
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1725
Research Article(ISSN: 2641-1725) 
Exploring Patient’s Experiences Attending a Joint Complex Airway Clinic Volume 3 - Issue 2
Muhammad Imran Qadir and Noor Arif*
- Institute of Molecular Biology and Biotechnology, Bahauddin Zakariya University, Multan, Pakistan
Received: March 14, 2019; Published:March 25, 2019
*Corresponding author: Alexandra Charnock, ENT, Alder Hey Children’s Hospital, UK
DOI: 10.32474/LOJMS.2019.03.000159
Abstract
Background and Objectives
Tracheostomies in children are increasingly common; subsequently, the need for coordinated multidisciplinary care of tracheostomy patients has become better recognised. This study explored the patient’s experience of attending a joint complex airway clinic at Alder Hey Children’s Hospital, examining patient satisfaction and their perceived level of involvement in the decisionmaking process. As well as, exploring whether the examination of their child’s dynamic airway improved their understanding and confidence in managing complex airways independently. Finally, it aimed to determine the impact the clinic had on the number of airway endoscopies required under general anaesthesia.
Methods
The joint complex airway clinic at Alder Hey Children’s Hospital is a multidisciplinary clinic with both ENT and respiratory teams present to manage children with tracheostomies and long-term ventilation needs. Additionally, it provides the opportunity for airway examination under local anaesthetic. This qualitative prospective study used feedback questionnaires, completed by parents/carers after attending the clinic; to obtained rated responses regarding the clinic set up and effectiveness. Those participating patients were then followed up to determine their need for further invasive airway endoscopies under general anaesthesia.
Results
The study suggested an overall satisfaction in the format and care provided by the clinic. In addition, it resulted in a large decrease in the need for endoscopies under general anaesthesia (95%).
Conclusions
These findings suggest the new service format has the potential to significantly benefit patient care in the future, as the need for long term tracheostomy care is ever expanding.
Abbreviations:ENT: Ears, Nose and Throat; MLTB: Microlarngotracheo bronchoscopy
Introduction
It is becoming increasingly common for children to receive tracheostomies due largely to the continued improvement of medical practice at developing new ways to extend the life expectancy of children with multifaceted diagnoses [1]. Most tracheostomies are performed in complex patients with sustained reliance on long term ventilation for survival [2,3]. Unfortunately, children like these are at higher risk of increased morbidity and mortality, typically secondary to their comorbidities [2,4]. Therefore, because of the collaborative management required for these types of complex paediatric patients, a coordinated multidisciplinary approach to tracheostomy care is optimal [5-7]. Besides, studies have shown that most tracheostomy-related adverse events are preventable, and that disorganised care and health information mismanagement are some of the major issues that hinder optimal tracheostomy care [1,7,8]. Suggesting, coordinated care is one way to better secure patient’s safety. Furthermore, the long-term management of tracheostomies including re-sizing and decannulation is not standardised, and highly variable depending on the indications for the tracheostomy and stage of patient development [9]. As such, a consistent multidisciplinary approach to the long-term management of a patient’s physical and medical needs is required [9].
Alder Hey Children’s Hospital in Liverpool, UK, provides secondary care to the children of Liverpool, but tertiary care to the children of a large catchment area including the Northwest of England, Isle of Man and Wales. Travel times for some families are over two hours by car and some from the Isle of Man take a day with return flights. Hence, the joint complex airway clinic service, which combines respiratory, ears, nose and throat (ENT), and allied healthcare services in a single out-patient clinic, was initially started to help minimise travel for families to multiple appointments and provide a more substantial dedicated service for the assessment of children with specific tracheostomy care needs. In addition, conventionally at Alder Hey Children’s Hospital, children with tracheostomies required an annual airway endoscopy under general anaesthetic to monitor and address issues of sizing (as the child grows), morphological appearance of the trachea and bronchi, and the development of any complications like intra-tracheal and stomal granulations. All of which can henceforth be provided as part of the new joint clinic service, with airway endoscopies being performed under local anaesthetic and scrutinised in real time by those clinicians and patients’/carers’ in attendance.
