
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Case Report(ISSN: 2641-1725) 
Sudden Death in a 10-Year-Old Boy with Coronary Arteritis and Retroperitoneal Fibrosis – A Case of Takayasu Arteritis Volume 4 - Issue 2
Morild Inge
- Department of Clinical Medicine, University of Bergen, Norway
Received: December 10, 2019; Published: December 17, 2019
*Corresponding author: Morild Inge, Gade Laboratory of Pathology, Department of Clinical Medicine, 5021 Haukeland University Hospital, Norway
DOI: 10.32474/LOJMS.2019.04.000183
Abstract
Takayasu arteritis is an uncommon chronic arteritis of unknown etiology, which primarily affects large vessels, such as aorta and its main branches, resulting in ischemia from gradual stenosis of involved arteries. It may also involve the coronary arteries, and lead to myocardial infarction and sudden death. Misdiagnoses, especially in children is not uncommon. In the present case a 10-year old boy with recently diagnosed retroperitoneal fibrosis and ureteral stenoses died suddenly. In addition to retroperitoneal fibrosis, with affection of the aorta, the autopsy revealed extensive coronary stenosing, and old myocardial infarctions. The findings were interpreted as caused by widespread, unknown Takayasu arteritis.
Keywords: Takayasu arteritis; Coronary arteries; Myocardial infarction; Sudden death; Retroperitoneal fibrosis
Introduction
Takayasu arteritis is an uncommon chronic arteritis, which is more common in South East Asia. The condition has increasingly been recognized world-wide also in Western Europe and North America [1,2]. It is predominantly a disease of young adults, and there is a female preponderance. It is heterogeneous in presentation, progression and response to therapy [3]. It primarily affects large vessels, such as aorta and its main branches, resulting in ischemia from gradual stenosis of involved arteries. The pattern of vessel involvement also varies in different parts of the world [4]. Juvenile Takayasu arteritis is a difficult diagnosis, and some patients develop uncommon manifestations and associated diseases that may contribute to the delayed diagnosis [5]. Takayasu arteritis has also been associated with retroperitoneal fibrosis [6,7]. Although the disease has a prolonged course, and a relatively good prognosis in many patients, cases of sudden death with unrecognized Takayasu arteritis have been reported [8,9].
We report a case of sudden death of a 10-year old boy with retroperitoneal fibrosis where the autopsy revealed widespread, unknown Takayasu arteritis.
Case
A 10-year old boy developed enlarged lymph nodes in the neck, a few months before his death. He had episodes with fever and was treated with antibiotics. Histologic examination of lymph nodes did not show any malignancy, only fibrosis and unspecific reactive changes. Shortly after, he developed symptoms of renal failure, with hydronephrosis and urinary infection. Further examinations revealed retroperitoneal fibrosis. High doses of steroids were given, and stents were inserted between the urinary bladder and the renal pelvises. Still, pyelostomies had to be performed, and the condition stabilized.
Some days before his death, he complained of retrosternal pain, and thereafter lost his conscience. Some muscular contractions were observed. After some minutes he regained his conscience, and the incident was interpreted as an epileptic seizure. Electro encephalon gram (EEG) and magnetic resonance imaging (MRI) did not reveal any pathology. A similar episode happened three days later. Two days after this, the same happened, but was followed by respiratory failure, followed by ventricular fibrillation and thereafter, a cardiac arrest. Despite resuscitative efforts the boy was pronounced dead after one hour, three months after the start of his symptoms.
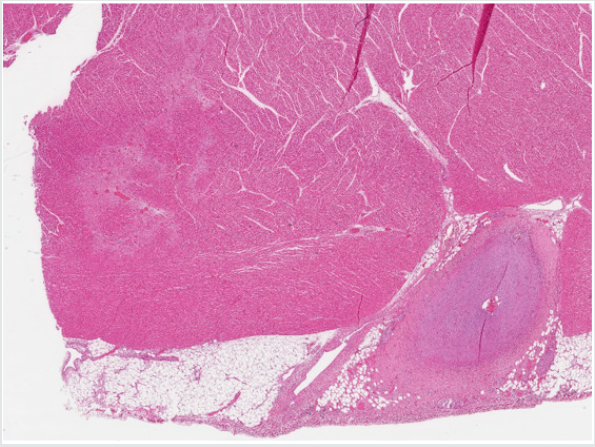
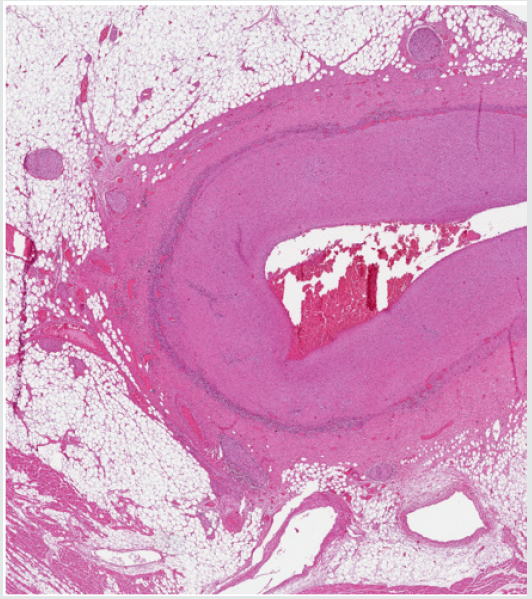
An autopsy was performed 4 days later. The body was that of a normally built boy, 142 cm and 34 kg. The heart weighed 215 g. It was slightly enlarged with some dilatation on the left side. On the epicardial side it was possible to see segmental thickening of the coronary arteries (Figure 1A & 1B). Transverse sections of the coronary arteries showed thickening of the walls, with only pinpoint size lumina (Figure 2). In the left ventricular myocardium, small fibrous areas could be seen macroscopically. Microscopically, these areas could be found as fibrous lesions, with some hypertrophied myocardial fiber nuclei, indicating older myocardial infarctions (Figure 3). No obvious recent myocardial infarctions were found. The histologic examination revealed heavily thickening of the arterial walls, mostly due to fibrous changes in the intima, sometimes with extreme narrowing of the arterial lumen. Patchy aggregates of lymphocytes were found in the intima, but such aggregates were much more pronounced along the border between the arterial intima and the media. A constant finding were a number of hypertrophied nerve fibers along the coronary vessels (Figure 4). No necrosis, granulomatous areas or giant cells were found.
