
Lupine Publishers Group
Lupine Publishers
ISSN: 2644-1217
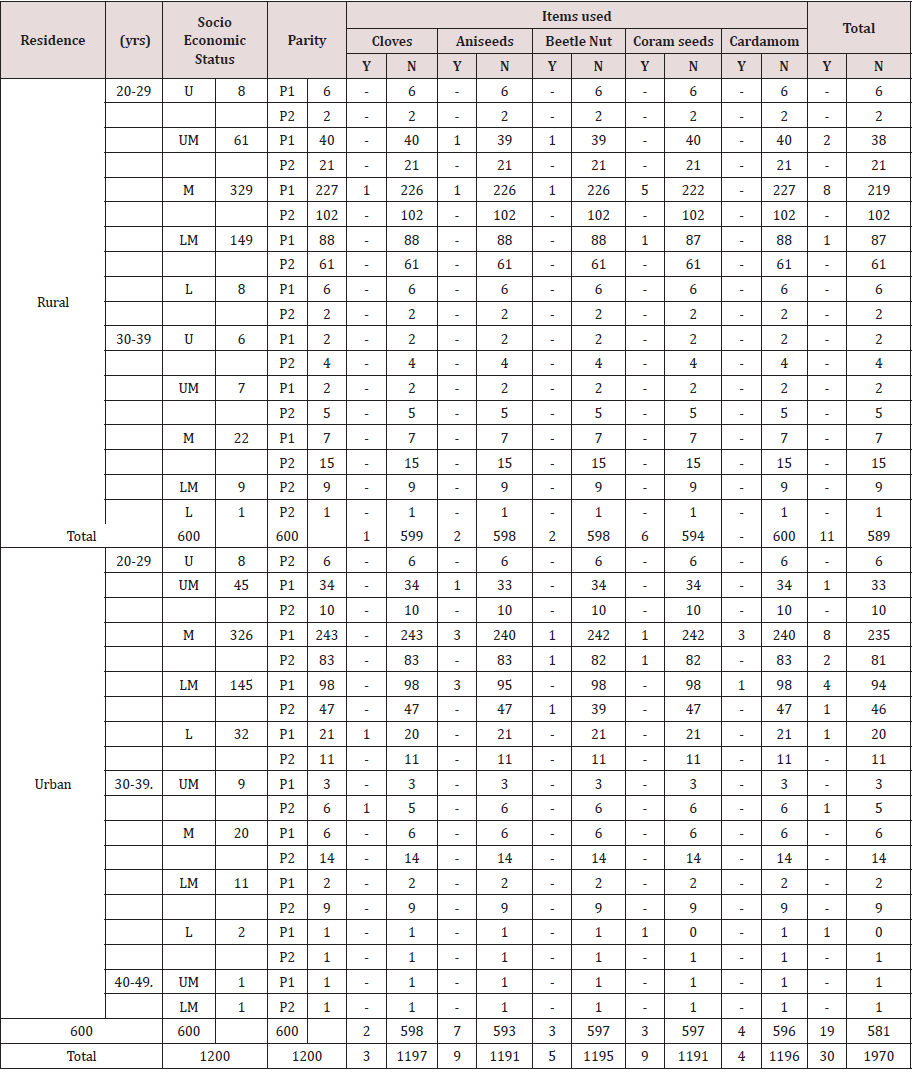
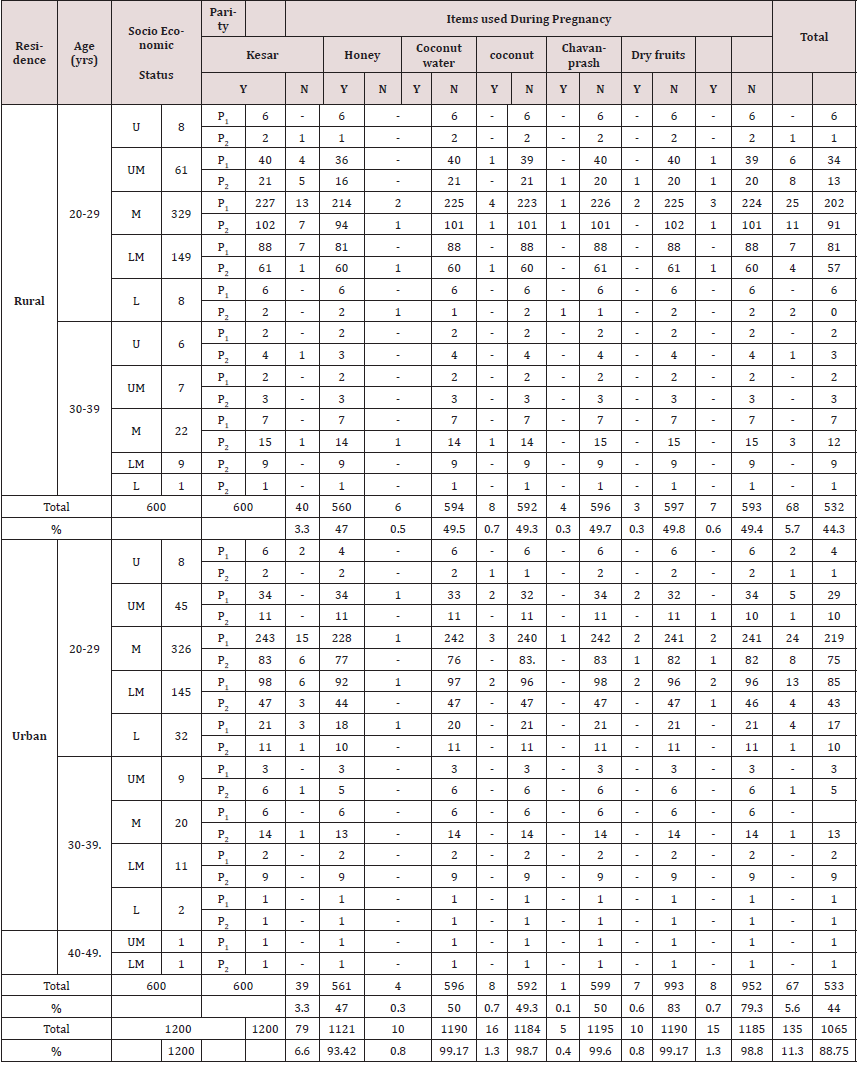
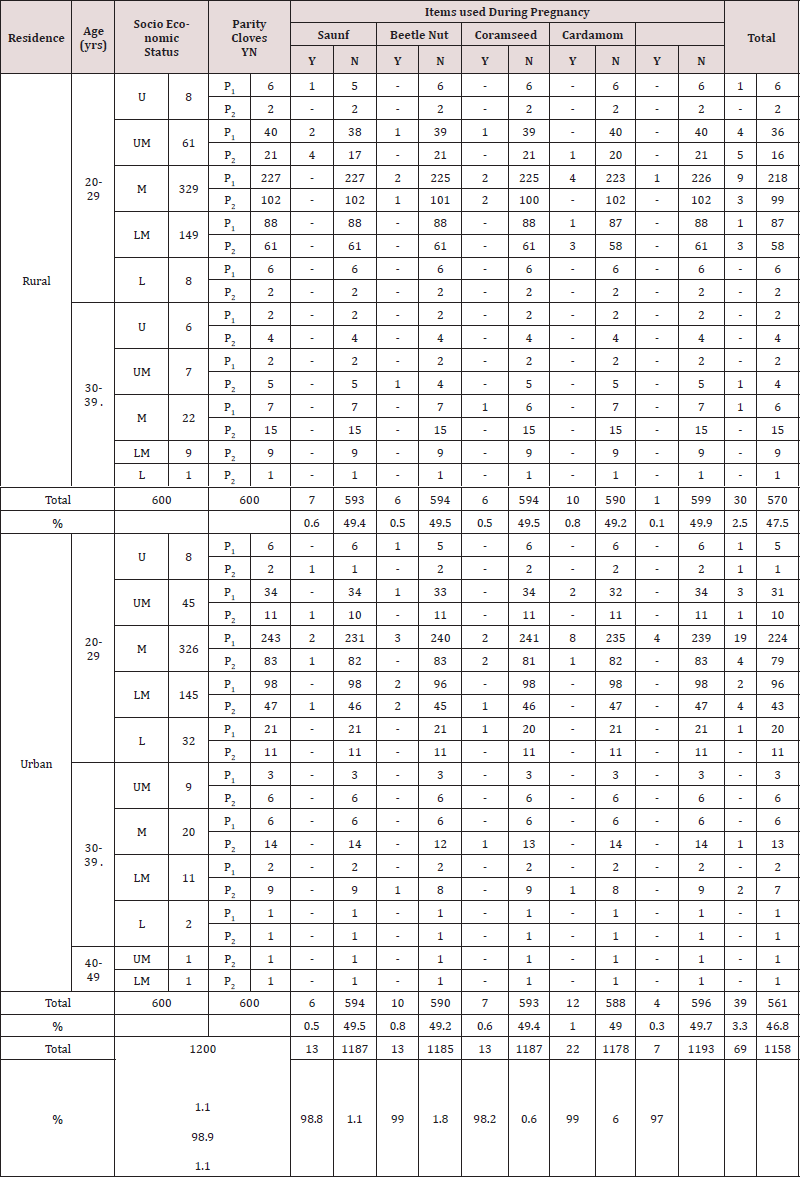
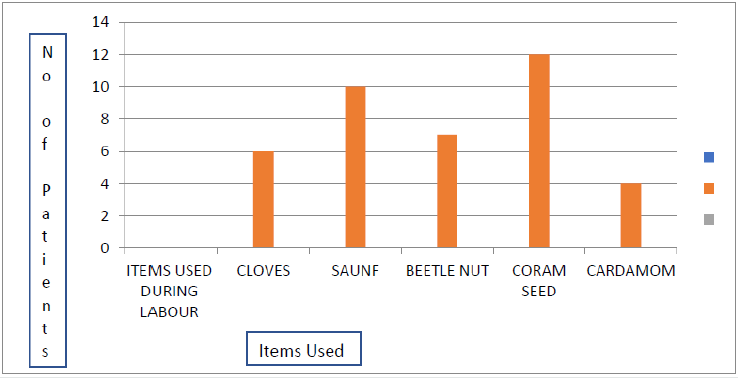
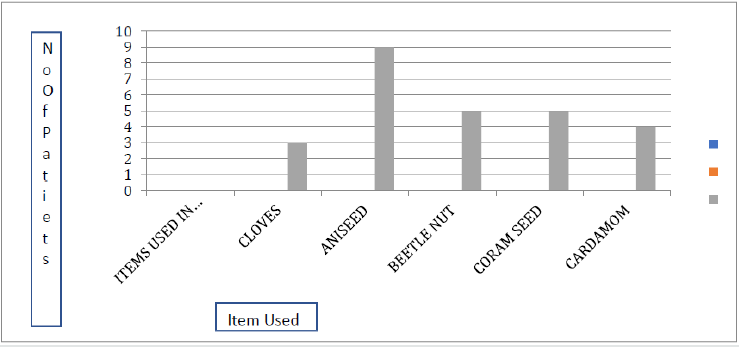
During labour the CIs used were Cloves, Saunf, Beetle Nut, Coram Seeds and Cardamom by 2.5% rural women and 3.3% urban. Most of those who consumed CIs were of middle class and of 20-29yrs. Overall nearly 6% laboring women used CIs. They did not inform about CIs to any health provider. The reasons given were that medication given in the hospital did not completely resolve the labour related ailments and CIs provided a more natural and faster relief. They said the usage of CIs increased the chances of natural birth and decreased the pain during delivery. Coram seeds were used by 1.6% women. CIs were used by 2.5% women in postpartum period. Common items used in post-partum were Cloves, Beetle nut, Ani seeds, Coram seeds, and Cardamom. Aniseeds and Coram seeds were used by 0.75%, Beetle nut by 0.4%. Women used CIs for preventing postpartum depression, mood elevation and improving lactation (Table 5).
Table 5: Complimentary Therapy in Postpartum period.
