Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Case Report(ISSN: 2641-1725) 
Not All Diabetics with High Anion Gap Acidosis are Diabetic Ketoacidosis- A Case Report of Starvation Ketoacidosis in a Diabetic Patient Volume 3 - Issue 5
Ali Hussain1, Hira Yousuf1 and Akbar Mahmood1* and Albusaidi Fadhila2
- 1Sultan Qaboos university Hospital, Oman
- 2Ministry of Health, Oman
Received: October 01, 2019; Published: October 09, 2019
*Corresponding author: Akbar Mahmood, Sultan Qaboos university Hospital, Oman
DOI: 10.32474/LOJMS.2019.03.000171
Introduction
Metabolic acidosis is a metabolic disorder characterized by an abnormal increase in acid production or reduces elimination of the generated acid into the body. Ketoacidosis is one of the main causes of metabolic acidosis. It is usually caused by different etiologies including Type 1 diabetes mellitus (DM) or ketone prone Type 2 diabetes mellitus, alcoholism and starvation. Isolated starvation ketoacidosis is a rare condition with unrecognized phenomenon. Herein, we are reporting a case of 24-year-old female with isolated starvation ketoacidosis.
Case Presentation
A 24-year-old young unmarried woman with a past medical history of end stage renal disease (ESRD) is on regular hemodialysis three times per week via permcath. Renal failure was caused by atypical hemolytic uremic syndrome. She underwent renal transplant which was failed unfortunately due to rapid recurrence of primary disease in the renal allograft within a year time. In addition to that she was diagnosed with diabetes mellitus post transplantation secondary to steroids and Tacrolimus, a condition named new onset diabetes after transplant (NODAT). She is chronically malnourished secondary to anorexia. She attended emergency department with cath related bacteremia with history of negligible oral intake for the last five days before presentation which was associated with nausea and few episodes of small volume, non-bilious non-bloody vomiting. She also complained of epigastric pain which was moderate to severe in intensity, present throughout the day and radiating towards the back without any aggravating or relieving factors. Patient denied history of loose motion malena or fresh blood in the stools, was anuric due to her ESRD. She is a lifelong teetotaler and non-smoker. On general examination she appeared sick and in distress secondary to pain. Abscess was found on the tunnel of Permacath site on the left pectoral region. Abdominal examination revealed epigastric tenderness, palpable, non tender renal allograft into right iliac fossa. There were no clinical stigmata of infective endocarditis.
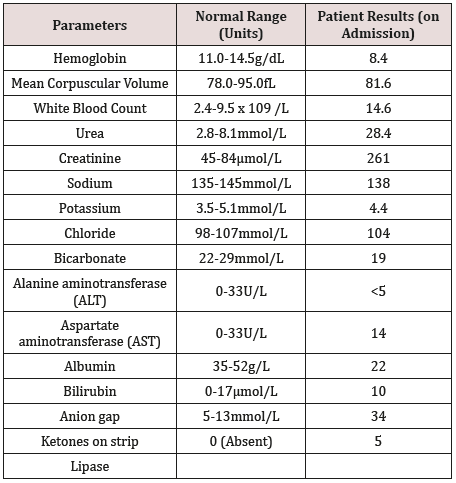
On laboratory assessment labs are shown in Table 1. She had polymorph nuclear leukocytosis, found to have methicillin resistant staph aureus later on. Significant high anion gap metabolic acidosis was found with capillary ketones positive up to 5 plus (on ketone strip) and normal osmolality and osmolar gap. Serum lactate and glucose levels were normal on admission. Ultrasound abdomen was ordered which showed evidence of mild to moderate nonbiliary pancreatitis. X-ray chest was unremarkable.