Aims
Being a novel outpatient service provision, modelled on the premise of multidisciplinary management, our primary objectives for this qualitative prospective study were to explore and analyse patients’ and parents’/carers’ experiences of attending the specialised joint respiratory and ENT complex airway clinic at Alder Hey Children’s Hospital. Specifically, this study focused on patient/ parental/carer satisfaction with the joint complex airway service and their perceived involvement in the decision-making process. We explored whether the examination of the child’s dynamic airway under local anaesthetic during the clinic appointment improved their understanding and confidence in managing the complex airway independently at home. In addition, we assessed the effectiveness of providing focussed tracheostomy care in a multidisciplinary set up by determining the number of additional elective airway endoscopies required under general anaesthesia.
Methods
Clinic Format
The joint complex airway clinic at Alder Hey Children’s Hospital, is a multidisciplinary setup led by ENT and respiratory consultants. Children who attend are normally aged anywhere from less than one to sixteen years of age. The patient group the clinic manages are children with a tracheostomy, with or without long term ventilation needs. They are routinely seen on a regular basis, the frequency of which is dependent on the individual’s clinical findings on review. The clinic visit is for a regular physical examination and review of any new concerns or complications associated with their airway care. This clinic can run instead of or in addition to regular appointments with the individual ENT and respiratory teams. Each session usually lasts between 45-60 minutes long. In addition to ENT and respiratory consultants, other relevant junior doctors, specialist nurses, allied health teams, community nurses, parents/ carers, as well as the tracheostomy patients themselves are all in attendance at the clinic appointment.
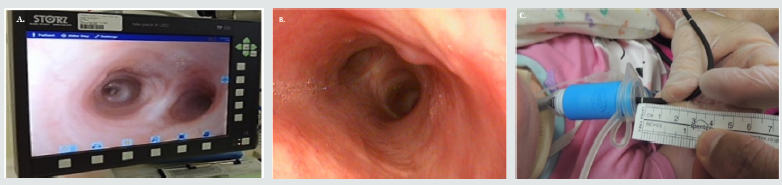
Like any clinical assessment, there is a review of the relevant history including the current tracheostomy tube size and length, frequency and or issues with tube changes, quantity of secretions, episodes of tracheostomy site bleeding and an overview of the general well-being of the child. The physical examination involves a nasolaryngoscopy (if required) and tracheoscopy, both of which can be performed on a conscious child in the clinic setting. The child is first administered local anaesthesia consisting of 5ml of diluted solution (1ml of 1% lignocaine with 4ml normal saline solution), delivered through the tracheostomy tube in a staged manner using 1ml spray bursts given over five minutes. Depending on the tracheostomy tube size, an appropriately sized paediatric flexible endoscope (Karl-Storz) is used to visualise the airways, as demonstrated in (Figure 1a). The full airway assessment includes examination of the trachea in addition to the right and left main bronchi looking at the morphological appearance of the tracheal lumen, its direction and mucosal appearance, and assessing for the presence of secretions or mucosal granulations (Figure 1b). The examination is made with the tube in-situ and without the tracheostomy tube. As depicted in Figure 1c, the distance of the tracheostomy tip from the carina is measure and the need for upsizing or downsizing the tube is noted.
This regular examination determines the health and suitability of the current tracheostomy, and a decision regarding the need for a furthermore detailed assessment and or procedures under general anaesthetic is made. If non-invasive procedures (i.e. application of silver nitrate) for stomal granulation is needed, it can be done at this time. Example images from a tracheoscopy procedure performed under local anaesthetic during a clinic session obtained with patient permission (Figures 1a-1c). Parents and carers are present at the time of the examination to visualise the patient’s dynamic airway. They are actively encouraged to be involved in the process by doing the suctioning of the child’s tracheostomy tube and participating in the ongoing discussion about the child’s airway and its appearance. The recordings are stored on the hospital computer systems and replayed afterwards when making decisions about future management between all teams and respective parents. The digital recording is then available to use during future discussions on the child’s progress. If requiring a further procedure under general anaesthetic, an operation date and time can be sorted out during the same clinic appointment.