U- Upper UM – Upper Middle M- Middle LM – Lower Middle L- Lower
P0- P1 P2- Parity
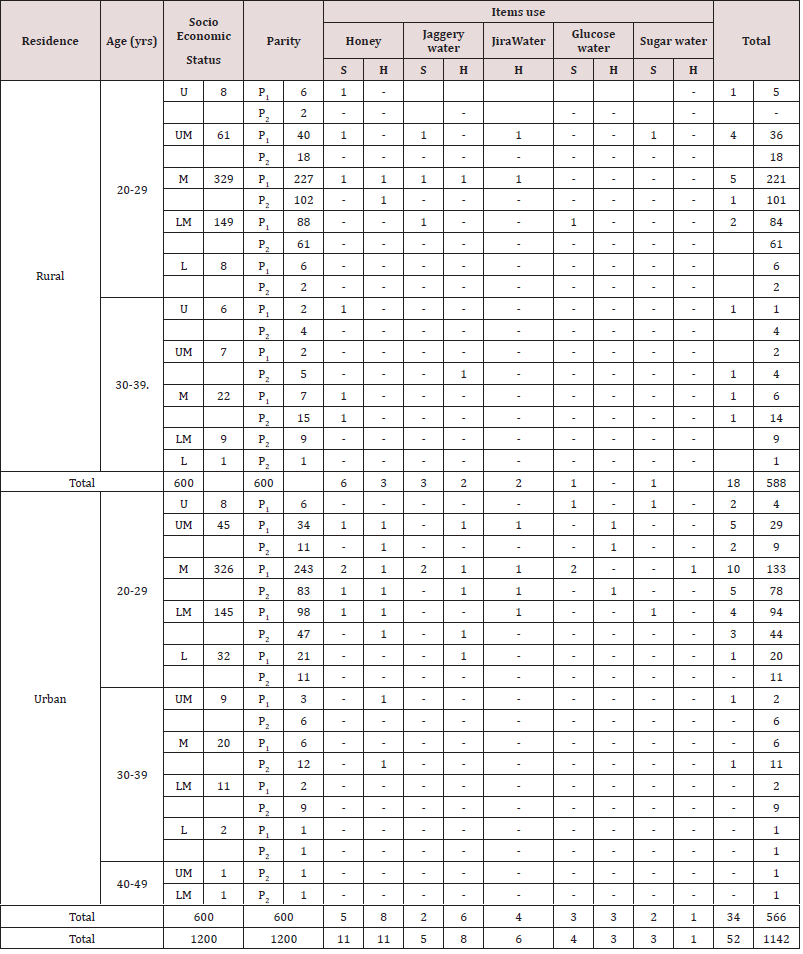
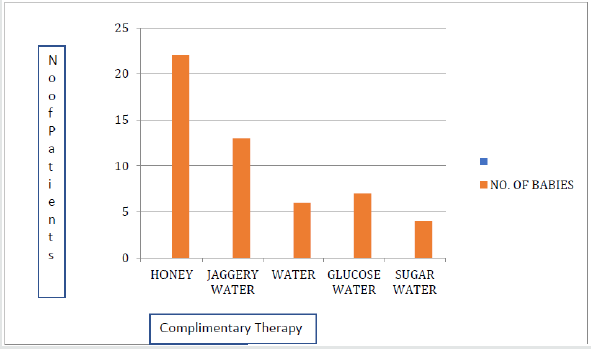
CIs like. Honey, Jaggery water, Jira water, Glucose water and Sugar water were also given to the babies. Over all 4.3% women gave CIs to their babies. Mostly Honey and jira water. with no difference in rural or urban women. Over all 4% women gave CIs to babies, Honey or Sugar in water, by 1.8% followed by Jaggery. It was revealed that more urban women, 34 (5.6%) used CIs for baby compared to rural women 18 (3%). CTs for baby were considered a source of energy to the newborn as well as were believed to boost the immunity of the newborn in conjunction with breastfeeding (Table 6). Tradition of massage was almost universal, legs and back during pregnancy and all over the body in postpartum, and to the baby too. This was irrespective of economic status or education.