Her infected catheter was removed immediately, and empirical antibiotics commenced, covering for both gram positive and negative organisms. Furthermore, she was diagnosed to have acute pancreatitis with a working diagnosis of possible euglycemic diabetic ketoacidosis in context of normal blood sugar, high anion gap and positive ketones concomitant with renal failure as a further cause of acidosis. Hospital course was complicated further with development of cerebro vascular event due to septic emboli which led to depress consciousness, right hemiparesis and inadequate swallowing resulting into hampered intake orally. She strongly refused for insertion of Naso-Jejunal tube (NGT) and kept nothing per oral (NPO) protocol. As patient had anuric ESRD so she was given intravenous fluid very cautiously to avoid fluid overload and started on insulin infusion according to modified local DKA protocol. Additionally, maintenance hemodialysis continued through a temporary dialysis catheter access but her high anion gap and ketones were failed to improve. In context of her poor intake before hospital admission, malnourishment due to her comorbid conditions and continued NPO status due to stroke and pancreatitis, we reviewed the aforementioned working diagnosis and considered starvation as cause of ketosis. Considering this fact she was counseled again about the importance of feeding and Naso-Jejunal tube insertion as a mean to feed, she was agreed and hence after uneventful insertion of NGT, started on renal enteral nutrition which provided 172 grams of carbohydrate per 24hrs which was further increased to 250gms in the next 24 hours. Concurrent intravenous thiamine was administered and she was monitored closely for development of refeeding syndrome by checking electrolytes and trace elements on daily basis. Her anion gap started to improve swiftly and later became normalized along with disappearance of ketones, as shown in Graph-1.
Graph 1: shows that swift drop of AG on day 2 after the start of naso-jejunal feed and normalization of AG on day 3 with disappearance of ketones. Day 1 was the day of admission.
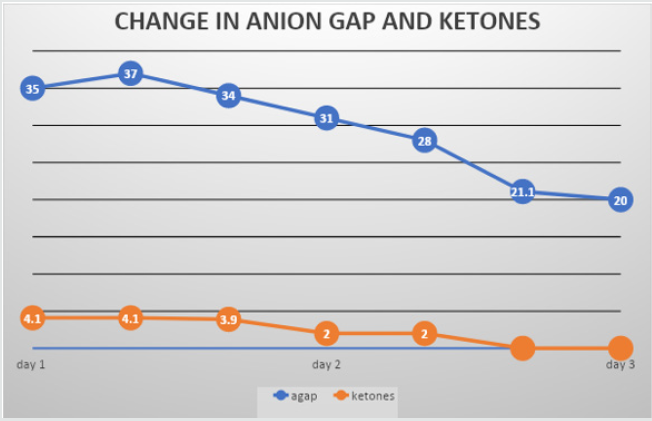
Disappearance of ketone bodies and dramatic improvement of anion gap in an already starved patient confirms the diagnosis of starvation ketosis.
Discussion
Metabolic acidosis with high anion gap and presence of ketones in the blood is called Ketoacidosis. The most common cause of ketoacidosis is diabetic ketoacidosis but other recognized causes are euglycemic ketosis, alcoholism, pregnancy with hyperemesis and starvation as shown in Table 2. Starvation ketoacidosis is a rare and not a commonly recognized condition and is often confused with euglycemic diabetic ketosis especially in diabetic patients. This fact must be bore in mind when dealing with such conditions because it is entirely a different clinical entity which merits separate management.
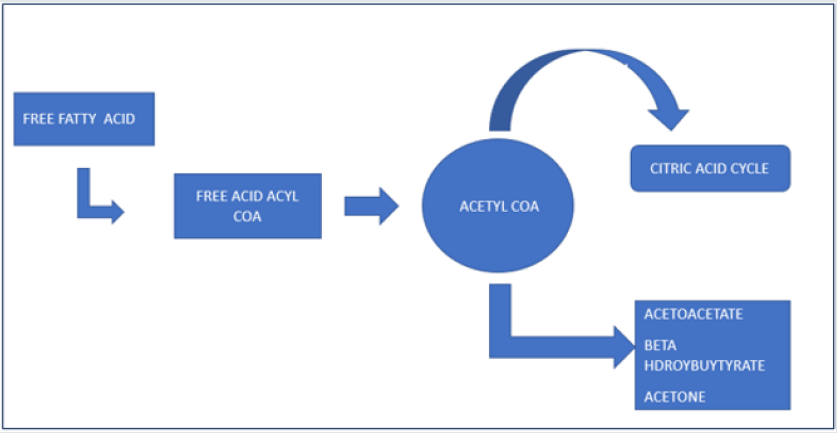
Under optimal physiological condition with adequate glucose supply and normal insulin secretion, glycolysis produce pyruvate which generates energy by production of ATP via enters the citric acid cycle. Starvation results in the production of glucose from non carbohydrate precursors. Mechanism of formation of ketone bodies is shown in Figure 1. Fatty acids are mobilized from adipose tissue and gluconeogenic and ketogenic pathways are activated in the liver. The released fatty acids are transported to the liver and extra hepatic tissues where they are oxidized in the mitochondria resulting into formation of ATP molecule. However, the increased supply of fatty acids to the liver results in an abundance of acetyl coenzyme A (COA) which exceeds the capacity of citric acid cycles thus ketone bodies are formed. Three well known ketone bodies are beta hydroxy butyrate, acetoacetate and acetone [1]. Beta-hydroxy butyrate and acetoacetate becomes a source of an alternative energy supply for the body at the cost of metabolic acidosis. Ketone body production maximizes after starvation period of at least three days and is usually eliminated by kidneys, either by oxidation (∼60 %) or by urine (∼40%) [2]. The fraction of ketoacids is oxidized by the gastrointestinal tract [3] and by conversion to acetone, which can be detected on the patient’s breath [4] Unlike patients with diabetic ketoacidosis, patients with starvation ketosis release insulin when carbohydrate is administered. They also produce high levels of glucose elevating hormones such as glucagon and have depleted glycogen stores. These hormones cause the lipolysis which helps generate ketones which are utilized for fuel. The addition of exogenous insulin in this state risks hypoglycemia. Once provided with adequate carbohydrates, the insulin levels will rise and counter regulatory hormone levels will fall, resolving the ketosis [5]
