
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Mini Review(ISSN: 2637-4544) 
New Insight into Pregnant Women Oral Health Cares Volume 1 - Issue 4
Hassan H Koshak*
- Department of Dental, Consultant in Periodontics and Implant Dentistry, Kingdom of Saudi Arabia
Received: March 10, 2018; Published: March 14, 2018
Corresponding author: Hassan H Koshak, Department of Dental, Consultant in Periodontics and Implant Dentistry, Head of the Dental Department and Dental Educator, Director of Academic and Education Affairs at Comprehensive Specialized Polyclinic, Ministry of Interior Security Forces Medical Services, Jeddah, Kingdom of Saudi Arabia
DOI: 10.32474/IGWHC.2018.01.000118
Abstract
The human body is comprised of complex systems, which are interconnected with each other. Because of the way, the human body is made; one organ of the body can have an impact on other organs of it. Oral health affects people physically and psychologically and influences how they grow, enjoy life, look, speak, chew, taste food and socialize, as well as their feelings of social well-being. The oral hygiene measures related to professional level, level of education, and periodontal maintenance. Some studies report that oral health has an impact on food choice and on the intake of key nutrients, causing various nutritional problems. Recent researches on oral and general health have shown a link between the two. With more than 90% of systemic diseases having oral symptoms. These symptoms can include swollen gums, sores, ulcers, dry mouth and more, the following diseases are an example of a systemic disease which has symptoms expressed in the mouth like diabetes, leukemia, oral cancer, pancreatic cancer, heart disease and kidney disease.
Research has also shown that poor dental hygiene and gum disease can directly increase the risk of heart disease, heart attack, diabetes, dementia, rheumatoid arthritis and even stroke. Women with poor dental health have also shown higher rates of preterm and low-birth-weight children. To prevent these health issues, practicing good oral hygiene is very important. Pregnant woman should get into good practices. Regular dental visits, brushing regularly, flossing and watching what they eat are all important steps in preventing dental diseases and keeping them in good health
Introduction
Oral health is multifaceted and includes the ability to speak, taste, touch, chew, swallow, and convey a range of emotions through facial expressions with confidence and without pain, discomfort, and disease of the craniofacial complex [1]. A healthy mouth is one that is free of pain and infection, with no untreated tooth decay, and with pink gum tissues that do not bleed on brushing. The mouth should be moist, with no evidence of lumps, ulcers or unusual color on or under the tongue, cheeks or gums [2]. Pregnancy is a state of physiological condition that brings about various changes in the oral cavity along with other physiological changes taking place throughout the female body [3].
What oral problems might develop during pregnancy?
Studies show that many pregnant women experience pregnancy gingivitis when dental plaque builds up on the teeth and irritates the gums. Symptoms include red, inflamed and bleeding gums [4].
Pregnancy gingivitis occurs more frequently during pregnancy because the increased level of hormones exaggerates the way gums react to the irritants in plaque. However, it's still plaque not hormones that is the major cause of gingivitis [5,6]. Keeping the teeth clean, especially near the gum line, will help dramatically reduce or even prevent gingivitis during pregnancy. And substituting sweets with more wholesome foods such as cheese, fresh fruits or vegetables is better for good oral health [7] Figure 1.
On the other hand
It is possible for bacteria that originate in the mouth (for example from decayed teeth or periodontitis patient) to get into the bloodstream and so to other parts of the body including the cardiovascular network where they can cause serious infections [8]. Bacteria-induced activation of cell-mediated immunity leading to cytokine production and the synthesis and release of prostaglandins, growth factors, cytokines, interleukin-1 (IL- 1), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNF-α), matrix metalloproteinase have been found in the amniotic fluid of patients in preterm labor with amniotic fluid infection and other potent cytokines, which may directly or indirectly interfere with premature rupture of membranes or fetal growth and delivery [5]. Oral pathogens release toxins that reach the human placenta via the mother's blood circulation and interfere with fetal, also prompt accelerated production of inflammatory mediators PGE2 and TNF that normally build to a threshold level throughout pregnancy, and then cue the onset of labor, growth and development [8].