Table 6: Complimentary Therapy Given to Baby.
U- Upper UM – Upper Middle M- Middle LM – Lower Middle L- Lower
P0- P1 P2- Parity S – Strong H - Healthy
Discussion
AT, TT, CTs and CIs encompass a broad spectrum of beliefs and practices used for treating or preventing various disorders and also for health promotion. Such CTs or CIs are believed to be used by pregnant women, for better growth of the baby or treating minor aliments or smooth birth process and may be women or their families had other notions Tiran [11] also opined that CTs may not be entirely free of risk. Still the use of TTs or ATs, CTs has become increasingly common in developed countries too, with women being the most frequent users. After review of various studies about CTs for perinatal depression. Sparling [12] reported that adequately powered systematic studies were necessary for knowing the role of ATs/CTs in the treatment of perinatal depression. Researchers reported that the estimates varied widely from 1% to 87%, but the general trend indicated that a significant number of pregnant women used CTs. Common modalities used included Massage, Herbal medicine, Relaxation therapies and Aromatherapy. Reasons for use varied and included the belief that these therapies offered safe alternative to pharmaceuticals and had better efficacy. They allowed greater choice and control over the childbearing experiences, In the present study when the usage of CIs/CTs was studied it was found that women of 20-29 years of age used these therapies the most. Body massage was universal. Women used CTs/CI for relief from anxiety during pregnancy and delivery and used them for a smoother delivery process and better outcome No difference was found with education or economic status. Most of the women using CTs had studied upto secondary school. Most of the women were housewives.
Truijens et al. [13] reported that many women were habitual users of such items in daily life. So, they continued using them even in pregnancy and delivery with the belief that CTs/CIs prepared the body better for pregnancy and labor. It was found that CIs were used more often in labor by primigravidae. This could be due to anxiety about the birthing experience with a lower threshold for tolerance of minor ailments, pain and desire of better birthing experience. And also, women listened to whatever was told by the family. Most expectant women used CIs on advice of family and friends, and they did not disclose use of CIs to their care providers. Skouteris [14] in his study, reported that half the Australian women surveyed consulted ATs practitioner for pregnancy related health conditions. It was quite common for women to consult multiple AT practitioners alongside their conventional maternity care providers. If a woman consulted a AT practitioner and conventional care provider simultaneously for the management of the same condition, without disclosing use of ATs to either practitioner, this could creat risk for mother or baby or both through possible pharmacological interactions between treatments or broader conflicts between the treatment goals of the two (or more). Bridee [15] reported that CTs use among pregnancy similar to non-pregnant, while during postpartum CTs use decreased., only 7.6% of women did not take any medicinal product throughout pregnancy. In various studies done for CTs results varied because they were affected by a number of factors. Health professionals of modern medicine needed to ask women about use of ATs or TTs CTs. Women may choose AT or CTs in pregnancy to have control over growth of baby and hence perceived as safer treatment option in pregnancy and childbirth or to select a treatment choice not covered by conventional medicine to prepare the womb and cervix for childbirth.
In the study by Jung et. al [16,17] the proposition of CT user among pregnant women was relatively high. Health providers, while respecting the beliefs of communities, needed to find means of best advocacy for safe practices. Knowledge of ATs/TTs, CTs CIs needed to be part of everyday clinical practice for the practitioners of modern medicine. They needed to promote beneficial practices and discourage the harmful modalities, for which research is essential. Awareness needs to be created in a sensitive way and also make health providers aware of existing ATs, TTs and CIs. Study by Hollyer [18] revealed a generalized lack of knowledge and poor understanding of the possible risks to women. and researcher reported that women’s holistic needs may not be met within a medical model of maternity care So CTs have a place. Many pregnant women who used CTs did not know whether they did good or bad to the mother and/ or the baby. The lack of awareness could lead to serious hazards in the mother and /or the baby. Massage and Aromatherapy were used for treating anxiety, Acupressure for back and pelvic pain and Acupressure, and ginger for morning sickness is known.