Figure 1: Example images from a tracheoscopy procedure performed under local anesthetic during a clinic session obtained with patient permission. A: Still image of the clinical examination of a child’s airways using a flexible endoscope, demonstrating normal anatomy of the tracheal lumen, carina, and both main bronchi. B: Captured image of child’s trachea lumen, with visualization of the carina, both main bronchi, and a granuloma (arrow) on the anterior wall. C: Clinical examination of a child’s airway using a flexible endoscope and conducting measurements for tube sizing.
Study Methods
At the conclusion of the appointment the parents and cares were requested to complete an anonymised questionnaire in the waiting area and were asked to leave it with the receptionist. If for some reason this was not possible or if they chose, the questionnaire could be completed over the telephone. Overall, not all patients that attend the clinic participated in the study due to personal preference. However, of those that did take part, only one questionnaire was complete for each patient as a general representation of their experience, regardless of how many individuals contributed to answering the questionnaire. The questionnaire used rating scales (1-10) to score the responses from negative to positive for several questions about the clinic service. Their responses regarding their experiences attending the joint complex airway clinic were then collated and analysed, giving qualitative feedback about the service.
In addition, follow-up of all those families whom participated in the study was done to determine if those children needed a further microlarngotracheobronchoscopy (MLTB) under general anaesthetic in addition to this clinic review, due to inadequate examination. This value was compared to data from previous years for those participating children, whom previously followed the standard practice of routine annual airway endoscopies under a general anaesthetic. The study was conducted prospectively over a six-month period. It was registered with the hospital and deemed exempt from further ethical approval.
Results
The patient feedback questionnaires suggested an overall positive opinion about the joint complex airway clinic. Of those parents/carers who participated (39), 77% (n=30) preferred the multidisciplinary set up of the joint complex airway clinic rather than separate ENT and respiratory clinics. In regards to specific service goals, 92% (n=36) felt included in the decision-making process regarding the future management of their child’s complex airway, 90% (n=35) felt that enough time was allocated in the clinic for adequate discussion and decision-making, and 97% (n=38) preferred the airway examination under local anaesthesia in clinic rather than under general anaesthetic. In terms of the educational benefits of the clinic, 89% (n=35) felt that the dynamic airway videos improved their understanding of their child’s complex airway, 97% (n=38) felt that they were given enough information about managing their child’s airway, and 72% (n=28) felt increased confidence about the handling of the child’s airway care independently at home after attending the clinic. In addition, of those children whose families participated in the study, there was a reduction in the need for surveillance airway endoscopies under general anaesthesia by 95%. Of those that did have to go on to have a further general anaesthetic examination, it was unavoidably required due to best medical practise prior to an attempted decannulation.
Discussion
Due to the complex medical needs of patients with tracheostomies and long-term ventilation requirements, the input from multiple different healthcare departments is necessary to provide safe holistic care. Effective management of these complex patients is dependent on appropriate, timely, and relevant communication between and among the different departments and the patient. Substandard communication is a known area of weakness in the health system that can have a drastic impact on the effective care of complex airways [8]. The joint airway clinic provides a dedicated service for children with specific complex tracheostomy care needs. Using a multidisciplinary clinic approach helps to avoid miscommunication or misunderstanding among the relevant parties regarding the patient’s condition and management plans [10]. It also reduces the possibility of errors or delays in communication which can occur between teams during the process of organising treatment/procedures/follow-up, as multiparty discussions are held during a single appointment. In our observed practice, the clinic has helped identify children needing further intervention and improved the efficiency of arranging further surgical procedures in accordance with the specific needs of the child and family.
What is more, the joint clinic reduces the number of individual clinic appointments that patients must attend which is potentially more convenient for the family regarding time/travel/cost/ employment/childcare [11]. It is also beneficial for these medically complex children as it can reduce their exposure to the hospital environment, limiting the psychological stress associated with multiple attendances and examinations, and reducing the physical risk of infection exposure [12]. A further assessment of which specific aspects of quality of life and care are impacted and or improved by this joint clinic would be an interesting expansion of the study, to determine the potential benefits it provides in addressing holistic patient care. From a departmental point of view, joint clinics could potentially reduce the number of nonattendance among patients and preserve the time and resources of the healthcare teams involved [11]. It could streamline the use of resources and prevent repetitive or unnecessary assessments by multiple teams that are otherwise unable to communicate or coordinate care effectively [10]. It is impossible to know for sure without further analysis, but this multidisciplinary system could be more efficient and cost effective to the health service [13].