Similarly, Alcoholics are another group prone to ketosis (alcoholic ketoacidosis (AKA). However they are particularly prone to develop hypoglycemia as a complication secondary to the administration of insulin therefore, such patients need to be treated with extreme care with frequent monitoring of blood sugar to deal with hypoglycemic episodes timely. There is limited evidence that insulin improves alcoholic ketoacidosis outside the case reports [2]. Our patient is a lifelong teetotaler additionally there is no osmolar gap thus exclude the presence of on additional toxic alcohol such as ethanol.
Euglycemic ketoacidosis has been reported with a normal sugar level in diabetics or in those receiving sodium–glucose cotransporter-2 (SGLT-2) inhibitors, both of which were not relevant in our patient. Our patient was not on SGLT-2 inhibitors additionally there was no change in the anion gap and ketone level after the commencement of insulin infusion.
Pregnant women especially those who develop hyperemesis gravidarum are prone to develop starvation ketosis. Vomiting leads to loss of gastrointestinal contents and inadequate intake, both contributes to starvation and it`s ill effects. Several hormones generated in pregnancy, including progesterone, cortisol, and human placental lactogen can contribute to a diabetogenic state presenting as insulin resistance, increased lipolysis, augmented production of free fatty acids and ketogenesis [6,7]. However, in our case patient is not pregnant so excludes hyperemesis gravidarum.
The mainstay treatment of starvation ketoacidosis is to supply sufficient amount of carbohydrates so that body overcome production of ketones bodies and thus improvement of the anion gap. In our case after starting patient on naso-jujenal feed with adequate carbohydrate content patient`s anion gap started to improve and ketones disappeared from the blood.
Conclusion
Starvation ketoacidosis in one of the important possible causes of ketoacidosis especially in patients with poor oral intake which is a usual consequence of most of the illnesses which leads to overproduction of ketone bodies consequently.This process starts within hours, even before hospital admission. This condition is not as uncommon as it is thought of, oftently goes unnoticed because of non-familiarity of this condition. Prompt diagnosis requires a high index of suspicion especially when patient is nonalcoholic and failure of anion gap to improve with insulin therapy.
Disclosure
None of the authors has a financial relationship with a commercial entity that has an interest in the subject of the paper. No financial support was used for the study.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- Ketone B, Barnett CR, Barnett YA (2003) University of Ulster at Coleraine, Coleraine, County Londonderry, Northern Ireland Copyright, Elsevier Science Ltd.
- Owen OE, Felig P, Morgan AP, Wahren J, Cahill GF (1969) Liver and kidney metabolism during prolonged starvation. J Clin Invest 48(3): 574–583.
- Windmueller HG, Spaeth AE (1975) Intestinal metabolism of glutamine from the lumen as compared to glutamine from the blood. Archiv Biochem Biophys 171(2): 662-672.
- Davids MR, Segal AS, Brunengraber H, Halperin ML (2004) An unusual cause for ketoacidosis. 97(6): 365-376.
- QJM (2004) An International Journal of Medicine. 97(6): 365–376.
- Hammerbeck H, Holland MR (2017) Starvation ketoacidosis: Treatment pitfalls Journal of the Intensive Care Society 18(3): 265.
- Hui L, Shuying L (22018) Acute starvation ketoacidosis in pregnancy with severe hypertriglyceridemia: A case report. Medicine (Baltimore) 97(19): e0609.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...