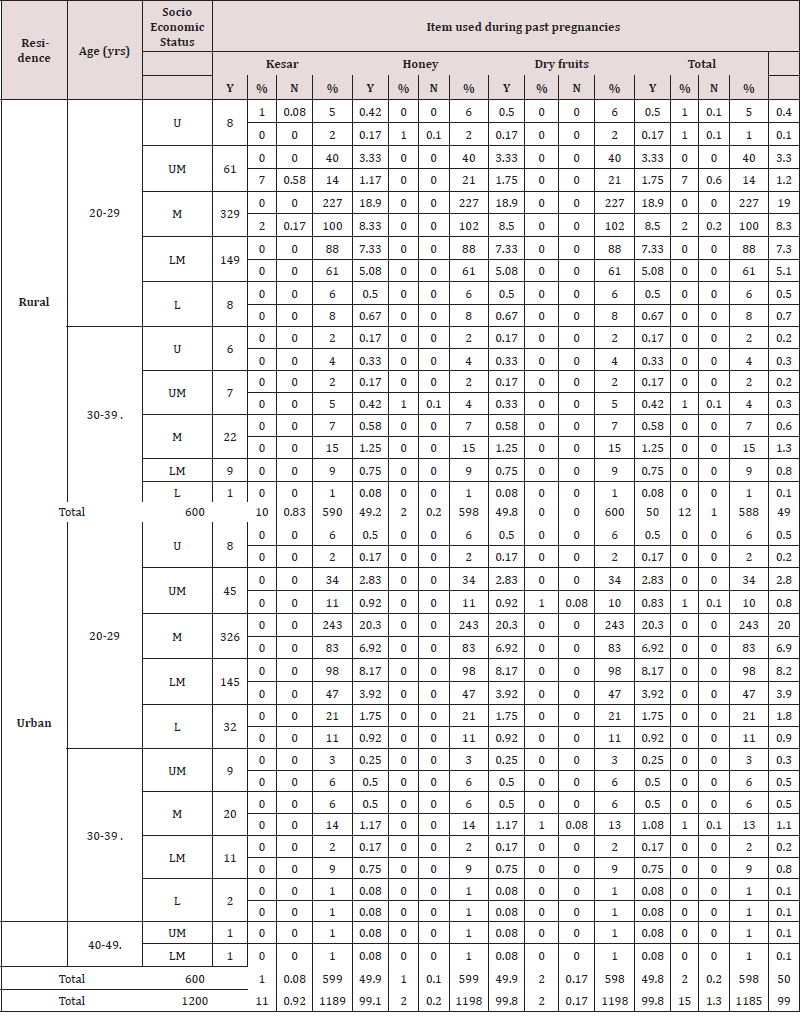
In the present study in past pregnancy less women had taken traditional medicine and Low Dog [19] reported that they had lack of knowledge of these products and hesitated because the safety of these products was not known. The women felt that they could have better control of pregnancy and improved growth of the baby. In general, CTs are increasingly being integrated into maternity care [20]. Use of Herbal and other natural treatments have been reported to be increasing in the United States and Canada, also as valid treatments [21]. Because Herbal and other natural remedies were not regulated to the same degree as traditional pharmaceutical products, use in pregnancy a potentially vulnerable time for both mother and fetus, so monitoring such things was thought to be essential [22]. Kesar and Carom seed use in pregnancy as per their traditional belief, cleaned the stomach and helped in reducing vomiting and indigestion. During post-partum period it increased the energy in the body and prevented infection Health and Balanve Guife [23] reported that for Nausea; Acupuncture, Acupressure, Ginger root worked well and were considered safe for pregnant women, Exercise, hypnosis and on Herbs close to the skin have been stated to be beneficial in turning a breech baby. Relaxation techniques, patterned breathing, emotional support, and selfhypnosis are already widely used CT in labor. Robust research is needed to understand their utility, benefits and concern if any. Pregnant women struggle with various health issues that can affect fetal development and normal delivery in the present study overall use was somewhat lower than expected. Conovar [24] from a single, urban hospital found that, 4.1% of women reported using an Her
During labour Coram seeds were consumed by women with the beliefs that the conventional medications did not cover all the ailments and CI provided better and faster relief of symptoms. Moreover, they prepared the uterus and cervix for a better birthing experience and increased the chances of natural birth. Women reported CIs improved lactation and specially in prim para lowered the chances of postpartum depression, elevated mood and symptomatically treated minor ailments. For the baby honey was the commonest CI given. According to Pallivalappila et al. [25] the application of a consistent and useable CTs definition proved to be a major issue. However, what is used, why is used are not well known. There are very few high-quality studies about the effectiveness CTs or ATs and more studies are needed. Studies should focus on the safety of specific with respect to wide range of pregnancy conditions and outcomes. Indeed, whether or not a particular therapy is deemed to be CTs may differ between countries, healthcare settings, and specialities. The lack of definitions and checklists may explain why the reported prevalence of CTS use appears to be highly variable, even within similar populations. However, what is used, why is used are not well known. Research is needed.