Although, the multidisciplinary clinic requires significant organisation to coordinate all the members involved, it provides a unique environment for both the ENT and respiratory teams to look at the dynamic airway in real time. Therefore, both teams can interpret the findings together and thus come to a joint management plan. This has already shown to greatly reduce the need for further invasive diagnostic procedures, by either team. Previously, annual general anaesthetic examinations of the patient’s airway were an essential part of the children’s longterm complex airway management. It not only determined the health of the tracheostomy but also the patient’s suitability for possible decannulation. However, any paediatric procedure done under general anaesthetic is complex to organise, expensive, and carries significant risk to the patient. Children have about double the risk of a major or minor side effect to anaesthesia, compared to adults [14]. Although the most common side effect of general anaesthesia in children over the age of five, nausea and vomiting, can be consider relatively mild in complex patients with several co-morbidities managing even minor reactions can be difficult and compounding particularly in even younger children [14]. Not to mention, the significant psychological impact that repetitive stress associated with procedures under general anaesthesia can put on these vulnerable children [15,16]. The seemingly obvious benefits to patients and the health service provided by completing airway examinations in the clinic setting under local anaesthetic rather than in theatre under general anaesthetic, requires further quantitative assessment.
Most importantly, our parent/carer feedback shows a general approval in the multidisciplinary complex airway clinic set up. Patients only must attend one clinic in which they get more time specifically allocated to their issues. Parents believe the clinic set-up with the use of dynamic airway images is informative. Thus, improving their understanding of their child’s airway/ tracheostomy, and increasing their confidence in managing any airway issues independently at home. Consequently, by optimising parental/carer’s tracheostomy care knowledge, the children’s safety and the stress burden on the parents is improved [17]. Lastly, parent/carer participation in the real time observation of the dynamic airway and the subsequent decision-making process provided a unique experience. The parents felt they were involved in management decisions, which has been found to be a key factor in impacting patient safety and quality of care [18]. In a patient centred care system like the NHS, such positive feedback is an essential marker of successful care delivery.
Limitations
The potential for this type of multidisciplinary team clinic setup is only possible in tertiary paediatric hospitals which support specialised care for tracheostomy and ventilator patients. Moreover, it requires the facilities and staffing to run the joint clinic and complete airway assessments under local anaesthetic. Therefore, a study of this clinic format is limited in its generalizability to services provided by other less specialised paediatric departments. In terms of study design, confounding variables would have been introduced with the variability in patient experiences prior to attending the joint airway clinic at Alder Hey Children’s Hospital. Most patients who attend this joint airway clinic would have be under review by teams at Alder Hey Children’s Hospital for the duration of their childhood. However, as the clinic was ongoing for a year prior to the study, there could be a variety of new or transferred patients who would have different comparative experiences; consequently, skewing questionnaire responses. Though, the questionnaire was designed so all patients could participate, regardless of their clinical history and previous clinic experiences. Furthermore, the study involved requesting patient participation or conducting telephone interviews by clinical staff involved in service provision
Next Steps
To further the quality of this study, continued qualitative feedback from parents/carers, patients and staff, needs to be obtained about this service. In addition, quantitative assessment of the effectiveness of the programme in terms of resource use verses cost, needs to be analysed. Including, an assessment of the cost for the patients/parents attending the joint clinic service, compared to other clinic attendances could be quantified. As it would be interesting to directly compare the feedback and practical costs from the joint service verses other independent clinic services within the hospital, to see if both patients and staff find the multidisciplinary setup significantly beneficial. In terms of patient care, an analysis of morbidity and mortality associated with routine MLTB examinations could be compared from previous years which conducted assessments under general anaesthetic, to quantify the risk reduction associated with changing to clinic examinations under local anaesthetic. Finally, a comparison of the effectiveness of the joint complex airway clinic service provided at Alder Hey Children’s Hospital with the setup of other tertiary healthcare systems, could help develop and advance the potential of the service both locally and beyond.