Figure 1: Positive Correlation between Parasite Density and IL-6 Plasma Levels in Children Infected with P. falciparum (r=0.43; P<0.0001).
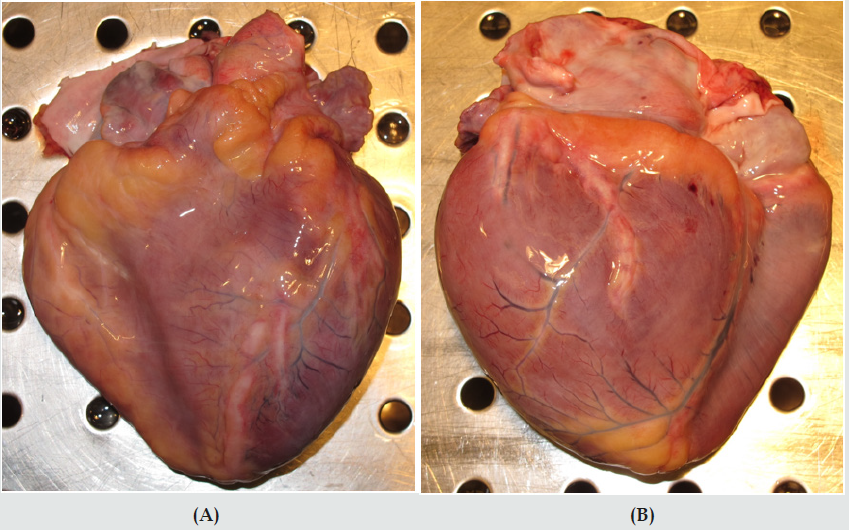
Figure 2: Microscopical transverse section of an epicardial coronary artery with severe thickening of the wall, mostly due to intimal fibrosis, with only a pin-point size lumen (hematoxylin and eosin stain).
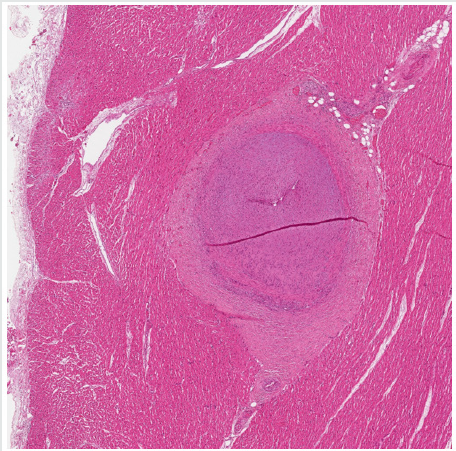
Figure 3: Left ventricular myocardium, with myocardial scarring and hypertrophic myocardial fiber nuclei together with affected artery (hematoxylin and eosin stain).
The aorta was of normal size in the thoracic and upper abdominal part, but below the level of the renal arteries, the aorta was surrounded by dense connective tissue, and the aortic diameter was severely reduced, due to compression from fibrosis and thickening of the arterial wall. Histology revealed similar changes as in the coronaries, with fibrosis and with a lymphocytic infiltrate between the intima and the fibrous media. Extensive lymphocytic aggregates were also found in the adventitia and in the surrounding fibrous and fatty tissue (Figure 4). Here, also a number of hypertrophied nerve fibers were found. The kidneys were of normal size, with slightly dilated pelvises with pyelostomy catheters. The ureters were heavily infiltrated with lymphocytes, and surrounded by fibrous tissue, leading to obstruction of the lumina. The other organs were unremarkable. Postmortem toxicology was negative. The death was attributed to acute heart failure due to extreme narrowing of the coronary arteries and old myocardial infarctions.