Conclusion
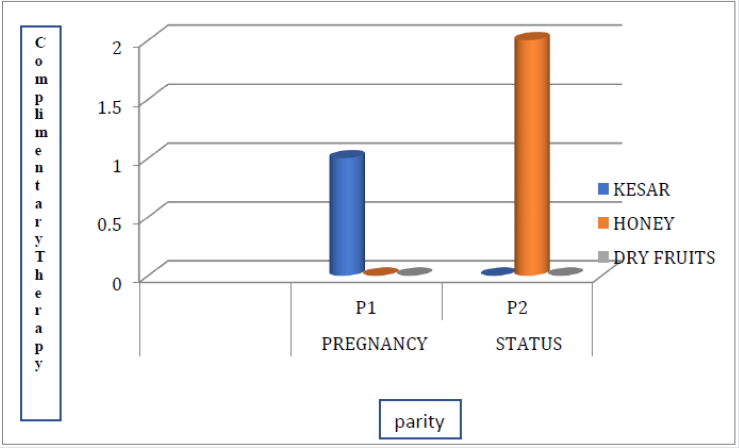
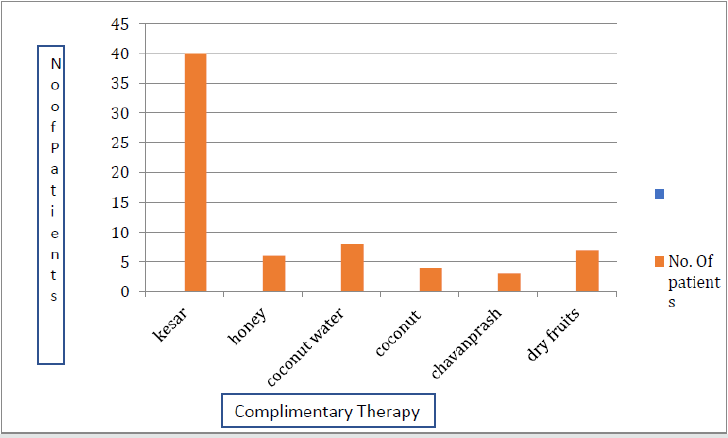
Community based research is needed to gain a greater understanding of the true use of AT, TT, CTs, CIs by pregnant women. Health professionals should ask women about use. It is essential to know what they use during pregnancy, labour and after delivery. Further evaluation of CTs among pregnant and postpartum women is necessary to determine the costs and benefits of integrative TTs in conventional care. Larger studies are needed for better understanding of the role of CTs in pregnancy (Graph 1-5).
References
- MacLennan, Alastair H, David H Wilson, Anne W Taylor (1996) Prevalence and cost of alternative medicine in Australia. The Lancet 347(9001): 569-573.
- Brevoort P (1998) The booming U.S. botanical market: A new overview. HerbalGram 44: 33-48.
- Eisenberg DM, Davis RB, Ettner SL, Apple S, Wilkey S, et al. (1999) Trends in Alternative Medicine Use in the United States, 1990-1997:results of a follow-up national survey. JAMA 280(18):1569-1575. doi :10.1001JAMA 280.18.1569.
- Ernst E (2000) The role of complementary and alternative medicine. BMJ321(7269): 1133-1135. doi:10.1136/bmj.321.7269.1133.