Figure 1:
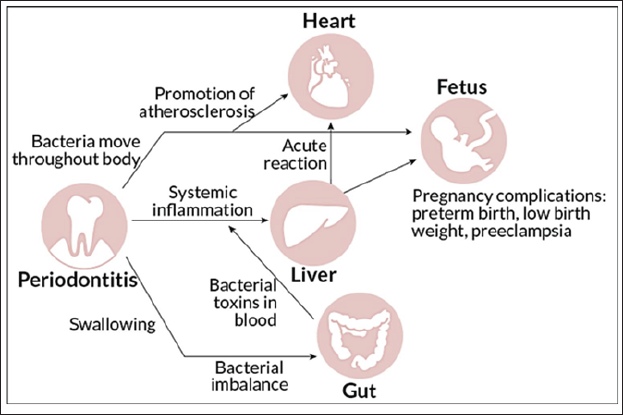
The biological mechanisms involve bacterially induced activation of cell-mediated immunity leading to cytokine production and the ensuing synthesis and release of PG, which appears to trigger preterm labor [4]. Elevated levels of cytokines (IL-1, IL-6, and TNF-α) have been found in the amniotic fluid of patients in preterm labor with amniotic fluid infection [8].
These cytokines are all potent inducers of both PG synthesis and labor [4]. Intra-amniotic levels of PGE2 and TNF-arise steadily throughout pregnancy until a critical threshold is reached to induce labor, cervical dilation, and delivery [5]. The elevated levels of these inflammatory mediators trigger premature delivery [4].
Who needs oral care?
Both pregnant or ether non-pregnant woman will need good oral care [8].
Recommended care for maintaining healthy natural teeth:1- Brush morning and night with fluoride toothpaste it is important to use fluoride toothpaste. The fluoride helps prevent tooth decay by binding with tooth enamel to repair the early stages of decay [2]. Only a pea-sized amount of fluoride toothpaste should be used for brushing. Use a soft bristled toothbrush to clean teeth, gums and tongue. The best brushes are ones with a smaller head and soft bristles [3].
A. If the care plan requires cleaning between teeth then consider using inter-dental brush, dental floss, or water floss that will be discussed later [2].
B. Flossing - removes tartar that collects at the gum line.
C. Rinsing - removes dislodged food particles and excessive toothpaste. Rinsing can also freshen breath, prevent or control tooth decay, and prevent or reduce gingivitis.
D. Mouthwash it should be used as a supplement when suggested by a dentist. A mouthwash does not replace the need for brushing with fluoride toothpaste [8].
E. Encourage consumption of sugar-free food and drinks between meals.
F. Ensure regular professional checkups and cleaning during periods of pregnancy [6].
G. Water flosser during the millennium period, the greater awareness of the need for effective alternatives to string floss began to emerge.
Results of studies found that the water flosser reduced the traditional clinical measures of plaque biofilm, bleeding, and gingivitis as well as modulated the cytokine profile. The effect on the inflammatory mediators was considered a modulation versus a reduction because the water flosser reduced the pro-inflammatory cytokines, IL-1ß and prostaglandin (PGE2) but increased the anti-inflammatory mediator interleukin-10 (IL-10), a blocker of IL-1ß, andγ),interferonacy to kinegammakeyin (INF killing bacteria [9].
In 2005, the first study that compared the water flosser to string floss was conducted at the University of Nebraska. In a 28 day RCT, a water flosser was paired with a manual or a power toothbrush and both were compared to manual toothbrush and string floss. The findings demonstrated that regardless of toothbrush type, the addition of the water flosser, once daily with plain water, to either a manual or power brush was an effective alternative to string floss for the reduction of bleeding, gingivitis, and plaque biofilm. It provided superior results in reducing inflammation with the Water Flosser being up to 93% better at reducing bleeding and up to 52% better at reducing gingival inflammation over string floss. Significant improvements in oral health occurred regardless of toothbrush type, so it was deemed likely that many patients currently using a power toothbrush may get further improvements in oral health by the addition of a water flosser [9]. Water Flosser users also had an 85% reduction in bleeding from baseline, which was 26% better than string floss and 53% better than tooth brushing alone [9].
