an alternative to general anaesthesia? Br Dent J 196(3): 133-138.
- Crystal YO, Janal MN, Hamilton DS, Niederman R (2017) Parental perceptions and acceptance of silver diamine fluoride staining. J Am Dent Assoc 148(7): 510-518.
- Woo D, Sheller B, Williams B, Mancl L, Grembowski D (2005) Dentists' and parents' perceptions of health, esthetics, and treatment of maxillary primary incisors. Pediatr Dent 27(1): 19-23.
- Champagne C, Waggoner W, Ditmyer M, Casamassimo PS, MacLean J (2007) Parental satisfaction with prerendered stainless steel crowns for primary anterior teeth. Pediatr Dent 29(6): 465-469.
- Maciel R, Salvador D, Azoubel K (2017) The opinion of children and their parents about four different types of dental restorations in a public health service in Brazil. Eur Arch Paediatr Dent 18(1): 25-29.
- White J, Wells M, Arheart KL, Donaldson M, Woods MA (2016) A Questionnaire of Parental Perceptions of Conscious Sedation in Pediatric Dentistry. Pediatr Dent 38(2): 116-121.
- Venkataraghavan K, Shah J, Kaur M (2016) Pro-Activeness of Parents in Accepting Behavior Management Techniques: A Cross-Sectional Evaluative Study. J Clin Diagn Res 10(7): 46-49.
- Jafarzadeh M, Keshani F, Ghazavi Z, Keshani F (2011) Reviewing the parental standpoint about origin of the dental fear in children referred to dentistry centers of Isfahan University of Medical Sciences. Iran J Nurs Midwifery Res 16(1): 133-139.
- Fishman R, Guelmann M, Bimstein E (2006) Children's selection of posterior restorative materials. J Clin Pediatr Dent 31(1): 1-4.
- Latkin C, Mai N, Ha TV, Sripaipan T, Zelaya C (2016) Socially desirability response bias and other factors that may influence self-reports of substance use and HIV risk behaviors: A qualitative study of drug users in Vietnam. AIDS Education Prevention 28(5): 417-425.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...