- Hepner DL, Harnett M, Segal S, Camann W, Bader AM, et al. (2002) Herbal Medicine Use in Parturients.AnesthAnalg 94(3):690-693.
- Jeffrey d Quinlan, Florida d Ashley Hill (2003) Nausea and Vomiting of Pregnancy.Am Fam Physician. 68(1):121-128.
- Jon Adams, Chi-Wai Lui, David Sibbritt, Alex Broom, Jon Wardle, et al. (2009) Women’s use of complementary and alternative medicine during pregnancy: a critical review of the literature. Birth 36(3):237-245.
- Hall HG, Griffiths DL, McKenna LG (2011) The use of complementary and alternative medicine by pregnant women: a literature review. Midwifery 27(6):817-824.
- Steel A, Adams J, Sibbritt D (2012) Complementary and alternative medicine in pregnancy: a systematic review. Journal of the Australian Traditional-Medicine Society 17(4): 205-209.
- Pinn G, Pallett L (2002) Herbal medicine in pregnancy. Complementary Therapies in Nursing and Midwifery8(2): 77-80.
- Tiran D (2001) Complementary strategies in antenatal care. Complementary Therapies in Nursing and Midwifery 7(1): 19-24.
- Deligiannidis, Kristina M, Nancy Byatt, Marlene P Freeman (2014) Pharmacotherapy for mood disorders in pregnancy: a review of pharmacokinetic changes and clinical recommendations for therapeutic drug monitoring. J of clin psychopharmacol 34(2): 244-245.
- Skouteris H, Wertheim EH, Rallis S, Paxton SJ, Kelly L, et al. (2008) Use of complementary and alternative medicines by a sample of Australian women during pregnancy. Aust N Z J Obstet Gynaecol48(4): 384-390.
- BirdeeGurjeet S, Kemper Kathi J, Rothman Russell, Gardiner Paula (2014) Journal of Women's Health. 23(10): 824-829. https://doi.org/10.1089/jwh.2013.4568.
- Headley J, Northstone K, Simmons H, Golding J (2004) Medication use during pregnancy: data from the Avon Longitudinal Study of Parents and Children. Eur J Clin Pharmacol 60(5): 355-361.
- Bishop JL, Northstone K, Green JR, Thompson EA (2011) 19(6):303-10. doi: 10.1016/j.ctim.2011.08.005.
- Jung JK (2016) inventor; Samsung Electronics Co Ltd, assignee. Display screen or portion thereof with graphical user interface. United States patent application US 29/495,796.
- Hollyer T, Boon H, Georgousis A, Smith M, Einarson A (2002) The use of CAM by women suffering from nausea and vomiting during pregnancy. BMC Complement Altern Med 2:5.
- Ernst E (2002) Herbal medicinal products during pregnancy: are they safe.BJOG109(3): 227-235.
- Low Dog T (2009) The use of botanicals during pregnancy and lactation. Altern Ther Health Med 15(1): 54-58.
- Ranzini A, Allen A, LaiY (2001) Use of complementary medicines and therapies among obstetric patients. Obstetrics & Gynecology. 97(4Suppl 1): pS46.
- Smith CA, Cochrane S (2009) Does acupuncture have a place as an adjunct treatment during pregnancy? A review of randomized controlled trials and systematic reviews. Birth (Berkeley, CA) 36: 246-253.
- Allaire A,Wells’ S (2000) Complementary and alternative medicine in pregnancy: a survey of North Carolina certified nurse-midwives. Obstetrics & Gynecology 95:19-23.
- Conover EA (2003) Herbal agents and over-the-counter medications in pregnancy. Best Practice & Research, Clinical Endocrinology & Metabolism 17: 237-251.
- Abdul RoufPallivalappila, Derek Stewart, Ashalatha Shetty, BinitaPande, James S McLay(2013) Complementary and Alternative Medicines Use during Pregnancy: A Systematic Review of Pregnant Women and Healthcare Professional Views and Experiences Evid Based Complement Alternat Meddoi: 10.1155/2013/205639.















.png)
.jpg)