Figure 4: Epicardial coronary artery, with moderate fibrosis. Inflammatory infiltrate along the border zone between the intima and the media, and hypertrophic nerve fibers on the adventitial side (hematoxylin and eosin stain).
Discussion
Takayasu arteritis is an inflammatory disease often involving the aorta and its main branches. The inflammation can result in varying degree of stenosis, luminal irregularity, but also in dilatation and aneurysms. Thoracoabdominal involvement of the aorta is reported to be more common in children [10,11]. The disease has an early active inflammatory, and a late chronic phase. Symptoms like fever, anorexia, night sweats and skin rash may be present in the active phase. In the present case the boy had cervical gland enlargement and episodes with fever three months before his death. This may have been symptoms from the active phase of the disease. Later, his symptoms were mainly from his ureteral stenoses, until he had symptoms interpreted as a form of epilepsy. Retrospectively, this may have been symptoms of a cardiac arrhythmia as the autopsy revealed scarring in the myocardium together with severe narrowing of coronary arteries. We believe that the cause of death is a cardiac arrhythmia, caused by the extensive stenoses in the coronary arteries.
Heart failure from Takayasu arteritis in children is mostly caused by hypertension and may be misdiagnosed for a dilated cardiomyopathy [4]. The diagnosis of Takayasu arteritis is relatively uncommon in Norway, especially in boys, increasing the chance of a late diagnosis or a misdiagnosis. Coronarial involvement has only been reported in 5 - 10 % of adult patients [4,9]. The incidence of coronarial involvement in children has not been studied.4,9 Some case studies have been reported [8,9,12].
There have been reports of a connection between retroperitoneal fibrosis and Takayasu arteritis. The association between retroperitoneal fibrosis and Takayasu arteritis is, however, very complex and rare, and only few cases have been reported in the literature [6,7,13-16]. We have no explanation for the hypertrophied nerve fibers found on the adventitial side of the affected arteries.
We believe that in a case of suspected Takayasu arteritis, a thorough cardiac examination, preferably with coronary angiography should be considered.
References
- Judge RD, Currier RD, Gracie WA, Figley MM (1962) Takayasu's arteritis and the aortic arch syndrome. Am J Med 32: 379-392.
- Lande A, Bard R, Rossi P, Passariello R, Castrucci A (1976) Takayasu's arteritis. A worldwide entity. NY State J Med 76(9): 1477-1482.
- Kerr GS, Hallahan CW, Giordano J, LeavittRY, Fauci AS, et al. (1994) Takayasu arteries. Ann Intern Med 120(11): 919-929.
- Kothari SS (2001) Takayasu’s arteritis in children - a review. Images Paediatr Cardiol 3(4): 4-23.
- Clemente G, Silva CA, Sacchetti SB, Ferriani VPL, Oliveira SK, et al. (2018) Takayasu arteritis in childhood: misdiagnoses at disease onset and associated diseases. Rheumatol Int 38(6): 1089-1094.
- Vaglio A, Salvarani C, Buzio C (2006) Retroperitoneal fibrosis. Lancet 367(9506): 241-251.
- Hardmeier T, Hedinger C (1964) The relationship between retroperitoneal fibrosis and so-called Takayasu's arteritis. Schweiz Med Wochensch 94: 1669-1676.
- Jedidi M, Chkirbene Y, Abdessayed N, Masmoudi T, Mahjoub M, et al. (2017) Sudden Death Due to Unusual Complication of Takayasu Arteritis: An Autopsy Case. Am J Forensic Med Pathol 38(2): 91-93.
- Hlavaty L, Diaz F, Sung L (2015) Takayasu Arteritis of the Coronary Arteries Presenting as Sudden Death in a White Teenager. Am J Forensic Med Pathol 36(3): 221-223.
- Shrivastava S, Srivastava RN, Tandon R (1986) Idiopathic obstructive aortoarteritis in children. Indian Pediatr 23(6): 403-410.
- Hahn D, Thomson PD, Kala U, Beale PG, Levin SE (1998) A review of Takayasu's arteritis in children in Gauteng, South Africa. Pediatr Nephrol 12(8): 668-675
- Otukesh H, Fereshtehnejad SM, Hoseini R, Zabihi A, Tafreshi R, et al. (2008) Extensive myocardial infarction in a child with Takayasu vasculitis: Report of a case and literature review. Iran J Pediatr 18(4): 364-368
- Jghaimi F, Kabbaj A, Essaadouni L (2010) Takayasu's arteritis and retroperitoneal fibrosis: A case report. Rev Med Interne 31(3): e1-e3.
- Fajacc A, Galezowski N, Cormier JM, et al. (1988) Artérite inflammatoire type maladie de Takayasu et fibrose rétropéritoné Rev Med Interne 9:436-437.
- Houman H, Haouet S, Lamloum M, Ghorbel IB, Miled M (1998) Retroperitoneal fibrosis associated with Takayasu arteritis. Ann Med Interne 149(2): 107-108.
- Aslangul E, Ranque B, Papo T (2003) Pseudotumoral retroperitoneal fibrosis and localized vasculitis with very high serum levels of anti-PR3 ANCA. Am J Med 115(3): 250-252.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