Recommended care for maintaining dental implants:(Sylvia et al 2012) classified periimplant tissues as the following:
a) Healthy: If there are no clinical signs of inflammation, the patient's implants are classified as healthy.
b) Implant Mucositis: Is a localized inflammatory lesion within the soft tissue, without progressive bone loss, apart from the original 0.2-2mm cratering that occurs shortly after abutment connection around some osseointegrated implants. Mucositis may be identified clinically by redness and bleeding on gentle probing (pressure < 0.15N).
c) Peri-implantitis: Is characterized by a localized inflammatory lesion that incorporates bone loss around an osseointegrated implant. In cases of peri-implantitis, the mucosal lesion is often associated with suppuration or deepening of the clinical probing depths and is always accompanied by bleeding on probing and loss of supporting marginal bone beyond the original bone loss.
d) Even though dental implants may accumulate less bacterial plaque than natural teeth, effective daily plaque control in pregnant woman is essential to maintain health and stability of both hard and soft implant supporting tissues [9].
Sylvia mentioned the Home care devices and aids that have been shown to be safe for use around implant surfaces include interdental brushes with nylon-coated core wire, soft toothbrushes (both manual and power), end-tuft brushes, gauze, many types of floss (e.g., plastic, braided nylon, coated, floss with stiffened end to clean under bridges, dental tape, Postcare implant flossing aid, stannous fluoride gel and Chlorhexidine) [9].
Plaque control for single implants can be accomplished with a toothbrush and dental floss: numerous studies have suggested that powered toothbrushes may be more effective than manual toothbrush. For implant supported fixed partial or complete dentures: floss threads or interdental brushes are effective in controlling interproximal plaque accumulation [10].
As with natural teeth, brushing and flossing are effective in disrupting supragingival plaque but have limited benefit in subgingival areas. Oral irrigation devices, particularly those with tips designed to penetrate the sulcus, have been shown to reduce the bacterial levels in periodontal pockets. Based on the evidence from periodontitis reports, dilute sodium hypochlorite may be the most effective antimicrobial irrigant for home use [10].
Conclusion
Oral care during pregnancy is very important and involves the contribution of the patient herself, dental professionals and physicians. Pregnant patients must be educated about the importance of maintaining good oral hygiene, expected changes in the oral cavity and routine dental visits.
References
- George A, Johnson M, Blinkhorn A, Ellis S, Bhole S, et al. (2010) Promoting oral health during pregnancy: current evidence and implications for Australian midwives. J Clin Nurs 19(23-24): 3324-3333.
- Ullah R, Zafar MS (2015) Oral and dental delivery of fluoride: a review. Fluoride 48(3): 195-204.
- Zafar MS, Ahmed N (2015) Therapeutic roles of fluoride released from restorative dental materials. Fluoride 48(3): 184-194.
- Trivedi S, Lal N, Singhal R (2015) Periodontal diseases and pregnancy. J Orofacial Sci 7: 67.
- Tarsitano BF, Rollings RE (1993) The pregnant dental patient: evaluation and management. Gen Dent 41(3): 226-234.
- Hemalatha V, Manigandan T, Sarumathi T, Aarthi Nisha V, Amudhan A (2013) Dental considerations in pregnancy a critical review on the oral care. J Clin Diagn Res 7(5): 948-953.
- Ito S (2000) Drug therapy for breast-feeding women. N Engl J Med 343: 118-126.
- Michalowicz BS, DiAngelis AJ, Novak MJ, Buchanan W, Papapanou PN, et al. Examining the safety of dental treatment in pregnant women. J Am Dent Assoc 139: 685-695.
- Sylvia Todescan (2012) Guidance for the Maintenance Care of Dental Implants: Clinical Review. J Can Dent Assoc 78: c107.
- Oral Health Care During Pregnancy Expert Workgroup (2012) Oral Health Care During Pregnancy: A National Consensus Statement . Washington, DC: National Maternal and Child Oral Health Resource Center.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...