Conclusion
The multidisciplinary joint complex airway clinic provides a platform for both ENT and respiratory teams to examine patients and come up with a shared strategy between themselves and patients/ parents/carers for long-term tracheostomy management. Overall, parental/carer feedback revealed a positive opinion concerning the clinic’s setup and a common feeling that their understanding and confidence levels in regard to their children’s complex airways improved after attending the clinic. Finally, the clinic service minimised the need for annual diagnostic MLTBs under general anaesthesia. Thereby, reducing the potential morbidity associated with repeat anaesthetic procedures.
References
- Watters KF (2017) Tracheostomy in Infants and Children. Respiratory Care 62(6): 799-825.
- McPherson ML, Shekerdemian L, Goldsworthy M, et al. (2017) A decade of paediatric tracheostomies: Indications, outcomes, and long-term prognosis. Paediatric Pulmonology 52(7): 946-953.
- Douglas CM, Poole-Cowley J, Morrissey S (2015) Paediatric tracheostomy -An 11-year experience at a Scottish paediatric tertiary centre. International Journal of Paediatric Otorhinolaryngology 79(10): 1673-1676.
- Carron JD, Derkay CS, Strope GL (2000) Paediatric tracheotomies: Changing indications and outcomes. Laryngoscope 110(7): 1099-1104.
- Liu C, Heffernan C, Saluja S (2014) Indications, Hospital Course, and Complexity of Patient’s Undergoing Tracheostomy at a Tertiary Care Paediatric Hospital. Otolaryngology Head and Neck Surgery 151(2): 232-239.
- Abode KA, Drake AF, Zdanski CJ (2016) A Multidisciplinary Children’s airway centre: Impact on the care of patients with tracheostomy. Pediatrics 137(2): e20150455.
- De Mestral C, Iqbal S, Fong N, et al. (2011) Impact of a specialized multidisciplinary tracheostomy team on tracheostomy care in critically ill patients. Canadian Journal of Surgery 54(3): 167-172.
- Berry JG, Goldmann DA, Mandl KD (2011) Health information management and perceptions of the quality of care for children with tracheotomy: a qualitative study. BMC Health Service Research 23(11): 117.
- Funamura JL, Durbin-Johnson B, Tollefson TT (2014) Paediatric tracheotomy: Indications and decannulation outcomes. Laryngoscope 124(8): 1952-1958.
- Yaneza MMC, Janes HP, Davies P (2015) Changing indications for paediatric tracheostomy and the role of a multidisciplinary tracheostomy clinic. The journal of laryngology & Otology 129(9): 882-886.
- McClure RJ, Newell SJ, Edwards S (1996) Patient characteristics affecting attendance at general outpatient clinics. Archives of Disease in Childhood 74: 121-125.
- Lerwick JL (2016) Minimizing paediatric healthcare-induced anxiety and trauma. World Journal of Clinical Paediatrics 5(2): 143-150.
- Pandian V, Miller CR, Mirski MA (2012) Multidisciplinary Team Approach in the Management of Tracheostomy Patients. American Academy Otolaryngology -Head and Neck Surgery 147(4): 684-691.
- Cohen MM, Cameron CB, Duncan PG (1990) Paediatric anaesthesia morbidity and mortality in the perioperative period. Anaesthetic and Analgesia70(2): 160-167.
- Kain ZN, Wang SM, Mayes LC (1999) Distress During the Induction of Anaesthesia and Post-operative behavioural Outcomes. Anaesthesia & Analgesia 88(5): 1042-1047.
- Kain ZN, Mayes LC, O’Connor TZ (1996) Preoperative anxiety in children, Predictors and outcomes. Archives of Paediatric & Adolescent Medicine 18(2): 651-658.
- Hartnick C, Diercks G, De Guzman V (2017) A quality study of familycentred care coordination to improve care for children undergoing tracheostomy and quality of life for the caregivers. International Journal of Paediatric Otorhinolaryngology 99: 107-110.
- McGrath BA, Lynch J, Bonvento B (2017) Evaluating the quality improvement impact of the global tracheostomy collaborative in four diverse NHS hospitals. BMJ Quality Improvement Reports 6(1): pii.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




